- Submissions

Full Text
Medical & Surgical Ophthalmology Research
Homozygous INPP5E Mutation Associated Joubert Syndrome with Retinitis Pigmentosa- A Case Report
Natalie Huang1*and Amirfarbod Yazdanyar2
1Department of Ophthalmology and Visual Sciences, State University of New York Upstate Medical University, USA
2Department of Ophthalmology and Mohawk Valley Retina, East Syracuse, USA
*Corresponding author: Natalie Huang, State University of New York Upstate Medical University, 750 E Adams Street Syracuse, NY 13202, USA
Submission: June 11, 2022;Published: June 30, 2022

ISSN 2578-0360 Volume3 Issue3
Abstract
Purpose:To present a case with INPP5E mutation associated with Joubert syndrome and retinitis
pigmentosa (RP).
Methods: A 11-year-old girl presented with progressive vision loss, lack of coordination, and muscular
weakness. Vision acuity was 20/60 bilaterally. Dilated fundus exam revealed temporal disc pallor,
retinal pigmentary epithelial mottling and atrophy, and diffuse white specks. Fundus autofluorescence
showed diffuse peripheral hypo autofluorescence and a ring of hyper autofluorescence in the macula.
Electroretinography showed decreased cone and rod responses.
Results: Genetic test was positive for INPP5E c.1073C>T (p. Pro358Leu) homozygous mutation.
Conclusions and Importance: INPP5E is one of many genes contribute to Joubert syndrome. A novel
homozygous mutation in INPP5E (c.1073C>T (p. Pro358Leu) can be associated with Joubert syndrome
combined with RP.
Keywords:Joubert syndrome; Retinitis pigmentosa; INPP5E; Ciliopathy
Introduction
Joubert syndrome (JS) is a ciliopathy caused by over 34 heterogenous genes that affect the function of primary cilia 1. It manifests as a neurodevelopmental disorder with related retinal or renal dystrophies and other organs, depending on the genes involved. It is inherited in an autosomal recessive pattern. INPP5E mutations have been recognized as a rare cause of ciliopathy and contribute to JS with associated diseases. [1-3] INPP5E encodes inositol polyphosphate 5-phosphate E, a vital protein in creating and maintaining primary cilia, which can be found in the inner segment of photoreceptors. [4] Retinitis pigmentosa has been rarely reported in patients with JS. We would like to present a case with a novel homozygous mutation in INPP5E in a patient with JS combined with retinitis pigmentosa.
Case Report
A 11-year-old Arabic-speaking girl presented with chronic and progressive vision loss since age 7. She reported more blurred vision at night than during the day. She had trouble seeing in school. Her vision would completely whiten out and then gradually come back when she was exposed to bright light. Besides progressive myopia, she also endorsed a history of “a nerve problem” since birth. The patient had been attending occupational therapy to learn how to improve her muscular strength and coordination. She had suffered from chronic headache, insomnia, and fine motor skill deficiency, such as difficulty writing and frequent dropping of objects. Family history included a brother with nonprogressive nyctalopia and a maternal aunt who was blind in her 30s with unknown diagnosis. On external examination, there was weakness in proximal muscles. She also demonstrated fine nystagmus with intermittent diplopia. Her best-corrected vision acuity (BCVA) was 20/60 bilaterally with a refraction of -6.00 diopters in spherical equivalent in both eyes. Clear cornea and lens, retina showed mild temporal disc pallor, retinal pigmentary epithelial (RPE) mottling and retinal atrophy in the macular, attenuated vasculature, RPE mottling in a speculated pattern in the periphery, and diffuse white flecks (Figure 1). Fundus autofluorescence (FAF) showed severe peripheral hypo autofluorescence with a ring of hyper autofluorescence around the macula, which was consistent with unhealthy RPE (Figure 2). Optic coherence tomography (OCT) revealed outer retinal atrophy with peri macular ellipsoid zone loss in both eyes (Figure3). Electroretinography (ERG) was consistent with decreased cone and rod responses (Figure 4). Humphry visual field test demonstrated bilateral total peripheral visual field restrictions (Figure 5).
Figure 1:Color Fundus photography of the right eye
(A) and left eye.
(B) both demonstrate mild temporal disc pallor, retinal pigmentary epithelial (RPE) mottling and retinal atrophy in
the macular, attenuated vasculature, RPE mottling in a speculated pattern in the periphery and diffuse white flecks
throughout the retina.

Figure 2:Fundus autofluorescence (FAF) of the right eye
(A) and left eye.
(B) show bilateral severe peripheral hypo autofluorescence with a ring of hyper autofluorescence around the macula,
consistent with unhealthy retinal pigmentary epithelium.
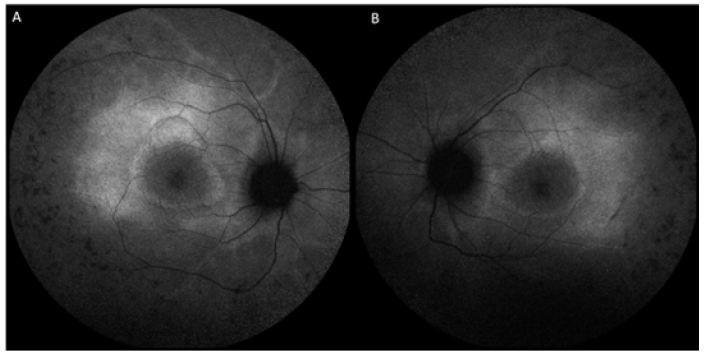
Figure 3:Optic coherence tomography (OCT) of the right eye
(A) and left eye.
(B) reveal outer retinal atrophy with perimacular ellipsoid zone loss in both eyes. White arrows demonstrate the
beginnings of ellipsoid zone loss.
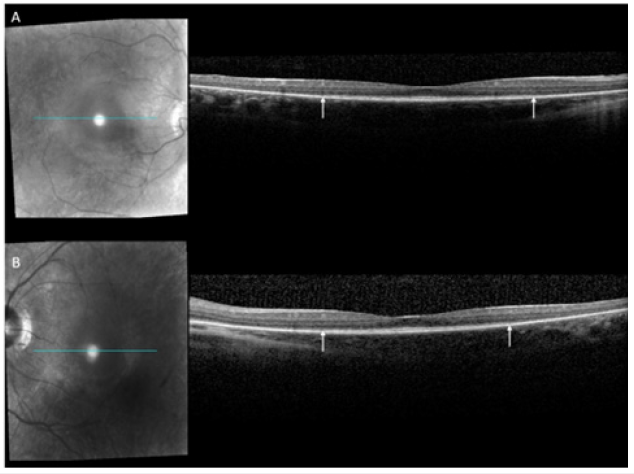
Figure 4:Electroretinography (ERG) was consistent with decreased cone and rod responses.
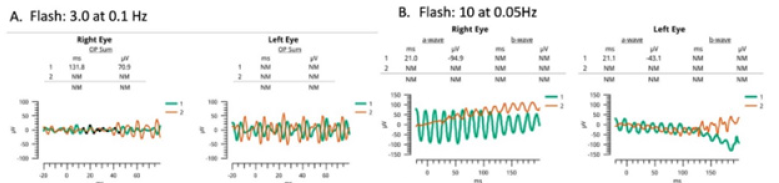
Figure 5:Humphry visual field test demonstrated total peripheral visual field restrictions in the right eye (A) and the left eye (B).

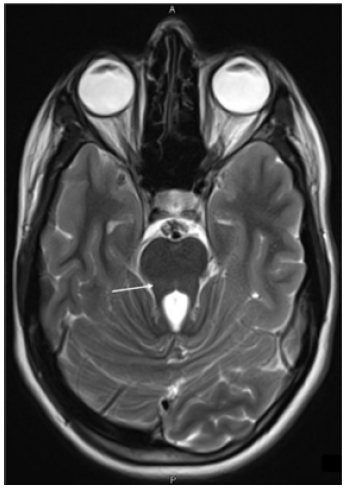
The patient was diagnosed with RP with a genetic test positive for INPP5E c.1073C>T (p. Pro358 Leu) homozygous mutation. Magnetic resonance imaging (MRI) of the brain demonstrated the molar tooth sign with atrophy of the cerebellar vermis, thickened and elongated superior cerebellar peduncles and deep interpeduncular fossa (Figure 6). The patient exhibited progressive myopia with a BCVA of 20/100 bilaterally with progressive pain in her spine, for which she followed up with neurology with repeat neuroimaging.
Figure 6:Magnetic resonance imaging (MRI) of the brain demonstrated the molar tooth sign (white arrow), with atrophy of the cerebellar vermis, thickened and elongated superior cerebellar peduncles and deep interpeduncular fossa.
Discussion
JS is a rare autosomal recessive disorder that belongs to a subgroup of ciliopathies that affect the central nervous system. Patients with JS demonstrate developmental delay, ataxia, hypotonia, nystagmus, renal and retinal dystrophies. [2,5] The diagnosis of JS is confirmed by the molar tooth sign on MRI of the brain, which is characterized by hypo genesis or agenesis of the cerebellar vermis, hypertrophy and elongation of the superior cerebellar peduncles and deep interpeduncular fossa. [6,7] Phosphoinositide 5-phosphatase is a ciliary protein encoded by INPP5E, mutations that cause ciliopathies, including JS. [8] Different mutations of the same gene can lead to different manifestations. For instance, a homozygous mutation at INPP5E c.1303C>T (p. Arg435Trp) was found to cause JS and related nephropathy, while a homozygous mutation at INPP5E c.1565G>C was linked with JS and retinal dystrophy. [2] In a large cohort study of patients with JS, INPP5E was found to be most visually impaired due to retinal degeneration. [1,3] There are 27 known INPP5E mutations that are associated with 2.7% of JS and related syndromes that involve predominantly the ocular system, such as Bardet- Biedel syndrome and Cohen syndrome [4,9]. In Arabs, such as our patient, INPP5E is one of the most common genetic mutations that are associated with JS [10].
Conclusion
Although retinal dystrophies have been known to be associated with JS, a case with JS combined RP has not been reported in the literature. We present the first case of such, with a novel homozygous mutation at INPP5E c.1073C>T (p. Pro358 Leu). As INPP5E has been increasingly recognized as a causative gene for JS and related syndromes, we hope to acknowledge this distinct mutation and its association with JS and RP, which could help direct clinicians with their diagnosis with a similar presentation.
References
- Brooks BP, Zein WM, Thompson AH, Mokhtarzadeh M, Doherty DA, et al. (2018) Joubert Syndrome: Ophthalmological findings in correlation with genotype and hepatorenal disease in 99 patients prospectively evaluated at a single center. Ophthalmology 125(12): 1937-1952.
- Shetty M, Ramdas N, Sahni S, Mullapudi N, Hegde S (2017) A Homozygous missense variant in INPP5E associated with joubert syndrome and related disorders. Mol Syndromol 8(6): 313-317.
- Rao KN, Zhang W, Li L, Anand M, Khanna H (2016) Prenylated retinal ciliopathy protein RPGR interacts with PDE6δ and regulates ciliary localization of Joubert syndrome-associated protein INPP5E. Human Molecular Genetics 25(20): 4533-4545.
- Hardee I, Soldatos A, Davids M, Vilboux T, Toro C, et al. (2017) Defective ciliogenesis in INPP5E-related joubert syndrome. Am j med genet A 173(12): 3231-3237.
- Choh SA, Choh NA, Bhat SA, Jehangir M (2009) MRI findings in Joubert syndrome. Indian journal of pediatrics 76: 231-235.
- Maria BL, Quisling RG, Rosainz LC, Yachnis AT, Gitten J, et al. (1999) Molar tooth sign in Joubert syndrome: clinical, radiologic, and pathologic significance. J child neurol 14(6): 368-376.
- Doherty D (2009) Joubert syndrome: insights into brain development, cilium biology, and complex disease. Semin Pediatr neurol 16(3): 143-154.
- Nozaki S, Katoh Y, Terada M, Michisaka S, Funabashi Y, et al. (2017) Regulation of ciliary retrograde protein trafficking by the Joubert syndrome proteins ARL13B and INPP5E. J Cell Sci 130(3): 563-576.
- Travaglini L, Brancati F, Silhavy J, Iannicelli M, Nickerson E, et al. (2013) Phenotypic spectrum and prevalence of INPP5E mutations in Joubert Syndrome and related disorders. Eur J of Hum Genet 21(10): 1074-1078.
- Devi ARR, Naushad SM, Lingappa L (2020) Clinical and molecular diagnosis of joubert syndrome and related disorders. Pediatr Neurol 106: 43-49.
© 2022 Natalie Huang. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






