- Submissions

Full Text
Medical & Surgical Ophthalmology Research
Acute Angle-Closure Glaucoma Resulting from Ciliochoroidal Effusion in a Young Myope Under Aripiprazole Therapy: A Case Report
Anne-Sophie Simons1,2*, Sophie Lemmens1,2 and Ingeborg Stalmans1,2
1Department of Ophthalmology, University Hospitals UZ Leuven, Belgium
2Department of Neurosciences, Laboratory of Ophthalmology, Belgium
*Corresponding author: Anne-Sophie Simons, Department of Ophthalmology, University Hospitals UZ Leuven, Belgium
Submission: February 09,2022;Published: February 21,2022

ISSN 2578-0360 Volume3 Issue3
Abstract
A 15-year-old girl presented with unilateral acute angle-closure glaucoma and bilateral myopisation. The patient had a medical history of depression under new therapy with aripiprazole. Ocular ultrasound demonstrated bilateral ciliochoroidal effusion with anterior rotation of the ciliary body and a forward displacement of the lens-iris diaphragm. After topical and systemic antihypertensive treatment and cessation of aripiprazole, intraocular pressure (IOP) normalised.
Introduction
Although glaucoma is highly prevalent worldwide, the prevalence of medication-induced glaucoma is uncertain. Drug-induced angle-closure glaucoma is an important entity for the ophthalmologist as well as the general physician as it represents a preventable cause of potential blindness [1]. Aripiprazole is an atypical antipsychotic drug, a quinolone derivate, that is used in the treatment of depression, bipolar disorder, obsessive-compulsive disorder and schizophrenia [2]. It is a partial agonist that acts on mesolimbic and mesocortical dopamine pathways. Insomnia, anxiety, headache, nausea, vomiting, weight gain and somnolence are common adverse effects. Sulfonamide derivatives have been reported to be associated with an idiosyncratic inflammation in the uveal tissue that result in choroidal effusion and ciliary body edema [3]. Ocular side effects of aripiprazole, which is not a sulfonamide derivate, are very rare. Thorough review of literature revealed only one case of aripiprazole-induced acute angle-closure glaucoma in a patient with plateau iris configuration. We describe a case of bilateral ciliochoroidal effusion with unilateral acute angle closure under aripiprazole therapy in a young patient with high myopia.
Case Report
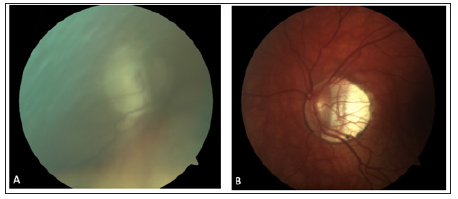
In June 2021, a 15-year-old girl was referred to our center because of acute angleclosure glaucoma in her right eye, which was not controlled after laser iridotomy and topical intraocular pressure-lowering medications. Her past ocular history included retinopathy of prematurity and high myopia. A review of her past medical history revealed a diagnosis of major depression. She was being treated with fluoxetine and trazodone for over one year, and more recently, aripiprazole. Family history was not significant for ocular diseases. One month after the start of aripiprazole, the IOP in her right eye was 24mmHg, for which she was prescribed timolol. The pressure in her left eye was 14mmHg at that time. Despite the continuation of treatment, the patient presented 3 months later with a painful red eye and blurry vision. On examination, her best-corrected visual acuity was 20/25 with -21.50 diopters in the right eye was 20/33 with -15.25 diopters in the left eye. Biomicroscopy revealed a pre-existing corneal band keratopathy, a bilateral shallowing of the central and peripheral anterior chamber with semi mydriasis and conjunctival hyperaemia in the right eye. Her IOP was 40mmHg in the right eye and 11mmHg in the left eye. Fundoscopy showed peripheral laser marks (related to her retinopathy of prematurity treatment) and a myopic retina. The optic discs were tilted and showed peripapillary atrophy, hindering neuroretina rim interpretation (Figure 1A&1B). Fundoscopy of the right eye was blurry due to the band keratopathy (Figure 1A).
Figure 1:Fundus photo of the right eye (A) and left eye (B).
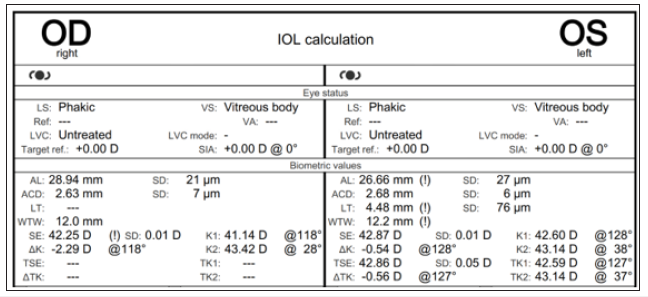
An urgent laser iridotomy was performed by her ophthalmologist, and she was started on topical antihypertensive therapy with travoprost, brinzolamide-timolol, and systemic acetazolamide which lowered IOP to 11mmHg in the right eye. The pressure in the left eye was 12mmHg at that moment. The pressure remained well-controlled under this therapy until 4 days after discontinuation of the acetazolamide when the unilateral acute angle closure-glaucoma reoccurred with an IOP rise to 32 mmHg despite patent iridotomy. Pilocarpine was then added, and acetazolamide reintroduced. Gonioscopy showed a closed angle in her right eye and a narrow angle in her left eye, respectively, Shaffer grade 0 and 1. Biometry showed an axial length of 28.94mm in the right eye and 26.66mm in the left eye. The anterior chamber depth was 2.63mm in the right eye and 2.68mm in the left eye (Figure 2).
Figure 2:Biometry.
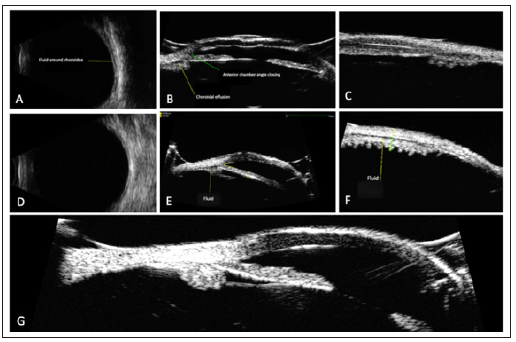
Since such a narrow anterior chamber depth is unusual for long eyes, we also performed an ocular ultrasound of the right eye. The ultrasound showed choroidal effusion syndrome with fluid accumulation around the choroid and an anterior rotation of the ciliary body, resulting in a forward displacement of the iris-lens diaphragm and a closed anterior chamber angle (Figure 3A-3C).
We advised immediate cessation of the antipsychotic drug aripiprazole. The topical antihypertensive therapy with travoprost and brinzolamide-timolol, as well as the oral therapy with acetazolamide, was continued. Pilocarpine was discontinued and a cycloplegic agent was started. After the withdrawal of aripiprazole, the eye pressure returned to normal even after discontinuation of acetazolamide. Repeated ocular ultrasound showed gradual resorption of the suprachoroidal fluid after withdrawal of aripiprazole (Figure 3D-3F), with a complete resolution 4 months after cessation (Figure 3G). The best-corrected visual acuity in the right eye improved from 20/25 to 20/63. After two months of well controlled eye pressures, the topical antihypertensive therapy was also discontinued. The patient’s eye pressure remained low during the four months of follow-up at our center, after which she was referred back to her ophthalmologist for further follow-up.
Figure 3:Echography of ciliochoroidal effusion syndrome in the right eye. B-scan demonstrated 360°shallow choroidal effusions in the posterior segment. (A) Ultrasound biomicroscopy (UBM) showed ciliary body edema and angle closing. (B and C) B-scan and UBM showed a decrease but persistent fluid accumulation suprachoroidal one month after discontinuation of Aripiprazole (3D, 3E and 3F) and total resolution of the ciliary effusion four months after discontinuation of aripiprazole (3G).
Discussion
This case is the second report of drug-induced angle-closure glaucoma due to choroidal effusion associated with aripiprazole use and the first report of this mechanism in a patient without the additional risk factor of a pre-existing narrow-angle in the context of a plateau iris configuration as described by Shen et al. [4] who reported the first case in 2018 [4]. Ocular ultrasound was instrumental in confirming the hypothesized mechanism of angle-closure, which is caused by an idiosyncratic inflammation in the uveal tissue that results in choroidal effusion and ciliary body edema. Consequent swelling and anterior rotation of the ciliary body causes an anterior shift of the iris-lens diaphragm and anterior chamber angle closure. This mechanism has been more extensively described using sulfa-based derivatives such as topiramate, hydrochlorothiazide, acetazolamide and other medications. It is an exceptional mechanism of acute angle-closure glaucoma, requiring a different management strategy than angle-closure glaucoma due to pupillary block. The use of pilocarpine is therefore not indicated for this type of acute angle-closure, as this further enhances the mechanism of anterior rotation of the ciliary body and iris diaphragm. On the contrary, the use of cycloplegic agents can be considered in such cases to counteract the anterior rotation of the ciliary body. Although acetazolamide itself has exceptionally been associated with acute angle-closure by ciliary effusion syndrome, its use was helpful in the resorption of choroidal effusion provoked by aripiprazole in our case. Both in the case presented by Shen et al. [4] and in our case, the eye pressure was not controlled by mere initiation of topical antihypertensive medication. Cessation of the causative agent appears indispensable for adequate pressure control, which emphasizes that this should be the first management step.
Conclusion
A. If a patient is placed on aripiprazole or other drugs,
reports back to the physician with symptoms suggestive of
acute angle-closure glaucoma’s, such as acute painful red-eye
or blurred vision, an immediate ophthalmological referral is
warranted.
B. It is essential to perform a comprehensive systemic drug
history, even when glaucomatous signs present unilaterally.
C. Ocular ultrasound (ultrasound biomicroscope and B-scan)
is key in diagnostics by establishing the underlying mechanism.
D. Treatment for medication-induced acute angle-closure
differs from that of primary angle closure.
E. Discontinuation of the causative agent, use of cycloplegic
drops, and intraocular pressure-lowering medications are key
in treating this condition.
Patient Consent
An informed consent was obtained from the patient.
References
- Khurana AK, Khurana B, Khurana AK (2012 ) Drug-induced angle-closure glaucoma. J Curr Glaucoma Pract 6(1): 6-8.
- Shapiro D, Renock S, Arrington E, Chiodo L, Liu L, et al. (2003) Aripiprazole, a novel atypical antipsychotic drug with a unique and robust pharmacology. Neuropsychopharmacology 28(8): 1400-14
- Alzendi NA, Badawi AH, Alhazzaa B, Alshahrani A, Owaidhah O (2021) O Topiramate-induced angle closure glaucoma: Two unique case reports. Saudi Journal of Ophthalmology 34(3): 202-204.
- Shen E, Farukhi S, Mason S, Mosead S (2018) Acute angle-closure glaucoma associated with aripiprazole in the setting of plateau iris configuration. Journal of Glaucoma 27(2): 40-43.
© 2022 Anne-Sophie Simons. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






