- Submissions

Full Text
Novel Research in Sciences
Undernutrition and Management Outcomes of Hospitalized Children Before and After 2015-Armed Crisis in Aden
Aida H Al Sadeeq*
Aida H Al-Sadeeq, Pediatrics Department, Faculty of Medicine and Health Sciences, University of Aden, Yemen
*Corresponding author:Aida H Al- Sadeeq, Pediatrics Department, Faculty of Medicine and Health Sciences, University of Aden, Yemen
Submission: October 30 , 2020;Published: March 15, 2021
.jpg)
Volume6 Issue4March, 2021
Introduction
In 2015, Yemen spiraled into armed crisis, the ongoing fighting has deteriorated the
economic situation, contracted the Yemen’s gross domestic products (GDP) by about 50% [1]
put the essential public services on the verge of collapse, created a humanitarian emergency,
pushing Yemen to the brink of famine, making it the world’s worst humanitarian crisis [2].
Although undernutrition is primarily a consequence of inadequate nutritional intake,
many other determinants that are negatively affected by conflicts involved in causation,
including poverty and access to health care, water and sanitation. These may be potential
targets for interventions that could have a more sustained effect than reactive nutritional
programs. Thus, understanding the effect of crisis on child nutritional status is extremely
relevant, an issue which has not been studied among hospitalized children thus far as a cost
of Yemeni conflict [3-5].
This review aimed to describe the pattern of undernutrition and outcome indicators
among hospitalized severely malnourished patients during two time periods, 2014 before and
2016 after 2015-armed crisis.
Patients and Methods
A retrospective observational study, conducted in the Therapeutic Feeding Centers (TFC) of Al-Sadaka Teaching Hospital (GTH), Aden, Yemen, during 2014 (before) and 2016 (after 2015 armed crises), included severe acute malnourished (SAM) < 5-year-old patients, who were admitted under the entry category of new SAM and were devoid of any chronic ill condition (new SAM were patients who directly admitted to our facility after being identified as severely malnourished as per the training modules for participants for inpatient management of SAM (WHO modified modules for Yemen) [6].
Data collection & Management
The following data were obtained from SAM registry record on the day of admission: age, gender, address, weight (kg), length/height (cm), MUAC (cm), and the ± bilateral pitting edema. Exit categories were also recorded. Addresses were tallied by 8 districts in Aden governorate and the nearby governorates. Children were categorized into two age groups (<24m, 24-59m). Only the outcome indicators defaulter and death of 6-59 m were evaluated as per the Sphere Minimum Standards (SMS) [7]. No discharge cure from inpatient care to compare with SMS cure rate. The recorded data were analyzed using SPSS for Windows (Version 25.0).
Result
A total 621 new SAM patients were admitted during the study periods, included 257 (41.4%), and 364 (58.6%) during 2014 and 2016 respectively. It was found that edematous malnutrition was significantly high among ≥ 24-month-old patients, whereas severe wasting was significantly high among under 24-month-old patients, (p=0.000), Table 1.
Table 1: Distribution of Admitted Children by Age Group During the Study Period.
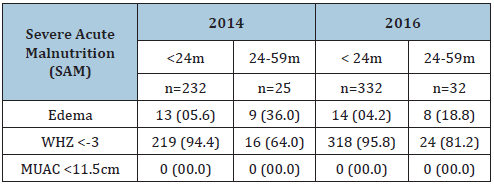
Figures in parentheses are percentages.
In Table 2 the mean and SD of age, weight and length/height of the patients during the two-year periods were nearly similar. There was no significant gender difference. The majority of admitted children were from Shikh Othman and Dar Sad districts/Aden governorate. Lahj and Abyan governorates were in the second and third order. Increased percentages of admitted patients in 2016 were from Altawahi, Khourmakser, and Serra districts, which were the scene of armed clashes during 2015. Table 3 shows the exit categories of 6-59-month-old patients. There were 195 and 294 belong to the age group 6-59 months during 1014 and 2016 respectively. Compared to 2014, poor outcome indicators were seen in 2016 with low recovery (70.1%), and high death and defaulter (24.5%) rates.
Table 2: Demographic Characteristics, Mean and SD of
Weight and Length/Height of the Study Children.
Figures in parentheses are percentages. *Including patients
from Taiz, Almakha, & Alhodaida governorates.
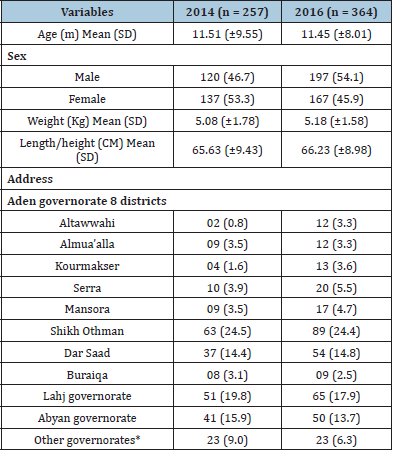
Table 3: Exit Categories of the 6-59 Study Patients During Management.

#Recovered cases referred to OTP or SFP to continue rehabilitation until cure, *Outcome indicators
Discussion
The study provides evidence that the frequency of severe
acute malnutrition increased in 2016 coupled with poor outcome
indicators. These negative health outcomes could be attributed
directly to the damaging effect of the armed conflict, and or
through accentuation and exacerbation of the country’s endemic
humanitarian problems, i.e., inadequate household food security,
insufficient health services, poor environment, and poor maternal
and childcare practices, which lead to deterioration in the
nutritional status of children [3-5].
The majority of admitted children were from Shikh Othman
and Dar Sad districts, these two districts have high population size
[8], in addition these were crowded by the internally displaced
people (IDP) from conflict affected districts in Aden and the nearby
governorates; the internal displacement has worsened the already
existed poor public health services [9].
The high defaulter rate (24.5%) found in 2016 compared
to Sphere Standards (<15 %) [7] is likely to be linked to reasons
belong to the patients [6]. Fortunately, the death rates in 2014 and
2016 are much lower than the accepted minimum for inpatient care
as per Sphere Standards of (<10%) [7], this could be attributed to
strict adherence to the training modules for inpatient management
of SAM, good quality care and clinical monitoring by the skilled
staffs [6].
Conclusion
Poor nutritional and outcome indicators were encountered in 2016 after the 2015-armed crisis. It is incumbent on pediatricians, public health professionals, and policy makers to seriously address undernutrition in the context of conflict as critical and priority issue.
References
- Langendorf M (2019) Beyond the war: The deep roots of Yemen’s economic crisis [Internet]. The New Arab, London, United Kingdom.
- UNICEF (2019) Yemen country brief [Internet].
- Ohannessian SG (2016) Conflict in Yemen and child malnutrition [Internet]. Economic research forum.
- De Souza LR (2017) Correlates of child undernutrition in Yemen. Bandung: J Global South 4(1): 3.
- (2017) European Commission, Country profile on nutrition, Yemen.
- WHO (2013) Modules for Participants: Training course on the inpatient management of severe acute malnutrition, the Yemeni version.
- SPHERE Project Team (2003) The SPHERE humanitarian charter and minimum standards in disaster response. The SPHERE Project, Geneva, Switzerland.
- Central Statistical Organization (Yemen) (2004) Yemen general population, housing and establishment census [Internet]. Sana’a Yemen: Central Statistical Organization (Yemen).
- Sallami Z, Kassim Y, Selvaraj J, Parry E, Winter G (2017) Impact of the armed conflict of 2015-2016 in Aden on health services and the availability of medicines. Health 9(4): 685-696.
© 2021 Aida H Al Sadeeq. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






