- Submissions

Full Text
Novel Practices in Medical Study
An Uncommon Cause of Palpitations: Chilaiditi’s Syndrome
Vera Seara* and Inês Burmester
Internal Medicine Department, Póvoa De Varzim/Vila Do Conde Hospital Centre, Póvoa De Varzim, Portugal
*Corresponding author: Vera Seara, Internal Medicine Department, Póvoa De Varzim/Vila Do Conde Hospital Centre, Praça Dr. António José de Almeida, 4480- 777 Vila Do Conde, Portugal
Submission: November 09, 2022 Published: December 16, 2022

NPMSVolume1 Issue2
Abstract
Chilaiditi’s syndrome refers to the interposition of the colon between the diaphragm and the liver, accompanied with clinical symptoms. Usually a benign condition, with symptomatic approach and rare surgical indication. The authors describe a case report of Chilaiditi syndrome in a young adult presenting with palpitations.
Keywords: Pseudopneumoperitoneum; Chilaiditis syndrome
Introduction
Chilaiditi syndrome is a rare finding, with prevalence described between 0.025 and 0.28% [1]. In most patients, it is asymptomatic and is often an incidental finding, denominated as the Chilaiditi sign [2]. This entity requires the presence of abnormal gaseous interposition of the colon between the liver and the diaphragm. As the elevation of the right hemidiaphragm occurs, the colon (identified by the presence of haustra) is interposed between the diaphragm and the liver. The superior hepatic border is positioned inferior to the left diaphragm [2].
Case Report
Figure 1: Chest (A) and abdomen (B) X-ray: presence of Chilaiditi. Blue arrow: colon (haustras visible). White arrow: hemidiaphragm. Asterisk: superior hepatic border.
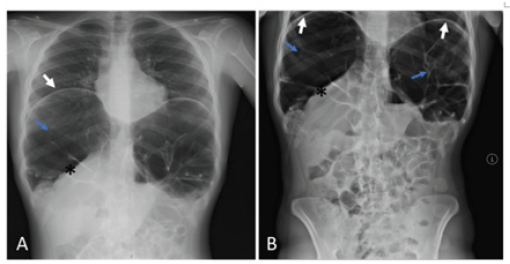
Chilaiditi syndrome is an uncommon condition, being described in 0.025%-0.28% of the population [1] An 18-year-old female, with no relevant personal history or usual medication is admitted at the emergency department with complaints of palpitations and mild abdominal pain. On physical examination, she is hemodynamically stable, sinus tachycardia with heart rate of 126bpm and abdominal pain discomfort in palpation, without signs of peritoneal irritation. Chest and abdomen X-ray shows Chilaiditi’s sign (Figure 1), with no other abnormalities. Electrocardiogram confirmed sinus rhythm. Consulted by general surgery, which excluded the presence of an acute abdomen. She was kept under surveillance and started fluid therapy and enemas. After bowel cleansing, the patient remained asymptomatic and without recurrence of tachycardia. She was discharged from hospital, with symptomatic medication, laxatives and referred to nutrition outpatient consult.
Discussion
Chilaiditi syndrome is accompanied by symptoms related to the digestive system, namely nausea, dyspepsia, constipation, abdominal pain, or intestinal obstruction secondary to intestinal volvulus [3]. Cardiovascular symptoms are less common, with tachycardia, arrhythmias and angina-like chest pain being reported [1,4]. The origin of Chilaiditi’s sign is unknown, but it may be secondary to congenital or acquired conditions. Congenital conditions include laxity or absence of hepatic suspensory ligaments, colic redundancy, or paralysis of the right diaphragm [4,5]. In acquired conditions, risk factors such as liver atrophy secondary to cirrhosis, ascites, obesity, or chronic constipation are the most identified factors [3,4]. In the presence of Chilaiditi syndrome, the initial approach is conservative, with fluids, decompression through a nasogastric tube, laxatives and enemas, and a high-fibre diet; in more severe cases, surgical intervention may be necessary in the presence of ischemia or secondary intestinal perforation [3].
Conclusion
The rarity of the disease, along with variations in clinical presentation, often results in misdiagnosis. Recognizing this syndrome is important in differential diagnosis with pneumoperitoneum, since the approach is conservative, in opposition of the pneumoperitoneum, which can lead to unnecessary invasive interventions.
References
- Kapania EM, Link C, Eberhardt JM (2018) Chilaiditi syndrome: A case report highlighting the intermittent nature of the disease. Case Rep Med.
- Sachdev MSB, Mahadzir MDA, Lee TC (2018) Chilaiditi's sign, a cause of pseudo-pneumoperitoneum: A case report. SAGE Open Med Case Rep.
- National Organization for Rare Disorders (NORD) Chilaiditi syndrome. In Chilaiditi's Syndrome - NORD (National Organization for Rare Disorders).
- Erdem SB, Nacaroglu HT, Canan SUK, Alper H, Demet C (2015) Chilaiditi Syndrome in two cases presented with respiratory distress symptoms. Turk Thorac J.
- Sureka B, Bansal K, Arora A (2015) Pneumoperitoneum: What to look for in a radiograph?. J Family Med Prim Care 4(3): 477-478.
© 2022. Vera Seara. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






