- Submissions

Full Text
Novel Approaches in Cancer Study
Management of an Oncology Patient who Developed Complications During Tube Thoracostomy in the Emergency Department
Serhat Orun1*, Mithat Fazlıoglu2, Batuhan Ilbey Basol1 and Muhammet Talha Aygun1
1Department of Emergency Medicine, Turkey
2Department of Thoracis Surgery, Turkey
*Corresponding author: Serhat Orun, Faculty of Medicine, Department of Emergency Medicine, Tekirdag, Turkey
Submission: April 18, 2022 Published: May 11, 2022

ISSN:2637-773XVolume7 Issue1
Abstract
Cancer patients are a special patient group that is more risky than other patient populations and should be approached more carefully. Especially in lung cancer patients, conditions such as tube thoracostomy required for empyema evacuation can lead to serious complications. The complication risk of tube thoracostomy procedure (19%), which is also present in the normal population, increases in oncology patients as a result of the changing anatomy, immune system and metabolic deficiencies. In addition, the management of these complications is not common. In this case, we aimed to present the complication that occurred during tube thoracostomy in a patient with squamous cell lung malignancy and our experience in the management of this complication.
Keywords: Emergency department; Lung cancer; Tube thoracostomy; Complication management; Prolonged CPR
Introduction
Lung cancer is the 2nd most common type of cancer among all cancers and the 1st in deaths due to malignanc [1]. Serious complications may be encountered in these cancer patients whose major risk factor is smoking. In addition, complications occur during risky invasive procedures applied to eliminate existing complications. One of these risky procedures is tube thoracostomy. Although an average complication risk of 19% is predicted for tube thoracostomy, the results can be fatal. These complications are most common in patients with empyema and diabetes mellitus [2]. Our aim in presenting this case is to convey the complication that occurred during tube thoracostomy in a patient with lung malignancy and our experience in the management of this complication [3].
Case
A 76-year-old male patient applied to our emergency department with the complaint of cough. In his anamnesis, it was learned that he was diagnosed with squamous cell lung cancer and a lobectomy operation was performed on the left lower lobe of the lung 1 month ago. The patient, who applied to the external health center with the complaint of fever and cough, was referred to our hospital as an outpatient. Fever was present for 4 days. Cough had been chronic for about 3 months. There was sputum production in white color. Vital signs; blood pressure: 140/80mmHg, pulse: 62 min Sat O2: 91% Fever: 37.0 ℃. The general condition of the patient was good, conscious, oriented and cooperative, GCS: 15. On physical examination, lung sounds were decreased in the left lobe, and lung sounds were not heard especially in the left lower lobe of the lung. Other system examinations were normal. Hemogram, biochemistry and coagulation tests were requested from the patient. Chest X-ray and uncontrasted thorax Computed Tomography (CT) taken at an external center on the same day were examined, thoracic surgery consultation was requested with the preliminary diagnosis of empyema.
After the evaluation, tube thoracostomy procedure was started by the thoracic surgeon. During the procedure, a sudden flow of approximately 1000cc of hemorrhagic fluid was observed from the inserted thorax tube. Rapid deterioration in the general condition of the patient was observed. In the vital signs of the patient who lost consciousness, ta: 60/30mmHg nb: 120 min sato2: 80%. The thorax tube was clamped and the flow was stopped. Immediately afterwards, the patient developed cardiopulmonary arrest, which was thought to be due to hypovolemic shock.
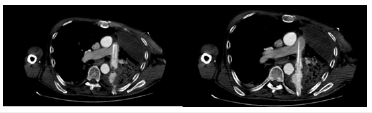
The patient was started on Advanced Cardiac Life Support (ADHS). Endotracheal intubation was performed. Bolus crystalloid isotonic fluid was started in the open vascular access to the patient. Since the patient had difficulty in opening the second vascular access, 2 intraosseous lines were opened to the patient. Bolus saline and 0 rh(-) erythrocyte suspension were given intraosseously. Blood group and cross match were studied from the blood sample taken at the time of application. At the same time, the patient’s vascular bed started to expand, and a second iv vascular access was opened through the external jugular vein under the guidance of ultrasonography. Until this stage, 4 units of 0 rh(-) erythrocyte suspension and 3500cc of physiological saline were administered to the patient. Spontaneous cardiac beat occurred in the patient after 90 minutes of ADHS. In his vital signs, blood pressure: 80/50 mmHg, nb:100/min satO2% was 88%. Dopamine IV infusion was administered to the patient. The patient was transferred to the intensive care unit for further examination and treatment. Here, after the patient stabilized, thoracic angiography was performed, it was seen that the thorax tube placed in the CT was in the main pulmonary artery. The patient was taken to an emergency thoracotomy, but it resulted in death during the procedure (Figure 1).
Figure 1:
Discussion
Invasive procedures in oncology patients are more risky in terms of complication development compared to the non-oncology patient group. The underlying causes of this situation include various factors such as altered anatomy after chemotherapy, radiotherapy and surgery, immunosuppression, and the patient’s metabolic status. Tube thoracostomy is one of these invasive procedures.
According to a study by Vilkki et al. [3] complications developed in 19.9% of 1169 patients who were followed up with a thoracic tube, and malposition in the tube was corrected in 7% of these patients with non-emergency operations. In the same study, it was stated that tube thoracostomy performed in patients with empyema caused more complications. In addition, it has been reported that CH16 tubes cause less complications than CH22 tubes [3].
According to a meta-analysis by Hernandez et al. [2] the complication rate in 4981 patients who underwent tube thoracostomy was 19%, and 15% of these complications were during insertion, 53% were positional, 16% were during extraction, 15% were immunological, 1% were and the other one is due to malfunction. According to the study of Maezawa et al. [4] 107 tube thoracostomy procedures performed, 8 patients’ tube-related complications (7.8%), and 4 had limited and 4 had unresolved hemothorax. This has led to the conclusion that small tubes (under 20 french) can perform the same function with low complication rates.
In the study by Kesieme et al. [5] intense pleural adhesion was found in the pleural area in all patients with pulmonary artery injury, and it was stated that this change caused the tube to enter the pulmonary artery, not the pleural area. There are different approaches in the management of these complications. Kao et al states that the definitive solution to the repair of these complications is surgery. Sundaramurthy et al. [6] a non-surgical management was recommended by in this procedure, after the thorax tube is clamped, the tube is slowly withdrawn after a certain period of time. It was stated that the perforated area of the pulmonary artery can be occluded by the thrombus present in the environment [7].
In our patient, it was decided to apply tube thoracostomy to drain the empyema. During the process, a 22CH size tube was used. We also think that choosing small tubes during tube thoracostomy will reduce complications. In addition, we think that the mediastinal anatomy may change in patients who underwent lobectomy, and this may change the localization of the left pulmonary artery. This anatomical change increases the risk of complications. Therefore, the anatomy of the area to be treated should be evaluated in detail before the interventional procedure in oncology patients. We think that simultaneous imaging techniques may be useful for this. Again, due to the possible risk of complications, we think that blood group and crossmatch study before the procedure in all of these patients will help emergency physicians in the management of CPR.
As a conclusion, the risk of complications during interventional procedures in oncology patients may increase due to various factors, therefore, we think that approaches that include instant imaging techniques instead of routine approaches to interventional procedures in oncology patients may reduce the risk of complications.
References
- Schabath MB, Cote ML (2019) Cancer progress and priorities: Lung cancer. Cancer Epidemiol Biomarkers Prev 28(10): 1563-1579.
- Hernandez MC, Khatib M, Prokop L, Zielinski MD, Aho JM (2018) Complications in tube thoracostomy: Systematic review and meta-analysis. J Trauma Acute Care Surg 85(2): 410-416.
- Vilkki VA, Gunn JM (2020) Complications related to tube thoracostomy in Southwest Finland hospital district between 2004 and 2014. Scand J Surg 109(4): 314-319.
- Maezawa T, Yanai M, Huh JY, Ariyoshi K (2020) Effectiveness and safety of small-bore tube thoracostomy (≤20 Fr) for chest trauma patients: A retrospective observational study. Am J Emerg Med 38(12):2658-2660.
- Kesieme EB, Dongo A, Ezemba N, Irekpita E, Jebbin N, et al. (2012) Tube thoracostomy: complications and its management. Pulm Med 2012: 256878.
- Kao CL MD, Lu MS, Chang JP (2007) Successful management of pulmonary artery perforation after chest tube insertion. The Journal of Trauma 62(6): 1533.
- Sundaramurthy SR, Moshinsky RA, Smith JA (2009) Non-operative management of tube thoracostomy induced pulmonary artery injury. Interact Cardiovasc Thorac Surg 9(4): 759-760.
© 2022. Serhat Orun. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






