- Submissions

Full Text
Novel Approaches in Cancer Study
A Strange Association Between A Rectum- Infiltrating / Metastatic Dedifferentiated Chordoma And Schmidt’s Syndrome
Endrit Shahini, Elena Maldi and Teresa Staiano*
FPO-IRCCS Candiolo Cancer Institute, Italy
*Corresponding author:Teresa Staiano, FPO-IRCCS Candiolo Cancer Institute Candiolo, Italy
Submission: September 12, 2019;Published: November 06, 2019

ISSN:2637-773XVolume3 Issue5
Abstract
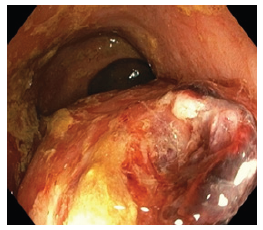
A 57-year-old Caucasian woman, presented to our Endoscopy Unit, complaining several episodes of rectal bleeding during the last 2 weeks, associated with lower abdominal and back pain, mild weight loss and asthenia. On presentation, the patient was hemodynamically stable. Her laboratory tests showed normocytic anemia of 10g/dL, increase of creatine chinase of 264U/L, and mild hypopotassemia (3.4 mEq/l). Moreover, she reported a family history for gastric cancer (father), and she was surveilled by our Oncological center for a recurrent neoplastic disease and for a systemic autoimmune disease, for many years stable under treatment with cycles of radiotherapy, imatinib mesylate, steroids, levothyroxine, and semestral zoledronic acid. After she underwent flexible sigmoidoscopy, a bulky ulcerated rectal mass, of suspected extraparietal origin, was revealed in (Figure 1) and (Figure 2). Multiple random biopsies were obtained from the normal mucosa as well as separately from the ulcers.
Figure 1:Endoscopic appearance of the ulcerated rectal mass, before the random biopsies performed from the normal mucosa
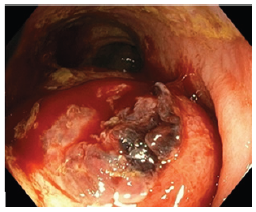
Figure 2:Endoscopic appearance of the ulcerated rectal mass, after the random biopsies performed from the normal mucosa
What is the most likely diagnosis?
Answer to: Image 3 - A Strange Association Between a Rectum- Infiltrating/Metastatic Dedifferentiated Chordoma and Schmidt’s Syndrome.
Figure 3:Rectal infiltrating chordoma on histology (H&E stain, 20x).
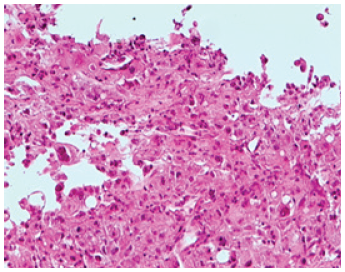
Figure 4:On immunochemistry Anti-Pancitocheratin antibody (AE1/AE3), S100, EMA, and vimentin were intensely and diffusely positive; anti-CDX2 antibody showed a weak/focal positivity (10x).
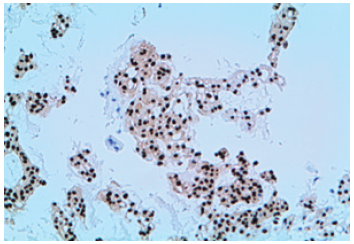
Histological specimens obtained from endoscopic biopsies showed clusters of medium/large-sized epithelioid cells, with abundant clear cytoplasm and round nuclei, suggestive of a pleomorphic mesenchymal neoplasia (Figure 3, H&E stain, 20x). This finding was further confirmed by immunohistochemistry studies with Brachyury antibody, which showed a strong and homogeneous nuclear positivity (Figure 4). A diagnosis of dedifferentiated chordoma was finally endorsed. At the age of 43-years, the patient underwent en-bloc sacrectomy for a large sacral mass (90x60x40mm). A postoperative diagnosis of dedifferentiated chordoma, was gained and she underwent pelvic radiotherapy (33 cycles, DFT=59.4Gy) [1,2]. Concurrently, she started steroid therapy when Schmidt’s Syndrome (autoimmune polyendocrine syndrome type 2) was diagnosed. When 5 years later disease stability was achieved, on computed tomographic (CT)/ Positron Emission Tomography (PET) investigations was shown a sacral recurrence of a bulky lesion (60x35mm). After imatinib mesylate therapy (600mg/day) was added, reaching disease stability within 15 months, the pelvic mass was surgically resected. Two years later, another local disease recurrence with “de-novo” lung metastasis [3], were treated with 10 months Cisplatin cycles (30mg/mq, -25%), additionally to pelvic radiotherapy (5 cycles, DFT=20Gy), and 6 months later imatinib mesylate was steadily used as maintenance therapy (300-600mg/daily).
Despite initial local/systemic disease progression, within 43 months of well-tolerated therapy, the disease recurrences were considered dimensionally unchanged. When an ulcerated rectal mass was diagnosed on endoscopic assessment after the onset of rectal bleeding episodes, the next abdomen/pelvic MRI and CT scan imaging, revealed an increase of the pelvic mass (77mm), which surrounded the back wall of the distal rectum, compressing and infiltrating it longitudinally for 50mm, with further infiltration of the posterior wall of the vagina. On the next 4 months our patient was conservatively managed (laxatives and iron replacement therapy), and rectal bleeding improved 2 weeks later without any recurrences, whereas tranexamic acid was used for treating few episodes of vaginal blood losses. As suggested by literature, a combination of surgical resection with adjuvant radiotherapy allows a good overall survival, local and distant relapse free survival in these patients, whereas imatinib is suggested for their nonsurgical management.1-3 Currently, there are no data on the most appropriate endoscopic treatment in cases of rectal bleeding due to the local advanced disease progression. New studies are warranted on this topic.
Author contributions
Shahini E collected data of the patient and drafted the manuscript; Maldi E performed the histological analysis of endoscopic biopsies; Staiano T provided content expertise; all the authors reviewed and approved the final draft.
Conflicts of interest
The authors disclose no conflicts.
References
- van Wulfften, Tromp I, Ferreira A, Fiore A, Bramer JAM, et al. (2019) Sacral chordoma: A clinical review of 101 cases with 30-year experience in a single institution. Spine J 19(5): 869-879.
- Catton C, O’Sullivan B, Bell R, Laperriere N, Cummings B, et al. (1996) Chordoma: Long-term follow-up after radical photon irradiation. Radiother Oncol 41(1): 67-72.
- Casali PG, Messina A, Stacchiotti S, Tamborini E, Crippa F, et al. (2004) Imatinib mesylate in chordoma. Cancer 101(9): 2086-2097.
© 2019 Teresa Staiano. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






