- Submissions

Full Text
Novel Research in Sciences
Gastric Outlet Obstruction Caused by PEG tube: A Case Report
Elmutaz Abdalla Mekki Kanani1* and Mohammed Hamed Naseeb Al Hinaei2
1Department of General Surgery, Oman
2Department of Gastroenterology, Oman
*Corresponding author: Elmutaz Abdalla Mekki Kanani,Department of General Surgery, Oman
Submission: September 21, 2020;Published: November 02, 2020
.jpg)
Volume5 Issue1November, 2020
Abstract
The percutaneous endoscopic gastrostomy (PEG) is the method of choice for a durable gastrointestinal tract access for feeding or gastric decompression. The basic indication is maintenance of adequate intake to meet the metabolic demands in patients who cannot do so normally, as a result of several disease states. PEG is typically a safe procedure if the guidelines and safety measures are followed. Gastric outlet obstruction (GOO) is a rare complication of PEG. Here we are discussing a case of GOO as a result of catheter balloon migration. We will briefly discuss the diagnosis, treatment, and safety measures to avoid this uncommoncomplication
Keywords: Percutaneous endoscopic gastrostomy; Gastric outlet obstruction; Endoscopy; Complication.
Introduction
Percutaneous endoscopic gastrostomy (PEG) is currently the preferred method for moderate to long term enteral feeding in patients who cannot use the normal oral route, provided that their gastrointestinal system is functional. This also helps preserve the gut activity which is important in boosting immunity and preventing bacterial translocation. It was initially introduced in 1980 by Gauderer et al. [1] as they strive to avoid laparotomy for gastrostomy access in the pediatric population [1]. Technical simplicity, safety, and elimination of the need for a general anesthetic and laparotomy are on the top of the list of the reasons behind its popularity. It allows durable optimization of feeding, but also requires occasional replacement [2]. Although considered a safe procedure, it has a potential for serious complications either during the insertion procedure or thereafter.
Case Presentation
This is a 77-year-old lady with a background history of diabetes mellitus, hypertension, hyperlipidemia, and bilateral knee osteoarthritis. She had suffered a cerebrovascular accident in 2013 which resulted in right sided middle cerebral artery distribution territory infarct and multiple lacunar infarcts. The collective sequelae of stroke and severe knee osteoarthritis left her bed bound. Later on, she had developed progressive swallowing difficulty in 2017, for which she was subjected to comprehensive work up that did not bring to light any specific cause. She ended up with a PEG tube insertion in 2018 with frequent subsequent replacements. The reasons for the previous tube replacements were tube clogging or a small tube size to meet her feeding requirements. Recently in January 2020, she was brought by family with complaints of bloating, nausea, and occasional vomiting. They noticed that they cannot deliver the same amount of feeding that was regularly being given since the latest tube change few months ago.
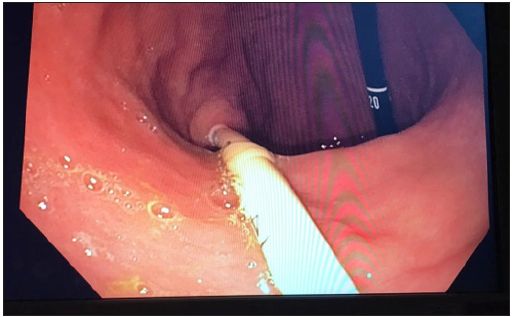
Her general examination was unremarkable and there were no abdominal signs. Investigations were as follows: Hemoglobin 10.9g/dl (Ref. 11-14.5), Platelets 210 103/µL (Ref. 150-450), White Blood Count 5.6 109/L (Ref. 2.4-9.5), C - reactive protein 1mg/L (Ref. 0-5), Erythrocyte sedimentation rate (ESR) 15mm/hr ((Ref. 0-15), Serum urea 4.3mmol/L (Ref. 2.5-7.5), Serum creatinine 71µmol/L (Ref. 44-80), Serum Sodium 132mmol/L (Ref. 135-145), Serum Potassium 4.2mmol/L (Ref. 3.5-5), Serum Chloride 89mmol/L (Ref. 95-110), Total serum bilirubin 8µmol/L (Ref. 3-19), Total serum protein 67g/L (Ref. 60-80), Serum albumin 43g/L (Ref. 35-50), Serum globulin 24g/l (Ref. 24-35). Her medications list includes metformin 1 gram and gliclazide 40mg twice daily, lisinopril and amlodipine 5mg each once daily, atorvastatin 20mg and clopidogrel 75mg daily. An esophagogastroduodenoscopy (EGD) showed the balloon of the PEG tube tightly impacted in the pylorus causing gastric outlet obstruction (Figures 1 & 2). It was not possible to pull the tube without deflating the balloon. The PEG tube was replaced with a Mushroom-type tube through the existing matured tract under direct endoscopic visualization without any difficulty. Patient had complete symptomatic relief and remained stable with good PEG function 8 months after the procedure.
Figure 1: Endoscopic view of the balloon stuck in the pylorus.
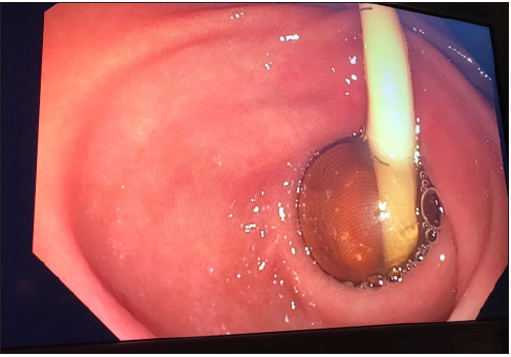
Figure 2: PEG tube emerging from the gastro-cutaneous mature tract.
Discussion
Gastrostomy tube feeding has long been practiced for feeding or gastric decompression purposes. Its insertion used to be through laparotomy under a general anesthetic or mini laparotomy under a local anesthetic in a selected cohort of patients. Gauderer et al. [1] had revolutionized the procedure in 1980 by their successful endeavor to utilize a combined endoscopic and percutaneous approach that helps to avoid both laparotomy and general anesthesia [1]. Ever since, the PEG approach had gained global popularity and is currently the most preferred approach [3]. Despite PEG excellent safety profile, it still carries a potential for both minor and major complications if insertion guidelines are not adhered to [2,3]. Comprehensive knowledge of PEG indications and contraindications together with proper management of patient’s co-morbidities and strict adherence to procedure precautions are the means to avoid complications [4].
Terino et al. [5] mentioned morbidity of 9.4% and mortality of 0.53% related to PEG [5]. Complications can be classified into three broad categories: immediate, delayed, or late [4]. Immediate complications are those related to the endoscopy and tube insertion procedures like bleeding and visceral injury. Delayed complications may occur within few days following the procedure, such as leakage, ileus, aspiration pneumonia, wound infection, etc. Beyond these time-frame complications may be considered late. Late complications may include but not limited to; enterocutaneous fistula formation, tube dislodgement and migration, inadvertent removal, ulceration, etc. Some complications are specific to certain procedure techniques as described by Pih et AL. [6].
Gastric outlet obstruction (GOO) is a rare complication of PEG. It happens when the PEG lodges in the pylorus or duodenum and results in partial or complete obstruction [7]. It can also obstruct the ampulla of Vater resulting in acute pancreatitis [8]. Both tube types with internal bolster and balloon can be implicated in causing GOO. Patient presentation depends upon the extent of the obstruction whether partial or complete. Generally, they present with abdominal cramps and intermittent vomiting. Reduced amount and new onset difficulty in giving feeds should prompt the exclusion of tube malposition. Diagnosis of the condition requires a high index of suspicion. Upper gastrointestinal imaging and endoscopy readily identify the problem. Endoscopy can be diagnostic and therapeutic simultaneously. Treatment of the condition is by tube re-positioning/retrieval. If the malposition occurs before the tract maturation (<4 weeks), endoscopic maneuvering can be attempted to ensure proper placement/replacement [9]. Post tract maturation tube can be replaced through same existing tract, after balloon deflation in balloon type tubes. In the latter case, proper position of the tube can be confirmed by water-soluble contrast study if any doubt exists [7,9]. An external bolster helps to keep the tube in position and avoid this complication of tube migration while an internal bolster keeps the stomach opposed to the abdominal wall [10]. Suturing the external bolster to the abdominal wall adds more security to the tube position.
Conclusion
Percutaneous endoscopic gastrostomy is currently the preferred method for long term enteral access. The procedure is safe but has a potential for serious complications. Gastric outlet obstruction is a rare complication of PEG. Treatment is straightforward when recognized. Awareness of the condition and the preventive measures are essential in reducing its incidence.
References
- Gauderer MW, Ponsky JL, Izant RJ (1980) Gastrostomy without laparotomy: a percutaneous endoscopic technique. J Pediatr Surg 15(6): 872-875.
- Schurink CA, Tuynman H, Scholten p, Arjaans W, Knol ECK, et al. (2001) Percutaneous endoscopic gastrostomy: complications and suggestions to avoid them. Eur J Gastroenterol Hepatol 13(7): 819-823.
- Azar AAR, Rahnemaiazar AA, Naghshizadian R, Kurtz A, Farkas DT (2014) Percutaneous endoscopic gastrostomy: indications, technique, complications and management. World J Gastroenterol 20(24): 7739-7751.
- Tomas H, Julius S (2016) Complications of percutaneous endoscopic gastrostomy. Best Pract Res Clin Gastroenterol 30(5): 769-781.
- Marisa MDT, Haleh MDV, Jeremy DOI (2017) Complications of a minimally invasive procedure: The PEG tube. American Journal of Gastroenterology 112: S1549-S1550.
- Pih G, Na H, Ahn J, Jung KW, Kim HD, et al. (2018) Risk factors for complications and mortality of percutaneous endoscopic gastrostomy insertion. BMC Gastroenterol 18(1): 101.
- Sherwin P, Sharma R, Jaik NP, Seamon MJ, Lukaszczyk JJ, et al. (2007) Complications related to percutaneous endoscopic gastrostomy (PEG) tubes. A comprehensive clinical review. J Gastrointestin Liver Dis 16(4): 407-418.
- Hawatmeh A, Alkhateeb A, Arqoub AA, Jumean K, Shaaban H (2016) Gastrostomy tube migration complicated with acute pancreatitis: Two case reports with review of literature. Int J Crit Illn Inj Sci 6(1): 48-50.
- Robert JS, Munot K (2018) Common gastrostomy feeding tube complications and troubleshooting. Clin Gastroenterol Hepatol 16(12): 1864-1869.
- Ponsky JL, Gauderer MW (1981) Percutaneous endoscopic gastrostomy: a nonoperative technique for feeding gastrostomy. Gastrointest Endosc 27(1): 9-11.
© 2020 Elmutaz Abdalla Mekki Kanani. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






