- Submissions

Full Text
Medical & Surgical Ophthalmology Research
A New Technique in Surgical Reconstruction of Upper Lid
Duong Dieu*
Faculty of Medicine-Nguyen Tat Thanh University. Add 300A Nguyen Tat Thanh street-Dist 4-HoChiMinh City, Vietnam
*Corresponding author: Duong Dieu, Faculty of Medicine-Nguyen Tat Thanh University. Add 300A Nguyen Tat Thanh street-Dist 4-HoChiMinh City, Vietnam
Submission: February 26, 2022;Published: April 18, 2022

ISSN 2578-0360 Volume3 Issue3
Abstract
Surgical reconstruction of the upper lid due to lagophthalmia is necessary. Lagopththalmia can be caused by trauma, inflammation, or congenital. Lagophthalmia with unclosed eyelid can be affected patient’s vison. Herpes Zoster ophthalmicus is an ocular disease that usually manifests as a unilateral painful skin rash in a dermatomal distribution of the trigeminal nerve shared by the eye and ocular adnexa. All of age can be occured by HZO but it is typically in older adults. In case of latent varicella-zoster virus (VZV) is reactive HZO can occurs within the sensory spinal or cerebral ganglia. Bell’s palsy (facial palsy) is characterized by facial drooping on the affected half, due to malfunction of the facial nerve. With lagophthalmia 2 problems are faced: esthetics and functional views. Reconstruction of the upper lid is satisfied both esthetic and functional views. A technique for reconstruction of the upper lid on these patients was proposed and described in detail as below. Three cases were selected in this case study. The first is loss of the upper lid by trauma. The last 2 cases are lagophthalmos with Bell’s paralysis and lagophthalmos caused by the contracted scar of the upper lid. All of these cases had been used as a simple new surgical technique with some advantages are discussed. The results and some consideration on HZO are reported herein.
Keywords:Surgical reconstruction; New technique; Upper lid; Lower lid; Lagopththalmia; Trauma
Introduction
Surgical reconstruction of the upper lid caused by lagophthalmia is necessary. Lagopththalmia can be caused by trauma, inflammation, or congenital [1,2]. Lagophthalmia with unclosed eyelid can be affected patient’s vison with unavailable treatment. Herpes Zoster Ophthalmicus is an ocular disease that usually manifests as a unilateral painful skin rash in a dermatomal distribution of the trigeminal nerve shared by the eye and ocular adnexa. All of age can be occured by HZO but it is typically in older adults. In case of latent varicella-zoster virus (VZV) is reactive HZO can occurs within the sensory spinal or cerebral ganglia. Bell’s palsy (facial palsy) is characterized by facial drooping on the affected half, due to malfunction of the facial nerve. In Lyme disease has also been related although the causes were not recognized in most cases with Herpes simplex. Ocular involvement occurs in approximately 50% of HZ patients without the use of antiviral therapy [3,4]. HZO is not a fatal cause. It caused the prolonged pain lead to disturbance and difficulty in treatment. It is one of many causes of bindness. So it may be a marker for AIDS particularly in young person [5,6]. With lagophthalmia 2 problems are faced: esthetics and functional views. Reconstruction of the upper lid is satisfied both esthetic and functional views. At echnique for reconstruction of the upper lid on these patients was proposed and described in detail as below. Three cases were selected in this case study. The first is loss of the upper lid by trauma. The last 2 cases are lagophthalmos with Bell’s paralysis and lagophthalmos caused by the contracted scar of the upper lid.
All of these cases had been used as a simple new surgical technique with some advantages are discussed. The results and some consideration on HZO are reported herein [7-10] included prevention [11,12].
Methods
Surgical technique with flap from frontal skin
Local anesthesia by injection 10 ml of lidocaine 2% into frontal
skin at nasal, frontal, and temporal V1 nerve:
A. From the upper lid we do a parallel incision 2mm from
this margin.
B. The 2 edges of this incision were dissected to create
a flap that could be grafted from the lower eyelid to correct the
lagophthalmos.
C. The pedicle was at the lateral level of the eyebrow. Inorder
to relpace the missing of upper lid this skin flap is used. The few
lines of eyebrows replaced the lost eyelashes. We used simple
sutures for the forehead wound. A crescent-shaped skin flap of
70x20mm was created from frontal skin. From the root of pedicle
we spread the flap to the medial canthus. This pedicle was too big
to nourish the flap replacing the upper lid. The donor area of the
frontal skin was then closed with simple sutures (case 1).
D. In case of frontal skin is not suitable for donor: (case 2) A
crescent-shaped skin flap of 70 x20mm was created from the lower
eyelid (a parallel marginal 2mm incision was made at the lower
eyelid an incision is done for making the flap). This flap is spreaded
from the pedicle to the medial canthus performing new lower lid.
The flap is nourished with an enough big pedicle.
E. The donor area of the lower eyelid was then closed with
simple sutures to avoid ectropion of the lower eyelid.
F. The flap with crescent-shape of the lower lid is moved to
upper lid with clockwise. At first one suture is done with the head
of flap, then the upper and lower lid are sultures. The pedicle of the
flap was the lateral canthus and was directly sutured.
G. Post sugery: The pedicle will be cut off at one week after
graft.
Surgical technique with flap skin from lower eyelid
A. Local anesthesia by injection of 10 ml of lidocaine 2% into
the upper lid and lower lid.
B. A parallel incision was made for flap above the lower lid
with 2mm from this margin:
C. The head of the flap was at the medial canthus and the
pedicle at the lateral canthus. This pedicle was too big to nourish
the flap.
D. The donor area of the lower eyelid was then closed with
simple sutures to avoid ectropion of the lower eyelid.
E. The flap with crescent-shape of the lower lid is moved to
upper lid with clockwise. At first one suture is done with the head
of flap, then the upper and lower lid are sultures. The pedicle of the
flap was the lateral canthus and was directly sutured.
F. One week following the graft, the pedicle was severed and
the sutures will be cut off.
G. Using lower lid skin in these cases are available both
aesthetic and reconstructive view.
Case Reports
Case 1
A 32-year-old male farmer fell while digging. After that he had suddenly bleeding from his left eye and pain brutally, so he cried for help. The neighbor took him to the health station of the village. At primary health care station in village: the patient with a first-aid dressing eye was transfered to the provincial hospital (Figure 1).
Figure 1:Graft upper lid trauma with frontal skin+some eyebrow flap.

Ocular examination revealed a visual acuity of 20/20 in the right eye.(OD: oculus dexter) and 20/20 in the left eye (OS: oculus sinister). Intraocular pressure was 12mmHg in both eyes (OU). Right eye=normal. Left eye=The upper eyelid was almost completely severed together with all the eyelashes, three-quarters of the skin, two-thirds of the tarsus, and half of the conjunctiva of the upper lid from the lid margin. Both eyeballs were normal. BP=120/70mmHg. BG=80mg% BT=2’ BC=5’. General examination: Nothing abnormal detected. Patient’s history: well-being. Diagnosis: Loss of an upper eyelid can arise through trauma Surgical Treatment: mentioned 2.1 above. This forehead wound beneath the flap was closed with interrupted sutures (Figure 2).
Figure 2:Graft upperlid Bell’s palsy with lowerlid skin flap.
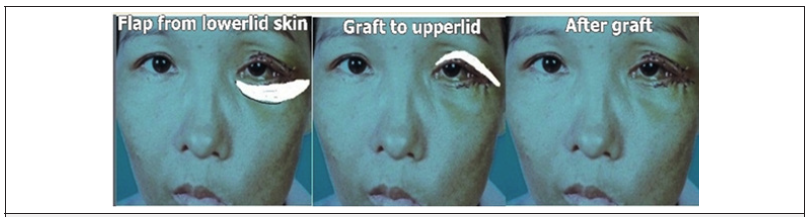
Using the head flap was sutured to the medial canthus, the upper edge of the flap to the residual upper lid by running sutures. The lower edge of the flap with the few lines of the eyebrow was turned down to become the new eyelid margin, using running sutures side-by-side (Figure 3).
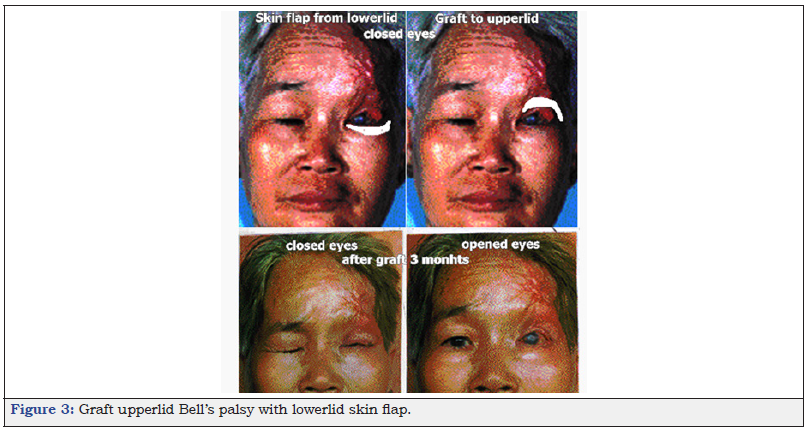
Figure 3:Graft upperlid Bell’s palsy with lowerlid skin flap.
Post-operative Recovery: By the second or third week postoperatively, the bruising had diminished and the color of the head skin flap had regained normally. Visual acuity for this patient 6 months later remained at 20/20.
A. A 45-yo-female suffered from facial drooping on the
affected half, eye-watering tears for many months, and no receiving
any drugs for treatment.
B. Eye examination revealed: RE=VA6/6. Normal. LE=VA
6/12. Cornea exposed 2mm when closed eye. Fluoresceine (+).
Laboratory findings included: RBC=3,900,000/mm3. WBC=7,600/
mm3. HIV=Negative. PCR Herpes (+). Normal chest X-ray and ECG.
C. Diagnosis: Recurrent Bell’s palsy 1st time and scattered
point keratitis. Lagophthalmos post-Bells palsy with PCA Herpes
(+).
D. Treatment: Steroid: prednisolone dose for 3 weeks.One month later: repeated treatment but lagophthalmos was not
ameliorated and poor vision 6/12.
E. Surgical Treatment for correction lagophthalmos:
mentioned 2.1 above.
Case 3
A 56-year-old female patient with 7 previous months of Herpes zoster ophthalmicus (HZO) was admitted the hospital. At the provincial hospital the patient was treated with intermittent pain relief after 6 months. The patient was severe left frontal headaches and eye ache for 2 week previously and oral steroids were prescribed by another (private) doctor. She was admitted to the author’s hospital. Eye check- up showed visual acuity 20/20 OD, light perception OS, The upper lid of the left eye had an adherent scar and contracted scar that caused the upper eyelid to shorten and thus exposed all of the cornea and part of the ocular conjunctiva. The conjunctiva of the upper lid was totally exposed with a round ulcer 1.5mm diameter. There was also a corneal ulcer of 10 mm diameter, with an irregular surface, that gave a positive to fluorescein. The anterior chamber was not observed. Laboratory findings included: RBC=3,900,000/mm3. WBC=7,600/mm3. HIV=Negative. Normal chest X-ray and ECG.
Diagnosis: Lagophthalmos caused by Herpes Zoster ophthalmicus Treatment: Surgical Treatment: mentioned 2.1 above.
Discussion
Case 1: Loss of an upper eyelid results in aesthetic and functional problems
For repairing upper eyelid defects there are many invasive techniques. The Cutler-Beard bridge flap from the lower eyelid is one of these techniques, the inverted semicircular flap, multiple composite eyelid grafts, the lower eyelid switch flap, the inferiorly based tarsoconjunctival flap, The tarsography is also used. These procedures result can be advantages as well as disadvantages. Many of these procedures are 2-staged [1, 2].
In this case of full-thickness loss of the total upper eyelid, Mustarde’s method, Mustarde’s method of repair (pedicle flap from lower lid to upper lid) was not appropriate. So a one stage procedure with foredead flap was done. When a cutting upper eyelid trauma, the levator muscle was contracted. In order to repair ptosis secondary trauma is about 6 to 9 months later as the condition may be self-limiting [1,2,5].
A full-thickness defect of the upper lid in this case. At first to cover the eyeball quickly a forehead skin flap to the upper lid is created. The superficial temporal artery will nourished this flap. The flap is nourished with an enough big pedicle. With the author’s experience, this case the width of the pedicle is one-third the length of the flap. The eyeball is covered by flap is one of many advantages of our one-stage procedure. So the preventing the possible sequelae of exposure such as ulceration of the conjunctiva or cornea, endophthalmitis, and rarely, enucleation [2]. In addition, in a tropical climate, ultraviolet light can cause lens and retinal damage. Ultimately, blindness may result. But the disadvantage of our procedure is the levator muscle without restoring [2].
Case 2 and 3: Lagophthalmia with Surgical Treatment
In case 2: Bell’s palsy (facial paralysis) is characterized by facial drooping on the affected half, due to malfunction of the facial nerve (VII cranial nerve), which controls the muscles of the face. The Charles Bell, who first described Bell’s palsy is a Scottish anatomist, Bell’s palsy is the most common acute mononeuropathy (disease involving only one nerve) and is the most common cause of acute facial nerve paralysis. The paralysis is of the intranuclear/ lower motor neuron type. Most people with Bell’s palsy will recover fully in time, even without treatment, but current treatments reflect the belief that viral inflammation of the seventh cranial nerve causes the compression and resulting paralysis. Cortico-therapy is used in the inflammation and swelling of the nerve along with an antiviral medication such as acyclovir or valacyclovir if a viral infection was suspected. According to the Mayo Clinic, evidence from clinical trials shows that treatment with steroids tends to be more successful than treatment with antivirals. After the failure treatment of steroids associated with antiviral drugs in case 3, an auto skin graft for correction lagophthalmos was done with good results as well as a good vision after a one-year follow-up [5,8].
In case 3:
Lagophthalmos due to adherent scar and contracted scar of the upper eyelid caused by herpes zoster is rarely seen but this condition needs to treat early for protective vision. Lagophthalmos caused by herpes zoster is rarely seen. HZO caused around all cases of 40% keratitis, 40% of uveitis cases, as well as necrosis retinitis, secondary glaucoma, ocular motor nerve palsies, cataract, and scleritis [5,9]. We will discuss our simple surgical technique for correcting this lagophthalmos The simple surgical technique can be performed under local anesthesia without the need for expensive technical equipment. A split level eyelid graft was used to repair a full-thickness defect caused by Herpes zoster lagophthalmos. In this patient, we used a pedicle flap from the lower to the upper lid (Mustarde’s method) associated with a split-level eyelid on the outer surface. There are several advantages to this technique. This patient was enough lower lid skin is an advantage. This laxity of lower lid skin was sufficient for reconstruction of the upper lid lagophthalmos. The second advantage the tarsal-conjunctiva was enough for this graft. The third advantage, the levator muscle remained in good condition both pre and after surgery. In upper lid reconstruction, the levator muscle is the most required structure. According to Mustarde’s method, this pedicle is about 8mm wide but we created a 20mm pedicle in order to permit a one-stage procedure [1,5]. The skin flap was nourished by two sides: one from the direct suture and the other from the pedicle. The root of the pedicle (2cm) was severed enough for successful grafting.Others problems with ophthalmic zona
*Herpes Zoster Ophthalmicus (HZO) and HIV: Kenya, Herpes Zoster Ophthalmicus (HZO) has been reported in 23% of patients with AIDS, aged between 8 to 47 years. Ocular motor nerve palsies and corneal involvement were seen in 3% and 2% of cases, respectively. HIV has been isolated from the healthy cornea of patients with AIDS. Our case 3 belonged to this age group. Ophthalmic zona may be a marker for AID Diagnosis of typical zona is usually easy with the eruption of vesicles distributed along trigeminal nerve but in the atypical case is not easy and for a gold standard in diagnosis DNA of zona virus is polymerase chain reaction (PCR). The general practitioners, eye doctors should be cautious in atypical cases of the zona, as well as particularly in the phrase of pre-eruption of vesicles because of transmission of both zona and HIV. In case 3 of the author unit, HIV was (+) and trabeculectomy was done and 10 months later this patient was died because of the final stage of AIDS [3,4,5].
*HZO and post herpetic neuralgia: HZO is not fatal but postherpetic neuralgia causes misery and distress. Treatment should start early at the time of HZO infection with antiviral agents, oral analgesics, and steroids.
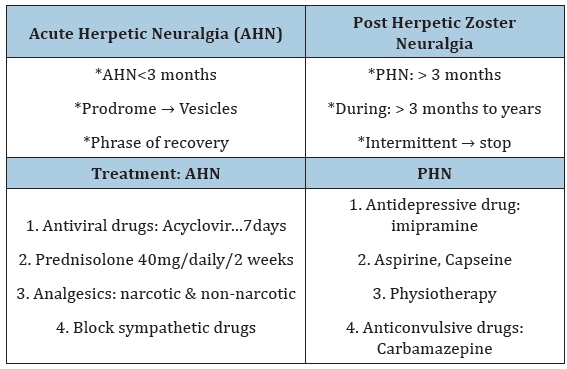
In these cases, the patients took both analgesics and steroids although steroids were more effective. The antiviral drug is prohibitively expensive and was not taken in case 1 but it had been used in case 2 and case 3. In the case of lagophthalmos, this resulted in severe corneal ulceration. In corneal scarring treated by perforated cornel grafting, recurrence took place in 20% of cases [6,7]; Table 1.
Table 1:Classification and treatment of herpetic neuralgia
*Cornea: The decreasing of corneal sensibility postherpetic
zoster may reversible or irreversible because of corneal epithelial
damages. Surgeries in these patients as glaucoma, cataract has to
be a warning [5].
*Iris: The paralysis of the constricted sphincter of the iris may
lead to dilation of the pupil so-called atypical Argyl Robertson
syndrome [5].
In this case: the pupil did not constrict one year later.
*Strabismus: may be caused by the paralysis of ocular muscles
need to be surgical correction [10].
Prevention< Adults 60- year-old and over should have a single dose of zoster vaccine whether they have had herpes zoster or not. This vaccine has been shown to decrease the incidence of zoster [11]. Receiving 400mg of acyclovir orally twice daily for one year would prevent ocular recurrences in immunocompetent persons who had had an episode of ocular HSV within the preceding year [12].
Introduction
Auto skin graft- a single-stage procedure for correction of upper eyelid lagophthalmos will then improve visual acuity as well as appearance. These patients have restored vision and have normalized intraocular pressure, and some satisfying results were reported hereafter a one-year follow-up. In our experience, tarsography should be performed first as a temporary treatment for lagophthalmos if vision is decreased. The result of surgical treatment on zona glaucoma with HIV (+) is poor both in vision as well as the quality of life. Some considerations on HZO were discussed in this paper for General Practitioners and Eye Doctor
Funding
No funding or grant support was received for this work.
Funding
No financial disclosures.
References
- McCord D, Lisman RD (1987) Upper eyelid reconstruction. In: Smith BC (Ed.), Ophthalmic plastic and reconstructive surgery. The CV Mosby Company, Missouri, USA, pp: 822-840.
- Duong Dieu (2017) Replaced loss of upper eyelid by frontal skin graft. International Journal Surgery Research. SciDoc Publishers, USA, 4(4): 85-87.
- Liesegang TJ, Thomas J (2008) Herpes zoster ophthalmicus natural history, risk factors, clinical presentation, and morbidity. Ophthalmology 115(2 Suppl): S3-S12.
- Haroon Awan R, Henry Alada S (1996) Ophthalmic manifestation of AIDS in Kenya. Ophthalmic Practice, Asian Edition, 2(3): 92-101.
- Miller SS (1987) Medical treatment for zona pigment glaucoma. Clinical Ophthalmology, Bristol, UK, 139: 172-194.
- Acland RH (1996) Herpes zoster and postherpetic neuralgia. Medical Progress 23(1): 38.
- Duong Dieu (2017) Herpes zoster ophthalmicus and medical treatment. Worldwide Journal of Multidisciplinary Research and Development 3(6): 01-04.
- Duong Dieu (2018) Surgical treatment for bell’s paralysis. International Journal of Research Publications 6(1): 5-7.
- Duong Dieu (2001) Upper eyelid reconstruction. Medical Progress 28(6): 26-
- Duong Dieu (1998) Surgical correction of exotropic and esotropic strabismus, ophthalmic practice. Canada, 16(2): 84-86.
- https://www.merckmanuals.com/professional/infectious-diseases/herpesviruses/herpes-zoster
- Wilhelmus KR, Beck RW, Moke PS, Dawson CR, Barron BA (1998) Acyclovir for the Prevention of Recurrent Herpes Simplex Virus Eye Disease. N Engl J Med 339: 300-306.
© 2022 Duong Dieu. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






