- Submissions

Full Text
Novel Research in Sciences
Presentation of Covid 19 Patients with and without Diabetes
Arzu Gunturk, Abidin Yusuf Kavurmaci*, Ferda Kartufan, Hanife Esra Gumus, Adnan Ezici, Pinar Çiragil, Sibel Bolukcu, Yasar Kucukardali and Hanife Esra Gumus
Department of Internal Medicine, Yeditepe University Hospital, Turkey
*Corresponding author:Abidin Yusuf Kavurmaci, Department of Internal Medicine, Yeditepe University Hospital, Turkey
Submission: March 1, 2021;Published: April 15, 2021
.jpg)
Volume7 Issue2April, 2021
Abstract
The presence of diabetes mellitus is one of the critical risk factors for covid 19. In this study, laboratory values and outcomes of symptoms of diabetic and non-diabetic patients were compared retrospectively. One hundred ten patients (90 nondiabetics, 20 diabetics) were included in the study. The mean age was higher in the diabetic group (64 vs. 53 years) (p=0.02). Only dyspnea was higher in the diabetic group (50 vs 25%) (p=0.008). In the comparison of basal laboratory values, the number of leukocyte neutrophils, platelets, and lymphocytes was higher in the diabetic group (p<0.05). The decrease in hemoglobin and lymphocyte counts were found to be higher in the diabetic group in the follow-up of the laboratory values performed every two days (p<0.05). The length of stay in the intensive care unit was longer in diabetic patients (20 vs. 7 days) (p<0.05). There was a positive correlation between the glucose level and the number of leukocytes only (r: 0.4 p=0.009) and neutrophils (r: 0.41 p=0.07). The steroid use rate was 18% in the diabetic group and 7% in the non-diabetic group, but the difference was not statistically significant. (p>0.05). The average age of the diabetic covid patient group, the frequency of shortness of breath, the duration of intensive care stay was higher, and the decrease in lymphocytes and hemoglobin was higher.
Keywords: Diabetes; Hyperglycemia; Infections; Covid 19; Hemoglobin; Lymphocyte; Erythrocyte
Introduction
The current pandemic of SARS-CoV2 coronavirus disease 2019 (COVID-19) is a particular challenge for diabetes patients. Diabetes mellitus predisposes the disease’s severe course and doubles the COVID-19 mortality risk due to pulmonary and cardiac involvement [1]. However, diabetes mellitus is an independent predictor of admission to intensive care unit or invasive ventilation or death in COVID-19 [2]. Besides, diabetes patients often suffer from comorbidities which further worsen clinical outcomes. Glycemic control during infectious diseases is often suboptimal, and anti-diabetic drugs and insulin therapy have to be adapted accordingly. The high prevalence of diabetes makes it essential comorbidity in patients with COVID-19. Individuals with diabetes are more prone to several infections. These infections may result in less well-controlled diabetes. Multiple pathophysiological explanations can be put forward supporting the association between DM and COVID-19 severity. Numerous factors contribute to the immune dysfunction in individuals with diabetes, including hyperglycemia, neutrophil chemotaxis inhibition, altered cytokine production, phagocytic cell dysfunction, impaired T-cell mediated immune responses and ineffective microbial clearance. This review article aimed to summarize the current knowledge about the relationship between diabetes and COVID-19 and its role in these patients’ outcomes. The study aims to investigate whether there is a difference between patients with and without diabetes in terms of the initial symptoms of the disease, laboratory values, duration of hospitalization, and rates of admission to intensive care.
Material and Method
This study was conducted on 109 patients diagnosed with covid-19, hospitalized, and treated at Yeditepe University Hospital between 15 March 2020 - 30 May 2020. There is no distinction between women and men. The age range is 18-85 years. Approved was obtained Ministry of Health and University ethics committee.
Inclusion criteria
a. Correct diagnosis of covid 19
b. Medical records are sufficient
c. Hospitalization for more than 72 hours
Exclusion criteria
a. Patients other than the specified age
b. Insufficient medical report
Working groups
The group with diabetes: Having been diagnosed with diabetes at least three months before admission to the hospital.
Non-diabetes group: Patients with covid 19 infections who have not been diagnosed with overt diabetes. The parameters
compared in the study groups: Comparison of the distribution frequency of symptoms, age, and gender distribution, length of hospital and intensive care hospitalization, intensive care admission rates, baseline laboratory values, course of laboratory values and final laboratory values, comparison of treatment options used. Laboratory parameters: Hemoglobin, leukocyte, neutrophil, lymphocyte, platelet, CRP, NLR, ferritin, d - dimer, AST, LDH, BUN, creatinine, glucose, Covid 19 PCR.
Method for covid 19 PCR: Nasopharyngeal swabs were collected from each patient, Viral transfer tubes (vNAT, Bioeksen, Turkey) were employed to transfer the samples. SARS CoV-2 Double Gene RT-PCR kit (Bioeksen, Turkey) was used for RNA amplification on the Light Cycler 480plate-based RT-PCR instrument (Roche, Switzerland). The SARS-CoV-2 double gene RT-PCR kit targets the SARS-CoV-2 specific N (Nucleocapsid) and Orf1abgene regions. The human RNaseP gene is targeted for sample, nucleic acid extraction and inhibition control. The shape of the growth curves was examined, and the non-sigmoidal curves were recorded as “negative”. Sigmoidal curves with cycle threshold (Ct)<38 were evaluated as “positive”. The Ct values of all positive results were recorded.
Statistics
We retrospectively conducted 110 COVID-19 patients. In our study for statistical calculations, the SPSS program was used. Initial symptoms and laboratory tests of patients, laboratory values during the clinical course and discharge period, length of hospital stay, and duration of intensive care were compared in diabetic and non-diabetic covid patients. Demographic data Average values and percentages were used in the evaluation. A categorical Chi-square test was used in the data. Student’s T-test on parametric data, Mann- Whitney U test was used for non-parametric data. In comparison, we were examining the course of laboratory data over time. General Linear Model Repeated Measures test was used. Non- Spearman’s Rho test when looking at the correlation of parametric values used.
Results
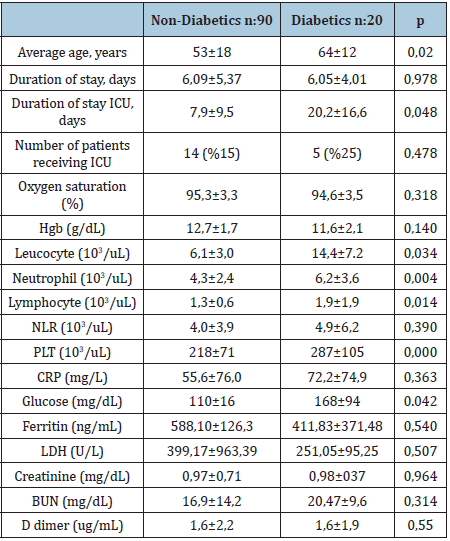
One hundred ten patients meeting their criteria were included in the study. There were 20 patients in the diabetes group and 90 patients in the non-diabetes group. The average age of the diabetes group was found to be higher (64 years vs. 53 years), and this difference was statistically significant (p 0.02). In terms of the frequency of initial symptoms, only shortness of breath was found to be higher in the diabetes group, and this difference was statistically significant 50% vs. 25%, p 0.048) (Table 1). There was a positive correlation between the glucose level and the leukocyte count (r: 0.40, p 0.009) and neutrophil count (r: 0.413, p 0.07). Length of stay in the intensive care unit of diabetic patients was found to be longer than non-diabetic patients. The mean hospitalization days of diabetic patients were found to be 20 days in intensive care and seven days for non-diabetic patients (P: 0.048). Basal leukocyte, neutrophil, lymphocyte, and platelet counts were higher in the diabetic group (Table 2).
Table 1:Distribution of initial symptoms in patients with and without diabetes.
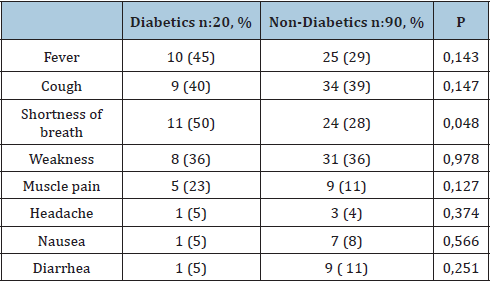
Table 2: Initial laboratory presentation of patients with and without diabetes.
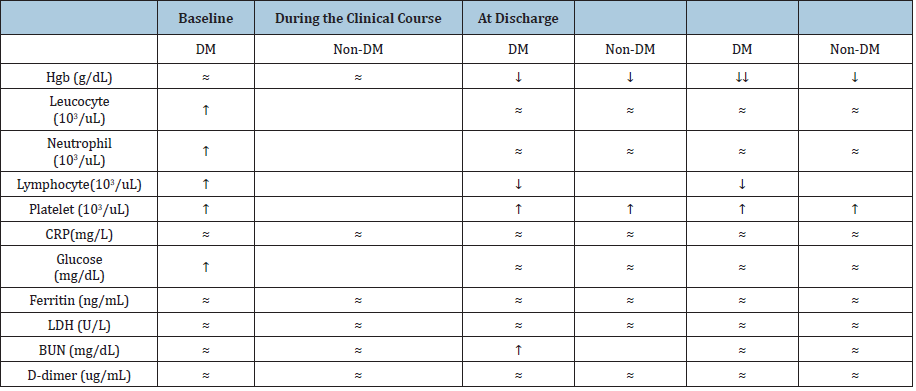
During the clinical course, did the study of laboratory values
differ in the diabetic and non-diabetic groups?
During the clinical course, there was no significant change in
leukocyte, neutrophil, CRP, ferritin LDH, creatinine values between
the groups (p>0.05). There was a significant decrease in hemoglobin
values in the clinical course (p: 0.000). The reduction was more
significant in the diabetic group (p 0.020). In the clinical course,
there was a decrease in lymphocyte count in diabetics (p=0.022).
There was a significant increase in the platelet count in the clinical
practice (p 0.000), but there was no association with diabetes (p
0.632). BUN values increased in a clinical course (p 0.026), but
the relationship with diabetes was not significant (p. 0527). When
the average values of leukocyte, neutrophil, lymphocyte, platelet,
CRP, ferritin, LDH, glucose, AST, d-dimer were examined during
discharge, no difference was observed between them (P>0.05).
There was a decrease in hemoglobin in both groups at the time
of discharge. It was observed that the decline in hemoglobin
level of the diabetic group was higher (10.3gr vs. 11.7gr). This
difference was found to be statistically significant (p:0.022. There
was a significant negative correlation between the decrease in
hemoglobin and d-dimer (r:-0.367, p 0.06). The steroid use rate was
18% in the diabetic group and 7% in the non-diabetic group. This
difference was not statistically significant (p<0.05) (Table 3).
Table 3: The status of laboratory parameters in the diabetic and non-diabetic groups at baseline, during the clinical course and at discharge.
Discussion
In our study, only shortness of breath as a symptom was seen
more in the diabetic group. In the diabetic group, it was observed
that the duration of stay in intensive care, the number of leukocytes,
neutrophils, and lymphocytes were more. It was observed that the
hemoglobin value was lower at the time of discharge. There was no
difference in terms of other symptomatology, clinical and laboratory
findings. So are people with diabetes caught in covid 19 more? Does
the disease progress more severe in those who are caught? Is the
death rate higher in people with diabetes? In the compilation of
Küçükardalı et al. [3] It was shown that diabetic patients did not
get covid-19 infection anymore [3]. In the studies of China and Italy,
the rate of developing covid in the same region in patients with and
without diabetes was found to be the same in outpatients (9-11%)
[4-6]. Is the disease more severe in diabetic patients with Covid
19? In our study, shortness of breath as a symptom was twice as
common in diabetic patients. In Yangli’s study, where the data of the
hospital where critical patients were sent, 48 (25%) of 193 patients
were diabetic. Furthermore, 66% of those with diabetes were taken
to intensive care. In the same study, those with diabetes were older,
lower lymphocyte count, higher d-dimer, CRP, LDH, ferritin, IL-6
[7]. In our study, 25% of the patients were taken into intensive
care, they were older, and the duration of stay in the intensive care
unit of diabetic patients was found to be longer than non-diabetic
patients (20 days vs 8 days). However, in our study, d-dimer, CRP,
LDH, ferritin, creatinine values were not found differences between
the groups. The leukocyte and lymphocyte counts were found to be
higher in the diabetic group in the admission tests, but the decrease
in the lymphocyte count was more significant in the diabetic
group in the test follow-ups performed every two days. It has been
reported that lymphocyte proliferation is inhibited [8], complement
activation is decreased [9], and viral replication may increase [10],
especially in poorly controlled diabetes.
In Tao’s study, anemia was found in one-third of the covid
patients brought to the emergency room. The presence of anemia
in the first days was associated with comorbid conditions rather
than disease severity. However, the development of anemia in the
following days may be due to factors associated with covid 19. In our
study, we found a decrease in hemoglobin values compared to basal
values in the following days. This decrease was more significant in
the diabetic group. We agree with the authors’ opinions put forward
on this issue. Anemia in moderate and severe cases of COVID‐19 is not driven by inflammation alone but a combination of factors,
including direct cytopathic injury resultant from infection of
circulating erythrocytes or their bone marrow precursors, indirect
erythrocyte damage due to hemolytic anemia, and/or thrombotic
microangiopathy, as evidenced by elevated LDH [11-13]. In our
study, we observed an increase in the mean platelet count in the
following days. This increase was not different in the diabetic and
non-diabetic groups [14]. The homeostatic response to platelet
consumption is increased platelet production with an increase in
the IPF. This compensatory response is robust in COVID-19 and
can be out of proportion to the degree of thrombocytopenia, with
elevated MPV and IPF immature platelet fraction. Occurring even
in COVID-19 patients with normal platelet counts [15]. Due to the
small number of our cases, mortality was not evaluated.
Summary
Diabetic patients are older, their stay in intensive care is longer, and their lymphocyte and hemoglobin decrease rates are higher.
References
- Fadini GP, Morieri ML, Longato E, Avogaro A (2020) Prevalence and impact of diabetes among people infected with SARS-CoV-2. J Endocrinol Invest 43(6): 867-869.
- Guan W, Liang W, Zhao Y, Liang H, Chen Z, et al. (2020) Comorbidity and its impact on 1590 patients with covid-19 in China: A nationwide analysis. Eur Respir J 55(5): 2000547.
- Kucukardali Y, Yalçın Arzu, Gezer I (2020) Relationship of covid and diabetes mellitus. Interventions of Obesity and Diabetes 4 (2): 341-343.
- Fadini GP, Morieri ML, Longato E, Avogaro A (2020) Prevalence and impact of diabetes among people infected with SARS-CoV-2. Journal of Endocrinological Investigation 43(6): 867-869.
- Wang L, Gao P, Zhang M, Huang Z, Zhang D, et al. (2017) Prevalence and ethnic the pattern of diabetes and prediabetes in China in 2013. JAMA 317(24): 2515-2523.
- Longato E, Di Camillo B, Sparacino G, Saccavini C, Avogaro A, et al. (2020) Diabetes diagnosis from administrative claims and estimation of the true prevalence of diabetes among 4.2 million individuals of the Veneto region (North-East Italy). Nutr Metab Cardiovasc Dis 30(1): 84-91.
- Yan Y, Yang Y, Wang F, Ren H, Zhang S, et al. (2020) Clinical characteristics and outcomes of patients with severe covid-19 with diabetes. BMJ Open Diab Res Care 8(1): e001343.
- Moutschen MP, Scheen AJ, Lefebvre PJ (1992) Impaired immune responses in diabetes mellitus: Analysis of the factors and mechanisms involved. Relevance to the increased susceptibility of diabetic patients to specific infections. Diabetes Metab 18(3): 187-201.
- Ilyas R, Wallis R, Soilleux EJ, Townsend P, Zehnder D, et al. (2011) High glucose disrupts oligosaccharide recognition function via competitive inhibition: A potential mechanism for immune dysregulation in diabetes mellitus. Immunobiology 216(1-2): 126-131.
- Kohio HP, Adamson AL (2013) Glycolytic control of vacuolar-type ATPase activity: A mechanism to regulate influenza viral infection. Virology 444(1-2): 301-309.
- Tao Z, Xu J, Chen W, Yang Z, Xu X, et al. (2012) Anaemia is associated with severe illness in COVID‐19: A retrospective cohort study. J Med Virol 93(3): 1478-1488.
- Henry BM, Benoit JL, Benoit S, Pulvino C, Berger BA, et al. (2020) Red blood cell distribution width (RDW) predicts COVID‐19 severity: A prospective, observational study from the Cincinnati SARS‐CoV‐2 emergency department Cohort. Diagnostics 10(9): 618.
- Henry BM, Aggarwal G, Wong J, Benoit S, Vikse J, et al. (2020) Lactate dehydrogenase levels predict coronavirus disease 2019 (COVID‐19) severity and mortality: A pooled analysis. Am J Emerg Med 38(9): 1722‐1726.
- Martinelli N, Montagnana M, Pizzolo F, Friso S, Salvagno GL, et al. (2020) A relative ADAMTS13 deficiency supports the presence of secondary microangiopathy in COVID 19. Thromb Res 193: 170‐172.
- Wool GD, Miller JL (2021) The impact of COVID-19 disease on platelets and coagulation. Pathobiology 88(1): 15-27.
© 2021 Abidin Yusuf Kavurmaci. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






