- Submissions

Full Text
Novel Approaches in Cancer Study
Sphenoidal Chondrosarcoma-Review of Literature of a Rare Case
Rajaram Sharma1*, Rinkey Baisoya2, Tapendra N Tiwari1 and Saurabh Goyal1
1Assistant Professor, Department of Radiodiagnosis, Pacific Institute of Medical Sciences, Umarda, Udaipur, Rajasthan, India.
2Resident Doctor, Department of Radiodiagnosis, Pacific Institute of Medical Sciences Umarda, Udaipur, Rajasthan, India
*Corresponding author:Rajaram Sharma, Assistant Professor, Department of Radiodiagnosis, Pacific Institute of Medical Sciences, Umarda, Udaipur, Rajasthan, India.
Submission: July 11, 2022 Published: July 21, 2022

ISSN:2637-773XVolume7 Issue2
Abstract
Background:Chondrosarcoma is an unsual tumour involving the skull base. This malignant tumour most commonly occurs in young adults, and it is found in countless anatomic locations, including long bones, flat bones, and craniofacial bones. It is necessary to distinguish myxoid chondrosarcoma from the chondroid variant of chordoma, as the treatment protocol and prognosis varies for both conditions.
Case report: A 30-year-old female came to our hospital with a complaint of right nasal obstruction for the past few months. The patient underwent a Computed Tomography(CT) scan of paranasal sinuses including base of skull was ordered. The CT scan revealed a well-defined lobulated hypodense soft tissue density mass lesion centered in the body of the sphenoid bone. The mass had internal ring and arc type of calcification. The mass was filling the sphenoid sinus, whole right sided ethmoidal sinuses, and eroding the skull base to reach into the extra-dural space. Mass was extending into medial part of right orbit causing compression of the medial rectus muscle and resulting in lateral side proptosis. Post obstructive sinusitis changes were observed in right frontal and maxillary sinuses. The patient underwent surgical management.
Conclusion: Sphenoidal chondrosarcoma is a rare entity; misdiagnosing it or missing the findings may have profound implications for the patient. CT provides an accurate and detailed depiction of the entity.
Keywords: Sphenoidal; Chondrosarcoma; Malignant
Introduction
Chondrosarcoma is a highly destructive malignant tumour, mainly cartilaginous, and sometimes bone or mesenchymal in origin. Its localization in the head and neck, particularly in the sphenoid sinus site, is rarer. The reported case describes the tumour involving base of the skull, maxillary sinus and sphenoidal sinuses. Symptoms presented by this condition are non-specific. We, at this moment present a case of chondrosarcoma of the sphenoid sinus with an aim to describe the clinical, radiological and anatomo-pathological profile and treatment of this pathological condition. Chondrosarcoma is an unsual tumour involving the skull base [1]. The global incidence is reported to be in 200,000 per year, and it is the third most frequent malignant bone tumour after multiple myeloma and osteosarcoma. This malignant tumour most commonly occurs in young adults, and it is found in countless anatomic locations, including long bones, flat bones, and craniofacial bones [2]. It is necessary to distinguish myxoid chondrosarcoma from the chondroid variant of chordoma, as the treatment protocol and prognosis varies for both conditions..
Case Presentation
A 30-year-old female came to our hospital with a complaint of right nasal obstruction and throbbing headache behind the eye for the past few months. She didn’t had any other associated complaints. General examination was unremarkable and vital were within normal limits. On her physical examination, it was noted that nasal flow was reduced on both sides, more on the right side (Figure 1). Diagnostic nasal endoscopy was done, which showed a budding polyploid mass, occupying the right nasal fossa which was pedicled in the sphenoid sinus. Basic blood investigations came out normal. For further evalution and better delineation of the pathology, a Computed Tomography (CT) scan of paranasal sinuses including base of skull was ordered. The CT scan revealed a well-defined lobulated hypodense soft tissue density mass lesion centered in the body of the sphenoid bone. The mass had internal ring and arc type of calcification. The mass was filling the sphenoid sinus ,whole right sided ethmoidal sinuses, and eroding the skull base to reach into the extra-dural space. Mass was extending into medial part of right orbit casuing compression of the medial rectus muscle and resulting in lateral side proptosis. Post obstructive sinusitis changes were observed in right frontal and maxillary sinuses.
Figure 1: (A&B) Non- Enhanced Computed Tomography (NECT) of head including Paranasal Sinuses (PNS), soft tissue window coronal plane and axial plane demonstrate a soft tissue density mass with punctate matrix calcification (white arrow) involving sphenoid bone and extending anteriorly to the nasopharynx and nasal cavity (black arrow). Laterally, on right side the mass is seen involving posterior maxillary walls and extending into right maxillary sinus. (C&D) NECT of head including PNS, bone window, axial plane and sagittal plane demonstrate anteriorly projecting mass with internal punctate matrix calcification (white arrow) involving sphenoid bone and extension into the nasopharynx, posterior nasal cavity. There is destruction of the bones of both maxillary sinuses, posterior part of the nasal septum (black arrow) and right side of petrous bone.

Treatment
The endoscopic way is the first choice of the treatment of sphenoid chondrosarcomas [3]. Because of the involvement of paranasal sinuses and extra dural extension, wide resection couldnt be done, and limited removal was advised to avoid complications. After debulking (for safer irradiation away from surrounding critical organs) patient was referred for radiotherapy. The patent is doinf fine till writing of this report.
Discussion
Chondrosarcoma is a malignant tumour, and it accounts for 20% of malignant bone tumors [4]. The incidence of the lesion increases with age. The mean age for chondrosarcoma is in the fourth decade [5], with a clear predominance among women [6]. Chondrosarcomas tend to be significantly larger in size at the time of presentation [7]. Symptoms of the tumours depend on the site and size and vary according to the adjacent involvement and extension. The most common presentations include nasal obstruction, nasal discharge, and headache (Figure 2). Extension of tumour towards the orbit can lead to facial asymmetry, restricted ocular movements, diplopia, proptosis, and facial pain. The intracranial extension of the lesion characterized by loss of vision, proptosis and multiple cranial nerve involvement [8]. Radiology plays an essential role in identifying and localizing the lesion before surgery. CT scan mainly helps determine the site, size, and extension of the tumour, allowing surgeons to adequately resecte the tumour. Axial, reformatted coronal and sagittal planes along with 3-dimensional CT images detailed information regarding the lesion [9]. The CT scan alos better for describing the interal pattern of calcification. Main role of MRI is to identify soft tissue extension and involvement of areas adjacent to the tumour. The MRI classifies and differentiates between post-operative granulation tissue and recurrences [10].
Figure 2: Histopathology image demonstrate abundant cartilaginous matrix with chondrocytes embedded. obvious atypia of nucleus and pleomorphism is also noted.
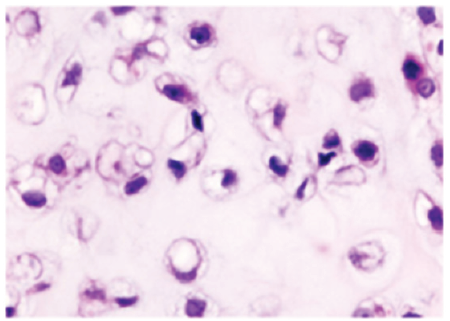
Chondrosarcoma originates either from primitive mesenchymal stem cells or tissue known to be formed of cartilage nests that remain after ossification. The gross appearance of the tumour is a well-circumscribed, round-ovoid, lobular and gelatinous mass. A fibrous capsule or internal haemorrhage may be present. The tumour size may vary, but the average size of the lesion is usually 3-8cm at the time of presentation [11]. Grading of lesions is based on two essential factors: Cartilage amount, maturity and connective tissue anaplasticity. According to these, they are subdivided into three types: classic, myxoid and mesenchymal. Secondly, as per the World Health Organization (WHO) classification system, they are classified into three grades based on degree of differentiation. Grade I is well-differentiated, grade II is moderately differentiated and grade III is poorly differentiated [12]. Histological grading depends on cellularity, nuclear size and the mitotic rate and found to correlate better with the pace of distant metastasis and overall survival [13]. The tumour’s histological appearance helps us make a differential diagnosis of chondroma, chordoma, and chondromyxoid fibroma. Fine needle biopsy or even an excision biopsy is not fully reliable as the specimen may not represent the actual lesion as areas of cellular atypism are restricted [14]. Multiple field evaluation is necessary for grading this tumour [15].
Mainstay of treatment remains surgery. Due to the frequent surrounding extension of the tumour, maximal surgery is required in the chondrosarcomas. Due to high complications related to the surgery, various supportive interventions are often needed. The first choice of treatment for the sphenoid chondrosarcoma is via endoscopic route [16]. Due to the locoregional extension of the tumour, wide resection is difficult to achieve. Limited part of the tumour can be resected to avoid complications. A large debulking with adjuvant radiation therapy has also been described. Surgery, as well as adjuvant chemotherapy, provide the excellent result as compared to surgery alone [17].
Diffrential Diagnosis
Anteriorly projecting sphenoidal mass with internal punctate (chondroid type) matrix calcification differentiates the sphenoidal chondrosarcoma to other entity such as chordoma, meningioma and metastasis.
Conclusion
Sphenoid bone chondrosarcoma is a rare malignant tumour. Symptoms mainly depend on the site and the extension. CT and MRI both help diagnose and map-out the lesion. MRI plays a crucial role in making the diagnosis. The main treatment is surgery, and radiotherapy. NCCT Head including paranasal sinuses should be the ideal investigation for chronic headache associated with nasal and ophthalmic symptoms. Soft tissue density mass of bony origin with punctate matrix calcification is the diagnostic of chondrosarcoma. CT also plays imperative role in pre-surgical planning to evaluate the disease extension.
References
- CBTRUS (2005) Central brain tumor registry of the United States 2005-2006.
- Unni K, Inwards C (2009) Dahlin’s bone tumours. (6th edn), p. 416.
- Guo L, Liu J, Sun X, Wang D (2014) Sinonasal tract chondrosarcoma: 18-year experience at a single institution. Auris Nasus Larynx 41(3): 290-293.
- Pontes H, Pontes F, Abreu M, Carvalho P, Brito Kato A, et al. (2012) Clinicopathological analysis of head and neck chondrosarcoma: three case reports and literature review. Int J Oral Maxillofac Surg 41(2): 203-210.
- Fu Y, Perzin K (1974) Non-epithelial tumours of the nasal cavity, paranasal sinuses, and nasopharynx: a clinicopathologic study 3. Cartilaginous tumours (chondroma, Chondrosarcoma). Cancer 34(2): 453-463.
- Koch B, Karnell L, Hoffman H, Apostolakis L, Robinson R, et al. (2000) National cancer database report on Chondrosarcoma of the head and neck. Head Neck 22(4): 408-425.
- Sharma K, Kaur A, Taneja HC, Tyagi I, Pandey R (1993) Nasal septal chondrosarcoma with visual loss. Indian J Ophthalmol 41(4): 189-191.
- Jaswal A, Jana AK, Sikder B (2008) Chondrosarcoma of the nose and paranasal sinus- a rare presentation. Indian J Otolaryngol Head Neck Surg 60(3): 284-286.
- Lioyd G, Lund VJ, Howard D, Savy L (2000) Optimum imaging for sinonasal malignancy. J Laryngol Otol 114(7): 557-562.
- Kavita S, Neeraj S (2016) Myxoid chondrosarcoma of nasomaxilloethmoid region with intracranial extension. Indian J Otolaryngol Head Neck Surg 68(1): 110-114.
- Evans HL, Ayala AG, Romsdahl MM (1977) Prognostic factors in chondrosarcoma of bone: a clinicopathologic analysis with emphasis on histologic grading. Cancer 40(2): 818-831.
- Ashley DJB (1990) Temperomandibular juxta-articular chondroma: case report. In: Evans’ histological appearance of tumours, 4th (edn), London, UK, pp. 133-139.
- Alho A, Connor JF, Mankin HJ (1983) Assessment of malignancy of cartilaginous tumours using flow cytometry. A preliminaw report. J Bone Joint surg 65(6): 779-785.
- Guo L, Liu J, Sun X, Wang D (2014) Sinonasal tract chondrosarcoma: 18-year experience at a single institution. Auris Nasus Larynx 41(3): 290-293.
- Boskos C, Feuvret L, Noel G (2009) Combined proton, and photon conformal radiotherapy for intracranial atypical and malignant meningioma. Int J Radiate Oncol Biol Phys 75(2): 399-406.
- Georges N, Vinai G (2016) Proton therapy for tumours of the base of the skull Chinese clinical oncology. Chin Clin Oncol 5(4): 51.
- Ruark DS, Schlehaider UK, Shah JP (1992) Chondrosarcomas of the head and neck. World J Surg 16(5): 1010-1016.
© 2022. Rajaram Sharma. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






