- Submissions

Full Text
Novel Research in Sciences
Concepts About Open Globe and Closed Globe Injuries in The Current Classification of Ocular Trauma
B Shukla* and Facs Fams
Director of Research, India
*Corresponding author: B Shukla, Director of Research, RJN Ophthalmic Institute, Gwalior, India
Submission: June 12, 2020;Published: June 19, 2020
.jpg)
Volume4 Issue1June, 2020
Introduction
Current classification of ocular trauma has been made by Kuhn et al. [1]. All eye injuries are divided in open globe and closed globe types. To describe the outer covering of sclera and cornea they have used the term eye wall. Closed globe injuries are those in which there is no full thickness wound in the eye wall whereas in open globe type there is a full thickness wound in the eye wall. From a long time, eyeball injuries have been classified as perforating and non-peforating. In a perforating injury there is a full thickness wound of eyeball and not eye wall). In other words in perforation not only sclera but corresponding parts of choroid and retina are also perforated resulting in communication of the interior and the exterior of eye ball. This does not apply to corneal injuries.
Perforation is a word used in all surgical sciences like general surgery, E.N.T., and gynecology. Open globe is a new term devised for eyeball. Characteristics of a perforation is indicated by occurrence of a hole, loss of fluid (or gas), lowering of pressure and deformity in the shape of cavity and more chances of infection [2,3]. In the so called open globe there is no communication between the exterior and interior of the globe as choroid and retina are intact and there is no formation of any hole. In the anterior segment a hole in the cornea alone will result in perforation as there are tissue layers beneath. A small experiment was carried out to support this view. It was done on fresh goats’ eyeballs. I.O.P. recorded in different situations.
Material and Methods
Fresh goats’ eyes were procured. In one eye I.O.P. was measured by Perkins tonometer and average of three readings was recorded. Then a 2 mm by 2 mm hole was made only in the sclera and I.O.P. recorded. Lastly a hole was made in scleral bed consisting of choroid and retina and I.O.P. was again recorded. Lastly the scleral bed was also perforated by a needle and I.O.P. recorded in the same way. Same procedure was done in the second eye also, but the square scleral cut was 4 mm by 4 mm. A slightly bigger hole was made by a thicker needle in the scleral bed and IOP recorded.
Observations
The following observations were recorded
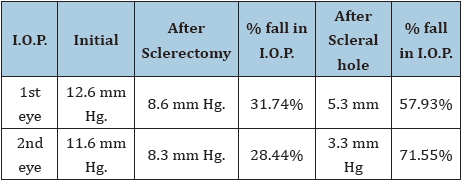
Initial IOP of 1st eye was 12.6 mm Hg and 2nd eye it was11.6 mm.Hg. After sclerectomy in 1st eye IOP was 8.6 mm Hg and in 2nd eye it was 8.3 mm Hg. % fall in IOP of 1st eye was 31.74% and in 2nd eye it was 28.44%. After scleral hole % fall in IOP in 1st eye was 57.93% and in the 2nd eye it was 71.55% and actual IOP was 5.3 mm in the 1st eye and 3.3 mm Hg. In the 2nd eye respectively Table 1.
Table 1:
Conclusion
After a hole in eyeball marked fall in I.O.P. was found. There was some fall in I.O.P. after sclerectomy also. In the 1st eye % fall of I.O.P. was 31.74% whereas in the 2nd eye it was % 28.44%. Difference between the two is little (3.3%). However, with a hole in the eyeball the fall in percentage is very high in both groups (57.93% in 1st eye and 71.55% in the 2nd eye). Thus, it is evident that after sclerectomy fall in I.O.P. was much less than hole in the eyeball. Open globe injury does not fulfill criteria of a perforating injury and hence its definition needs correction.
Acknowledgement
I wish to thank Dr. Ashish Dhage for recording the I.O.P. by Perkins handheld tonometer during the experiment. I also thank Mr. Vijay Birwal for preparation of the paper.
References
- F Kuhn, R Morris, C D Witherspoon, K Heimann, J B Jeffers et al. (1996) A Standardized Classification of Ocular Trauma. Ophthalmology 103: 240-243.
- Shukla B (2019) Basic concepts and confusion about ocular penetration and perforation. EC Ophthalmology 10: 6.
- Shukla B (2019) Limitations in the current classification of ocular trauma. Acta Scientific Ophthalmology 2(7): 23-25.
© 2020 B Shukla. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






