- Submissions

Full Text
Novel Research in Sciences
The Prevalence of Vitamin D Deficiency in ADHD-Affected Children and Adolescents in the Appalachian Region of Virginia
Shaily A Amin1*, Abul BMMKI2 and Anuradha Reddy1
1Dept. of Psychiatry, Virginia Tech Carilion School of Medicine, Roanoke, Virginia 24011. USA
2Dept. of Genetic Engineering and Biotechnology, University of Dhaka, Dhaka, Bangladesh
*Corresponding author: Shaily AA, Department of Psychiatry, USA
Submission: December 16, 2019;Published: February 07, 2020
.jpg)
Volume3 Issue3February, 2020
Abstract
Objective: To examine the prevalence of serum Vitamin D [Vit.D] insufficiency/deficiency in children/adolescents with ADHD in Roanoke City of the Appalachian region of Virginia.
Methods: The levels of Vit.D in the serum of 35 children/adolescents [with the diagnosis of ADHD [with or without comorbidities] were examined and divided into three groups: Cohort A [deficient levels of Vit.D (≤20ng/L)]; Cohort B [insufficient levels of Vit.D (21-29ng/L)] and Cohort C [sufficient levels of Vit.D (≥30ng/)].
Result: There was a significant (P≤06E-06) difference in serum Vit.D in Cohort A vs Cohort B. Additionally, the levels of Vit.D in Cohort A was significantly lower (P≤1.78E-09) when compared to ‘normal/required’ levels of Vit.D. Similarly, the levels of Vit.D was significantly lower (P≤2.89E-07) in Cohort B vs Cohort C.
Conclusion: 85% of ADHD-affected children/adolescents in the Appalachian region exhibited insufficiency/deficient level of Vit.D.
Introduction
The Appalachian Regional Commission (ARC) has reported a significantly higher general and mental health disparity [16%vs.8%] in the Appalachian region of Virginia as compared to the non-Appalachian part of the USA [1]. The below-par mental health conditions include high levels of Attention-Deficit/Hyperactivity Disorder [ADHD], Depression [MDD], Adverse Childhood Experience [ACE], Mood Disorder [MDX] and Generalized Anxiety Disorder [GAD] above national averages [1]. The average genetic association [[rg]=0.40] suggests a close genetic linked-trait among ADHD-affected brain and MDD, GAD, and bipolar disorder [2]. While symptoms of ADHD are first displayed in childhood, about 50% of children also meet the criteria of ADHD in adulthood [3]. Thus, ADHD occurs in about 2.5% of adults and twice the frequency [about 5%] is observed in children [4].
Deficiencies in Vit.D in animal models show abnormal growth of brain and neurons, enlarged ventricles, reduction in dopamine, NGF, and several neurotrophic factors, which are pathophysiological traits associated with mental health [5,6]. Vit.D deficiency [≤20ng/L], and insufficiency [≤30ng/L] are widespread in children and adolescent-mental ailments [5-7]. It seems the pleiotropic role of Vit.D is entwined in early brain development, onset and progression of clinical symptoms of ADHD [5-9]. The indispensable role of Vit.D, 1α-hydroxylase, and Vit.Dreceptors (VDR) are underappreciated in the regulation of tyrosine hydroxylase, dopamine, norepinephrine, and epinephrine. Vitamin D also regulates inflammation, neuronal survival, synaptic plasticity, and neuronal development in the human brain and psychiatric illnesses, such as ADHD, MDD, MDX, and GAD [5-9]. However, the relationship between Vit.D and ADHD has not received sufficient attention, if any, in the challenging health status in the Appalachian region of Virginia. Thus, in view of the approximately 66% of Vit.D insufficiency/deficiency in healthy children/adolescents in the USA [2,5], we examined the frequency of serum Vit.D in a small group of children and adolescents with ADHD and its comorbidities in Roanoke City at Carilion Clinic, which is located in the Appalachian region of South West Virginia. It is thus essential to improve our understanding of risk factors associated with ADHD-affected children/adolescents to better recognize, avert or treat the core disorder and its comorbidities.
Subjects and Study Cohorts
The medical records [from June 2018 to May 2019] of thirty-five patients with ADHD and related comorbidities [such as MDD, MDX, and GAD] were extracted using EPIC software at Carilion Clinic in Roanoke city. All the study subjects were from the outpatient clinic and had lab values of serum Vit.D drawn. The diagnosis of ADHD was made from a clinical interview and DSM-IV criteria and/or VADPRS. The comorbidities were diagnosed by the criteria described in the Diagnosis and Statistical Manual of Mental Disorders, Fifth Edition. The composition of the group consisted of subjects diagnosed with ADHD, 25.7%; ADHD+MDD, 28.5%; ADHD+GAD 28.5%; ADHD+GAD+MDX 11.4% and ADHD+GAD+MDD, 5.7%. There were 21 males (M) and 14 females (F) in the study. The group consisted of 60% Caucasians, 22.8% African Americans, 11.4% of biracial, and 5.7% of others, and an average age of 12.4±2.9. The group was divided into three Cohorts based on the levels of Vit.D in the serum as recommended [5-9]. Briefly, Cohort A consisted of 19 subjects with deficient levels of Vit.D [≤20ng/L]. Eleven subjects [in Cohort B] had insufficient levels [21-29ng/L] of serum Vit.D, whereas Cohort C consisted of 5 subjects with serum Vit.D levels of ≥30ng/L. Data were represented as the mean±standard deviation [with Students t-test and P values as required] using GraphPad Software (v1.14).
Result and Discussion
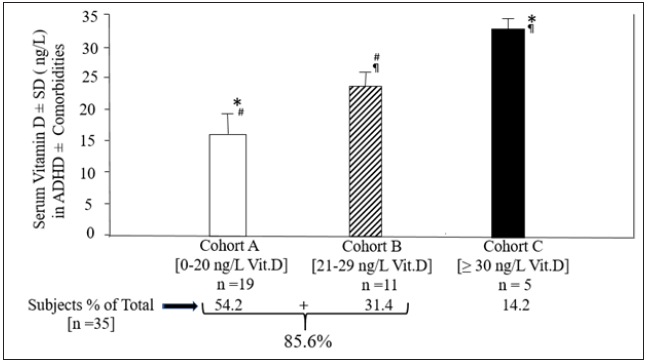
There was no significant [P≤0.3] difference in the average age of 21 males (12.0±3.4] and the 14 females [13.1±2.3]. Furthermore, there was no significant difference [P≤0.49] in the levels of Vit. D in all males [20.9±7.7ng/L] or females [20.2±5.4ng/L]. Thus, the data eliminated the age and sex-based bias in these cohorts. However, there was a significant (P≤1.06E-06) difference in the deficient levels of serum Vit.D in Cohort A [15.7±3.7ng/L] versus insufficient levels of Vit.D in Cohort B [23.4±2.0ng/L] as shown in (Figure 1). Furthermore, the deficient levels of Vit.D in Cohort A was significantly lower (P≤1.78E-09) when compared to ‘normal/required’ levels of Vit.D [33.0±1.7ng/L] in Cohort C. Similarly, the levels of Vit.D was significantly lower (P≤2.89E-07) in Cohort B vs Cohort C (Figure 1). This analysis shows that ~85% of ADHD-affected children and adolescents from the Roanoke city [population about 1 million] in the Appalachian region of Virginia exhibited insufficiency/deficient level of Vit.D irrespective of their racial distribution, age, and sex, as shown in Figure 1.
Figure 1: Comparison of vitamin D levels in ADHD±related comorbidities-affected children and adolescents
Our observation suggests that there may be a widespread occurrence of Vit.D deficiency/insufficiency in ADHD-affected children and adolescents in this region irrespective of the variable that is typically associated with levels of Vit. D across populations [2,5]. Our Cohort took into account the variables of age, males/ females, and socioeconomic status concerning levels of Vit.D. Furthermore, the racial distribution of our cohort was similar to the U.S Census [https://www.census.gov] for the city of Roanoke, Virginia. Several studies have also shown low levels of Vit.D in individuals with GAD, MDD, seasonal affective disorder [2,5]. The possibility that multidrug regimens in these subjects may inhibit Vit.D synthesis or absorption which cannot be ruled out [2,5].
These preliminary findings are alarming and raise a red flag because overall, the ADHD-affected children and adolescents exhibited a significant difference (average of 17.9±4.6ng/L) of Vit.D as compared to 33.0±1.7ng/L in the subject without ADHD. Long term and large epidemiological studies showed that deficient levels of Vit.D progressed towards osteomalacia and increased risk of hypertension, diabetes, and cardiovascular mortality [5,6]. Nevertheless, these conditions may be clinically manageable. Supplementing of [Vit.D or placebo] as adjunctive therapy to methylphenidate in ADHD-affected children and adolescents showed significant [P≤0.0009] improvement [based on CPRS and WCST scales] in cognitive tasks at the conceptual level, together with a decline in hyperactivity, inattention, and impulsivity [9-11]. An increment of 10ng/mL of Vit.D in the serum decreased symptoms of depression by 10% [5,6]. The claims on the improvement in mental health via supplementation of Vit.D are inconsistent and not robustly supported by all the research studies due to lack of controls for outside variables [5,6,8]. These include lack of statistical analysis, sample sizes, study design, acceptable clinical outcome scales, and/or consideration of genetic and epigenetic factors in investigations [5,6,8-10]. The exact mechanism(s) of action of Vit.D in the ADHD-affected brain remains elusive [8]. However, several theories suggest Vit.D may augment dopamine signaling that regulates the tonic excitatory drive and regulates the frequency of brain rhythms. Vitamin D is known to activate neural circuits involved in the symptoms of ADHD [8].
The small sample size, lack of data on risk factors like dietary habits, and exposure to sunlight/day of the cohorts are the main limitations of this preliminary investigation. It may be prudent to plan and execute for more controlled, extensive evidence-based studies, across all hospitals in Southwest Virginia in the future [7,8]. The future study can also be designed to examine ADHDaffected children and adolescents using WPREMB, CPRS, and ADHD-RS scales, and optimal support strategies before and after supplementation of Vit.D [8-10]. The outcomes will provide a better clinical result on the effect of Vit.D on ADHD-affected children and adolescents in the region.
Limitation and Conclusion
The clinical perspective of these observations suggests that Vit.D insufficiency/deficiency in ADHD-affected children and adolescents [with and without other comorbidities] may be widespread in the challenging conditions in the Appalachian region. Similar to the high incidence [78-91%] of Vit.D insufficiency/ deficiency as reported in Iran and Saudi Arabia [5,6]. While a Vit.D guideline exists for management of Vit.D deficiency for bone health, there are no guidelines currently available for the use of Vit.D as adjunctive therapy for Psychiatry [5,6]. Vitamin D sufficiency/ deficiency is frequently overlooked in the clinic where USPSTF does not recommend universal screening of Vit.D [5,6]. However, Vit.D may play a paramount role in individuals diagnosed with ADHD. Despite the current limitations of the study described above, these preliminary observations not only warren a more extensive study but also consider a cautionary change in the policies and procedures in hospitals across the region. These changes may include not only the diagnosis of Vit.D levels of all subjects diagnosed with ADHD and related comorbidities but also the initiation of programs [with close monitering] to establish oral supplementation of Vit.D [9-11]. Although exposure to sunlight plays a critical role in sustaining the level of Vit.D, it may not be sufficient to alleviate Vit.D deficiency due to other variables [5,6]. Oral supplementation of 5000U/day or 50,000U/week has shown to improve deficient levels of Vit.D to sufficient levels in the blood [9-11]. These changes in policies may also be a starting point to ease the concerns of most patients with ADHD who are resistant to treatment with stimulant medications.
The figure shows a comparison between the three Cohorts [Cohort A, n=19; Cohort B, n=11; and Cohort C, n=5] with three different concentrations of serum Vit.D respectively in 35 study subjects with ADHD± related comorbidities. The data are expressed as mean± SD for each Cohort. Students t-test was performed for statistical analysis and the significant difference between two representative Cohorts are *P≤1.78E-09; #P≤1.06E-06; ¶P≤2.89E-07. This study was presented as an abstract and poster at the American Academy of Child and Adolescent Psychiatry’s 66th Annual Meeting in Chicago on October 14-19, 2019.
References
- McGarvey EL, Verdin MLL, Killos LF, Guterbock T, Cohn WF (2011) Health disparities between appalachian and non-appalachian counties in Virginia, USA. J Community Health 36(3): 348-356.
- Anttila V, Sullivan BB, Finucane HK, Walters RK, Bras J, et al. (2018) Analysis of shared heritability in common disorders of the brain. Science 360(6395): eaap8757.
- Lara C, Fayyad J, DeGraaf R, Kessler RC, Gaxiola AS, et al. (2009) Childhood predictors of adult attention-deficit/hyperactivity disorder: Results from the world health organization world mental health survey initiative. Biol Psychiatry 65(1): 46-54.
- Sadock BJ, Sadock VA, Ruiz P (2014) Kaplan and Sadock’s synopsis of psychiatry: In: (11th edn) Behavioral sciences/clinical psychiatry, Lippincott Williams & Wilkins, Philadelphia, USA, p. 1472.
- Harris HW, Jaiswal P, Holmes V, Weisler RH, Patkar AA (2013) Vitamin D deficiency and psychiatric illnesses. Current Psychiatry 12(4): 19-24.
- Mulcahy K, Trigoboff E, Opler L, Demler B (2016) Physicians prescribing practices of vitamin D in a psychiatric hospital. Innov Clin Neurosci 13(5-6): 21-27.
- Khoshbakht Y, Bidaki R, Abargouei AS (2018) Vitamin D status and attention deficit hyperactivity disorder: A systematic review and meta-analysis of observational studies. Adv Nutr 9(1): 9-20.
- Saedisomeolia A, Samadi M, Gholami F, Seyedi M, Effatpanah M, et al. (2018) Vitamin D's molecular action mechanism in attention-deficit/ hyperactivity disorder: A review of evidence. CNS Neurol Disord Drug Targets 17(4): 280-290.
- Elshorbagy HH, Berseem NF, Abdelghani WE, Suliman HI, Shokary AH, et al. (2018) Impact of vitamin D supplementation on attention-deficit hyperactivity disorder in children. Ann Pharmacother 52(7): 623-631.
- Dehbokri N, Noorazar G, Ghaffari A, Mehdizadeh G, Sarbakhsh P, et al. (2019) Effect of vitamin D treatment in children with attention-deficit hyperactivity disorder. World J Pediatr 15(1): 78-84.
- Mohammadpour N, Jazayeri S, Djalali M, Hosseini M, Effatpanah M, et al. (2018) Effect of vitamin D supplementation as adjunctive therapy to methylphenidate on ADHD symptoms: A randomized, double-blind, placebo-controlled trial. Nutr Neurosci 21(3): 202-209.
© 2020 Shaily A Amin. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






