- Submissions

Full Text
Novel Research in Sciences
Drug Mixed by H2O2 Injection Intratumoral to turning an Extracellular Matrix into Autologous Coagulum as Drug Depot
Baofa yu MD*1 and Qiang FU MS2
1Shandong Baofa Cancer Institute, USA
2Taimei Baofa Cancer Hospital, China
*Corresponding author: Baofa yu MD, Shandong Baofa Cancer Institute, Immuno Oncology Systems, Inc., San Diego, CA 92122, USA
Submission: June 20, 2020;Published: July 10, 2020
.jpg)
Volume4 Issue2July, 2020
Abstract
Aim: To explore the nature of hydrogen peroxide at higher dosage for denature-aggregation of tumor with drugs through aggregation in denatured tumor for turning extracellular matrix into autologous coagulum for drug depot and prolong function of drug.
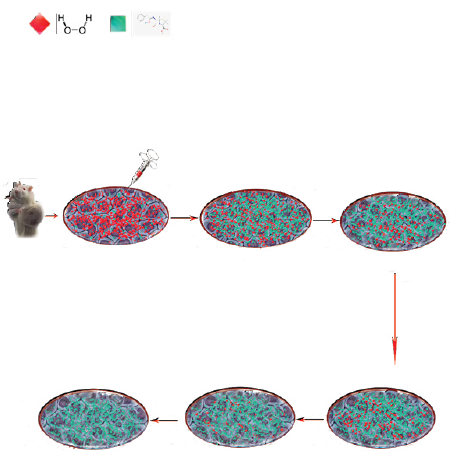
Method: Injection of oxidant mixed drug into tumor.
i. Preparation for two 5 ml of BLM-I131, one diluted with 0.12 ml NS and 0.2 ml (0.2mCi =49.67µg BLM) for tumor injection in control group; one diluted with 0.12 ml of H2O2 (0.833 mg/ml) and 0.2 ml (0.2mCi =49.67µg BLM) for tumor injection in experimental group.
ii. Tumor imaging with BLM-I131 analyzed at different time points.
iii. Radioactivity in tumor of mice analyzed under SPECT scanning imaging instrument at the 0, 5 h, 1 h, 2 h, 4 h, 8 h, 24 h, 48 h, 96 h, 120 h, 144 h and 168 h, activity of isotope I131 is representing the BLM retaining time in tumor.
iv. Also, tumor sectioned and observed cellular and extracellular matrix changes of histological structure.
Result: It was observed that BLM-I131 with ROS in tumors sustained for 168 hours while BLM-I131 with NS in tumors sustained for 8 hours only. Radioactivity of BLM-I131 in tumors with ROS reach at peak 1.5 hours and second peak at 20 hours by average to extend to 168 hours, while radioactivity of BLM-I131 in tumors with NS reached at peak in 0.5 hour, decreased to 30% in 1.5 hour quickly to background in 8 hours; We observed the extracellular matrix changes in experimental tumor while no changes in control tumor.
Conclusion: A water soluble oxidant mixed with free drug can play a biological scissors role to chop tumor matrix, then it resulted in a denature tumor matrix into a coagulation for a drug depot, it showed drug of BLM-I131 sustained in tumor for a long time; while oxidant plays an important role to punch holes on cell membrane and resulted a high permeability for high concentration drug in each cancer cells.
Figure 1:
Keywords: Drug delivery; Extracellular Matrix as Drug Carrier; Autologous Coagulum; Intracellular Drug Delivery
Introduction
Drug delivery is considered important and has been evaluated and applied extensively in drug development with various formulations improving patient compliance and convenience [1]. Current technologies allow delivery of release drugs from days to years. Implantable systems can locally delivery drugs for months, even years. While such significant advances are been made, there are still a area where substantial improvements need to be made bring care of cancer patients to next level clinically. The benefit of drug delivery technologies lies in the ability to specifically target a drug including intratumoral injection or drug slow release to minimize drug-originated systemic toxic effects [2]. There has not been much thought for applying about that drug leaves carrier to tumor cells then circulates throughout the whole body. While the drug is linked to the carrier, the drug may not take action to kill tumor cells; when the drug leaves the carrier, the drug may go anywhere and resulted less effective to kill of the tumor. Other factors such as difficulty injection and poor distribution due to viscosity of delivery drugs are limiting clinically improvement for most tumor treatment with various drug delivery systems or formulations. Twenty-eight years ago, author came to realize how to integrate drug delivery in tumor with water soluble drugs to overcome the viscosity of difficulty injection and reach a better distribution within a tumor. While studying liposomal drug delivery for intratumoral chemotherapy, he realized an idea about comprehensive therapy with reactive oxygen species (ROS) for anticancer drug in water soluble solution with easier injection and good distribution within tumor.
ROS a big family of reactive oxygen species including H2O2, the activity of reactions is a double-edged sword and the nature of ROS is exemplified in apoptosis of cancer cells [3,4]. Strong ROS-producing oxidant can damage any vital cellular structures like DNA and protein [5]. It is good example to know that function of hydrogen peroxide can denature proteins like Whey protein when it reaches a higher than 0.1% concentration for clean the bacteria during the manufacture of milk [6]). There is no reported that hydrogen peroxide is used for establishing a drug depot with sustaining release drugs in the treating tumor. But exogenous hydrogen peroxide can kill tumor cells at higher concentration through chemical denature protein (naturally like a chemical chop or blender) [7]. ROScan embed anticancer drugs in tumor through intratumoral injection of ROS and denature aggregation of tumor mass as drug depot to prolong function of drug and kill the rest of cancer cells. We applied to intratumoral injection of oxidant mixed with drug in animal tumor models.
Result
BLM-I131 labeling rate was 86% after Sephadex G250 column chromatography were collected for BLM-I131solution [8]. Activity of BLM-I131 measured by Gama-meter was 1.002mCi/ml, labeling rate ishigher enoughfor representative of BLM sustaining in vivo study.
It was observed that BLM-I131with oxidant was sustained in tumors to 168 hours in experimental group while BlM-I131 with NS was sustained in tumors only to 8 hours in control group. Radioactivity of BlM-I131 in tumors reached at peak in 0.5 hour in control group, decreased to 30% in 1.5 hour quickly to background in 8 hours; but radioactivity of BlM-I131 with oxidant in tumors reach at peak 1.5 hours and second peak at 20 hours by average of data analysis, significantly longer sustaining BLM-I131 with oxidant than it was with NS in tumors, then slowly start to decrease to background in 168 hours (7 Days) (Table 1, Figure 1 & Figure 2).
Table 1: The activity of the BLM-I131 of the experimental and control groups at different time points (μCi)
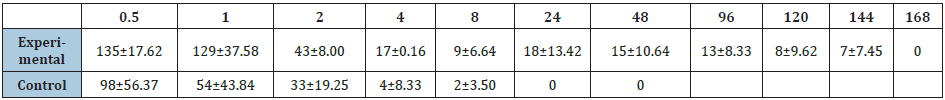
Figure 1: The activity curve of BLM-I131 in two groups at different time points. It is the activity curve of BLM-I131 in two groups at different time points and showed that BLM-I131 is sustained in tumor of experimental for a long time over 168 hours with oxidant while it is sustained in tumor of control only for 48 hours.
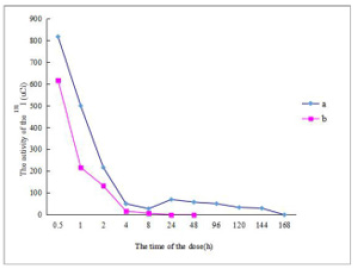
Figure 2: The SPECT imaging of the two groups at different time points. It showed that I131 activity in tumor of mice under SPECT, red light is the light of I131 under SEPCT imaging, at 168 hours in experimental group, I131 is still showing as red light while it is in control group. I131 is not showing any red light. a) Experimental b) Control
It was observed in C57 BL mice with melanoma cells that the structure changes were in experimental tumor while no changes in control tumor (Figure 3). the structure changes included cellular and extracellular matrix, massive leukocytes appeared at 1 hour after injection with oxidant, tumor cell was apoptosis with shrinkage, micro holes on cell membrane, more heterochromatin with concentrated at 12 hour after injection, tumor cell loose arranged with more mesenchyma and collagenous fibers at 48 hour after injection, tumor cell loose arranged with massive leukocytes and desmocyte at 48 hour after injection, tumor cell shrinkage with more heterochromatin and massive aggregation at 168 hour after injection (Figure 3).
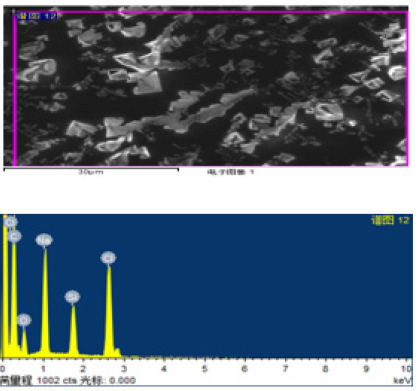
It was also observed in themelanoma cell smear that the large quantity of crystals was in smear from experimental tumor at 4 and 24 hours after injection with oxidant while a little crystal was in smear from control tumor with NS injection (Figure 4). It was also observed that cell and cell debris in treatment and drug crystal separation in the post treatment (Figure 5), which showed the ROS could punch holes on cell membrane to create higher permeability and that is why drug crystals was observed under electronic microscope. It showed that element, Na k weight ratio increased to 8.67 to 5.75 from 1.36 to 0.78, element, Cl cok increased to 18.49 to 7.95 from 1.30 to 0.46 under electron microscope and μm (micrometer) level by scanning with beam detecting (Table 2).
Also showed elements of drug penetrated into tumor cells at higher level immediately (Figure 5A & 5B).
Figure 3: The observation of the Balb/c H22 tumor-bearing mice after intratumoral injection under the transmission electron microscopy A. 5000×14, control tumor: the tumor cells were regularat 1h after injection with normal saline. B. 5000×14, experimental tumor: massive leukocytes were appeared, leukocyte and tumor cellat1h after injection with oxidant. C. 5000×14, experimental tumor: the tumor cells were apoptosis with shrinkage, cell debris at 12h after injection with oxidant. D. 5000×14, experimental tumor: the tumor cells loose arranged with more mesenchyma and collagenous fibres48h after injection with oxidant. E. 5000×14, experimental tumor: the tumor cells loose arranged with massive leukocyte and desmocyteat 48h after injection with oxidant. F. 5000×14, experimental tumor: the tumor cells were apoptosis with cell shrinkage, more heterochromatin and massive aggregation at 168hafter injection with oxidant.
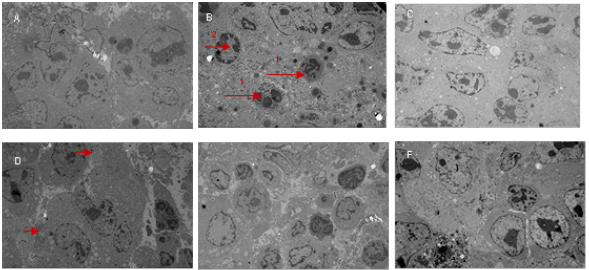
Figure 4: Fig 4 Theobservation and analysis of the melanoma cell smear with C57 bl/ctumor bearing mice under scanning electron microscope (Type: FEI Nova NanoSEM 450). A. 100×1, Controlgroup: cell debris and a little crystal separation from injection at 1 hour after injection with normal saline. B. 100×1, experimental group: large quantity of crystal is in smear at 1h after injection with oxidant. C. 100×1, experimental group: lot of crystal separation at 4 h after injection with oxidant compared the crystalat1hafter injection. D. 100×1, experimental group: lot of compounds of the cell debris and crystal separation at 24 h after injection with oxidant.
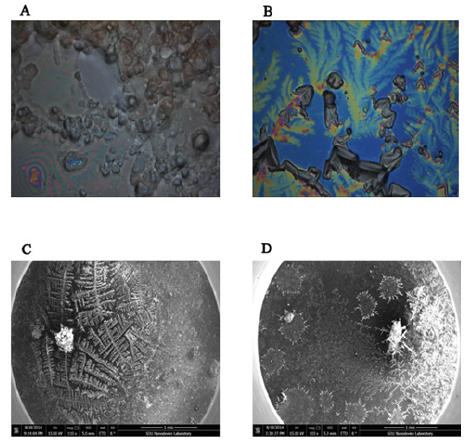
Table 1: Comparison before and 24 hours after Injection with water soluble free drug with oxidant.
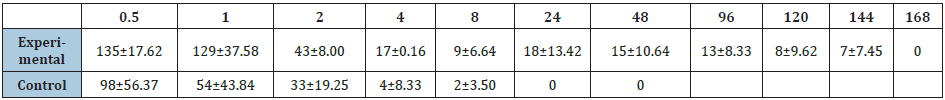
Figure 5A: 5A.it showed that Na K and Cl cok ration (%) at higher numbers before injection with drug in water soluble solution with oxidant under electron microscope and μm (micrometer) level by scanning with beam detecting.

Figure 5B: 5A.it showed that Na K and Cl cok ration (%) at higher numbers before injection with drug in water soluble solution with oxidant under electron microscope and μm (micrometer) level by scanning with beam detecting.
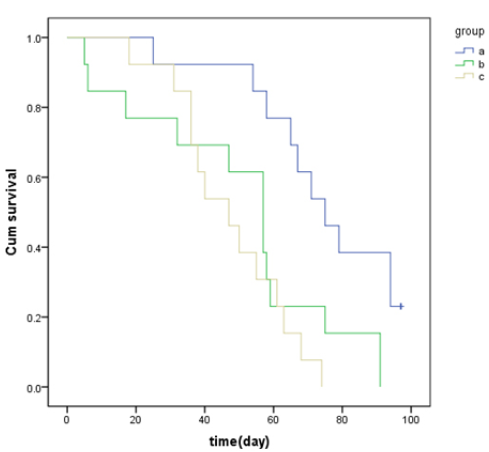
Pathological changes were found in experimental tumors, more inflammatory cells appeared in tumor 1 h after injection with oxidant, fibroblast cell appear in tumor 24 h after injection with oxidant and large obvious fibrosis proliferation at 168 h after injection with oxidant (Figure 6), also observed the median survival time of the experimental group was 75 days, only 56 days and 46 days in the control and non- treatment groups, respectively (both P<0.05) (Figure 7). It was observed the tumor cell growth well, tumor cell infiltrating into the muscle and tumor partial necrosis in the control group.
Figure 6: Pathological changes of the tumors in control and experimental groups at different time points in Balb/c mice with H22 tumor A1: control group (×100), the tumor cells grew well at1 hour after injection. A2: control group (×100), the tumor cell was infiltrating the muscle at 24 hours after injection. A3: control group (×100), there were partial necrosis of the tumor tissue 168 h after injection. B1: experimental group (×100): there were infiltration zone with inflammatory cells at 24 hours after injection. B2. Experimental group (×400), obvious fibrosis proliferation at 168h after injection.
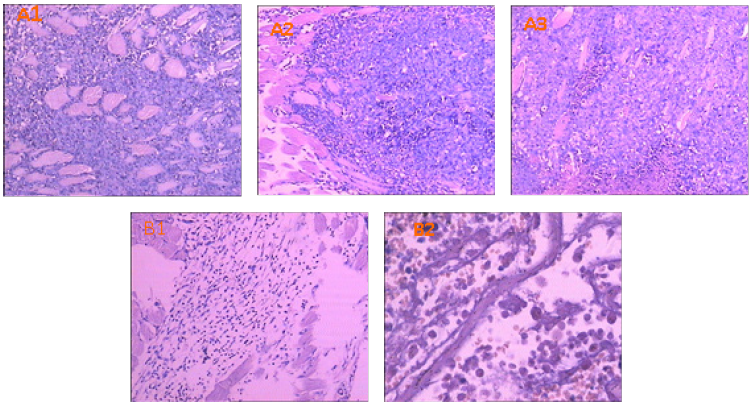
Figure 7: Survival curve of experimental H22 mice with tumor The median survival time of the experimental group was 75 days, and 56 days and 46 days in the positive and negative control groups, respectively. The experimental group obviously prolonged the survival time and showed significantly difference compared to the positive and negative control group with the p value 0.022 and 0.015.
Discussion
Drug delivery technology had advanced a significantly interesting for cancer chemotherapy in last several decades. There is a gap between the promising preclinical approaches to clinical trial which is a poor success rate and may relate to selection status of disease at time of trial. Conventional chemotherapy was given most of patients who lost opportunity of surgery in order to kills rapidly proliferating cells including residual cancer cell, while chemotherapy produce side effect like suffer from hair loss, stomach irritation, and damage bone marrow. Therefore, drug delivery system was focused on “target drug delivery” to site of the tumor, the effective target drug delivery must fully meet the four key requirements: target, retain, evade and release [9]. For Intravenous administration, it requires drug loaded effectively in delivery vehicle, sufficient residence to reach intended sites of the body by the circulation, retention and drug release within a period time and intended sites (i.e., targeting) that enough allows for function of drug. Classical liposomes (i.e. phospholipid bilayer vehicles) have been effective in decreasing the clearance of encapsulated agents and in passively targeting specific tissues with considerable limitations [10], pupylation has been used extensively to modify the pharmacokinetics of the drug itself and/protein-drugs [10]. Name of “active targeting” means a variety of factors that includes: efficient ligand-receptor, target cell selective expression, receptor availability, the rate of internalization vs shedding of that surface receptor, etc. Further, deference between expression of a promising tumor-targeting receptor and homogenously distributed within a tumor may change its surface expression over time [11-13]. By the ROS function, with injection of water soluble free drug with oxidant, tumor cell is denatured like punch with multiple holes on membrane, it make easier for drug or hepten is easily allowed penetrate into tumor cell, and the tumor associated antigens may be haptenated and release into blood circulation also, it can explain that Dr. Yu’s group for treating pancreatic cancer with a prolong survival time after introtumoral injection with anticancer drug and oxidant [14].
The same limitation has happened for most drug targeting delivery systems not as “active targeting”, less thought about the drug leaves carrier to tumor cells and also circulates to the whole body; while the drug is linked to the carrier, the drug cannot take action to kill tumor cells; when the drug leaves the carrier, the drug may go anywhere of whole body and resulted less effective killing on the tumor. Other factors such as difficulty of injection and poor distribution due to viscosity of most delivery drugs are limiting clinically improvement.
There, we developed an introtumoral injection for anticancer drug sustaining in tumor by apply a water-soluble drug with ROS solution, it overcome the difficulty of injection and poor distribution of drug in tumor.
First, we observed Balb/c mice with H22 cells that BlM-I131with ROS was sustained in tumors to 168 hours (7 days) for experimental group while BlM-I131with NS sustained in tumors only to 8 hours for control group. Radioactivity of BlM-I131with ROS in tumors reaches at peak 1.5 hours and second peak at 20 hours by average of data analysis, significantly longer sustaining BlM-I131 in tumor than it is with NS in tumors, then start to decrease slowly to background in 168 hours (7 days). It gives a great period of time for bleomycin (or any drugs)to take an action for killing tumor cells at tumor site of injection.
Second, we observed the structure changes in section from experimental tumor while no structure changes in section from control tumor. The structure changes included cellular and extracellular matrix, massive leukocytes appeared, tumor cell apoptosis with shrinkage, micro holes on cell membrane, more heterochromatin, tumor cell loose arranged with more mesenchyma and collagenous fibers, tumor cell loose arranged with massive leukocytes and desmocyte, tumor cell shrinkage with more heterochromatin and massive aggregation. The all changes was induced by ROS imbalance with Redox-relevant aspect of the cellular and extracellular matrix [15], it resulted in coagulation of tumor matrix like soft for drug sustaining in tumor as a drug depot [16] and drug penetration into tumor cells to kill tumor cells. We also observed the large quantity of crystals drugs at µm level in smear of the melanoma with ROS while a little crystal drugs in smear of control tumor, which showed the drug penetrated into tumor cell with ROS, so that is why the drug kill tumor cell more effectively while drug stays a long period of time in tumor. We observed that cell debris with drug crystal separation in the post treatment slice at cell level and sub cell levels, it showed the evidence of oxidantpunchholes on cell membrane to create higher permeability and allow drug penetrated into tumor cells; that is why drug crystals observed under electronic microscope.
Final, The median survival time of the experimental group was 75 days, and 56 days and 46 days in the positive and negative control groups, respectively (both P<0.05 ), prolonger of sustaining drug in tumor resulted in a long survival time with introtumoral injection with a water soluble free drug with oxidant.
Conclusion
A water soluble oxidant with free drug can play a biological scissors role to chop tumor matrix and it resulted in a denature tumor matrix into a coagulation as a drug depot; the oxidant plays a role to punch holes on cell membrane and resulted a high permeability with high concentration drug or hapten into each cancer cells in order to kill tumor cell and mix cell debris or antigens (P53, P16, Surl, MLSN) with hapten (unpublished data), which is possible for autologous vaccination at tumor site since we found autologous antibodies increased after this treatment, which give a good explaining why Dr. Yu’s group for treating pancreatic cancer with a successful prolong survival time after introtumoral injection with anticancer drug and oxidant [14].
Method
All methods were carried out in accordance with relevant guidelines and regulations in china and the protocol approved by Jinan Baofa Cancer hospital committee with ethical approval in one time.
Materials and equipment
I13115mCi in 10 ml (Beijing Atomic Hi-Tech co., LTD); Bleomycin (BLM) (Japanese medicine Co, LTD); SPECT model: GE Hawkeye SPECT with I131 in the collimator.
Animal tumor model and method
Animal tumor model preparation: all mice (Balb/c) were keep in room with 12-hour light and 12 dark at room temperature between 15 °C and 20 °C with permit of animal care. Each of mice were inoculated by the 0.2ml/per with H22 cells of 2.34×106/ml in normal saline in left forearm axillary for tumor model, when tumor grows to the size about 1x1 cm, mice with size similarly tumor were divided into two groups in control (66 mice) and experimental (66 mice) for drug sustaining studies, additional for non-treatment group as a negative survival control. Also prepare the C57BL/6 mice inoculated by 0.2 ml/per with melanoma cell of 3x106/ml in normal saline in left axillary for tumor model, when tumors grows to the size about 1x1 cm, choose similarly tumor for drug injection and prepare the tumor samples and section into micro slices for scanning electron microscope (SEM) analysis.
Drug preparation: I. 0.1mol/NaoH buffer solution: 5.6ml of saturated liquid NaoH was added into 1000ml cold water from new boiling water with oscillation.=
PH 7.4 KH2PO4: 1.36g was added into 79 ml of 0.1mol/l HaoH, diluted into 200 ml with oscillation.
III. Bleomycin labeling with I131: BLM (Bleomycin) 15mg was added into 3ml KH2PO4 buffer solution with oscillation, then 0.6 ml (3mg) was mixed with I131 15mCi in 10 ml, shaken and placed for 20 min, added NS to 15 ml to be final concentration of BLM labeled I131 with BLM 0.2mg per ml with 1mCi of I131. Labelled rate is 86% of drug with I131, finial concentration of BLM-I131 is 248.44µg/ml. The two 5 ml of BLM-I131, one was diluted with 0.12 ml NS and 0.2 ml (0.2mCi = 49.67µg BLM) for tumor injection in control group; another one was diluted with 0.12 ml of oxidant (H2O2, 7.23 mg/ml) and 0.2 ml (0.2mCi = 49.67µg BLM) for tumor injection in experimental group [8].
Intratumoral delivery for sustaining study: Total 132 mice (Balb/c) with tumors were divided into 66 mice as control groups, 66 mice as experimental groups, each tumor was intratumoral injected with 0.2ml (0.2mCi) BLM-I131 in NS in control groups and each tumor was intratumoral injected with 0.2ml (0.2mCi) BLM-I131 in oxidant solution in experimental group, both for analysis of BLM-I131 PK study and survival study.
Tumor imaging and BLM-I131 account analysis: at different time point, four mice in each group were put into anesthesia for tumors removing, each tumor was keep in single bottle with an aqueous solution of formaldehyde, and determination of its radioactivity in difference time and days, rendering the radioactivity curves. Radioactivity in tumor was analyzed under SPECT scanning imaging instrument at the 0, 5 h, 1 h, 2 h, 4 h, 8 h, 24 h, 48 h, 96 h, 120 h, 144 h and 168 h. Left mice were keep to live for survival study analysis.
Each tumor in C57Bl/6 mice was sectioned by the pathological slicer and observed cellular and extracellular matrix changes of histological structure under both microscope and transmission electron microscopy or scanning electron microscope.
Statement of the issue of ethical: Study related with animal (rats) ethical has been approval from Shandong Baofa Therapeuitcs’s ethics committee, however the research is not related using a part of the amniotic membrane of neonates and any source of the fetal bovine serum.
Competing interests: The both of authors Baofa Yu, MD and Qing Fu declared that there is no a competing interests, also one of us did not get any research fund from government or from any private fund for this research.
Author Contribution Statement
Baofa Yu had designed of the research protocol and wrote the main manuscript all, Qing Fu had done the experiment and prepared a figures and table.
Acknowledgement
Thanks to Prof. Xuemin Xu who gave a help in writing for main manuscript and he currently is working at The University of Texas Permian Basin (UTPB).
References
- Hoffman AS (2008) The origins and evolution of “controlled” drug delivery systems. J Control Release 132: 153-163.
- You Han Bae, Kinam Park (2011) Target drug delivery to tumor: Myths, reality and possibility. J Control Release 153(3): 198-205.
- Andy TY Lau, Ying Wang, Jen-Fu Chiu (2008) Reactive Oxygen Species: Current knowledge and Application in Cancer Research and Therapeutic. Journal of Cellular Biochemistry 104: 657-667.
- Plaine HL (1955) The effect of oxygen and hydrogen peroxide on the action of a specific gene and on tumour induction in drosophila melanogaster. Genetics 40(2): 268-280.
- Martindale JL, Holbrook NJ (2002) Cellular response to oxidative stress: Signaling for suicide and survival. J Cell Physiol 192: 1-15.
- Nancy L, Fish R (1967) Effect of Hydrogen Peroxide on Whey Protein Nitrogen Value of Heated Skimmilk. Journal of Dairy Science 50(7): 1045-1048.
- Cooney CM, Morr CV (1972) Hydrogen Peroxide Alteration of Whey Proteins in Whey and Concentrated Whey Systems. Journal of Dairy Science 55(5): 567-573.
- Avcibasi U, Demiroglu H, Unak P, Muftuler FZB, IchedefC A, et al. (2010) In vivo Biodistribution of I131labled Bleomycin and Isomers (A2 and B2) on Experimental Animal Models. Journal of Radioanalytical and Nuclear Chemistry 285(2): 207-214.
- Mills JK, Needham D (1999) Target Drug Delivery. Expert Opin Ther Patents 9: 1499-1513.
- Harris JM, Martin NE, Modi M (2001) Pegylation -A novel Process for Modifying Pharmacokinetics. Clin Pharmacokinet 40: 539-551.
- Capone PM, Papsidero LD, Chu TM (1984) Relationship Between Antigen Density and Immunotherapeutic Response Elicited by Monoclonal Antibodies AgainstSolid Tumors. J Natl CancerInst 72(3): 673-677.
- Wen DY, Hall WA, Conrad J, Godal A, Florenes VA, et al. (1995) In vitro and in vivo Variation Intransferr in Receptor Expression on a Human Medulloblastoma Cell Line. Neurosurgery 36: 1158-1164.
- Li YM, Hall WA (2010) Targeted Toxins in Brain Tumor Therapy. Toxins 2: 2645-2662.
- Peng Jing, Jian Li, Feng Gao, Yuanfei Lu, Jian Liu, et al. (2015) Use of hapten combined cytotoxic drugs for enhancing therapeutic effect in advanced stages of pancreatic cancer. Journal of Liver Research, Disorders & Therapy 1(3): 00013-0021.
- Eble JA, de Rezende FF (2014) Redox-relevant aspects of the extracellular matrix and its cellular contacts via integrins. Antioxid Redox Signal 20(13): 1977-1993.
- BaoFa Yu, Sinil Kim (1994) Alcohol with Intratumoral Drug Injection and Pharmacokinetics of Drug after Intratumoral Injection: A New Concept of Intratumoral therapeutic Coagulum with Drug Depots. Journal of Current Oncology 1(2): 97-100.
© 2020 Baofa yu MD. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






