- Submissions

Full Text
Medical & Surgical Ophthalmology Research
Treatment Outcomes of Ocular Surface Squamous Neoplasia with Surgery and Adjunctive Mitomycine C: Retrospective Case Series
Hülya Gökmen Soysal*
Professor of Ophthalmology, Kafkas University Medical Faculty, Turkey
*Corresponding author: Hülya Gökmen Soysal, Professor of Ophthalmology, Kafkas University Medical Faculty, Turkey
Submission: March 8, 2021;Published: March 26, 2021

ISSN 2578-0360 Volume3 Issue2
Abstract
Aim: To present the clinical features and therapeutic outcomes of Ocular Surface Squamous Neoplasia (OSSN) cases which were treated with surgery and adjunctive Mitomycine C (MMC).
Materials and Methods: The records of 38 eyes which were treated for OSSN were reviewed retrospectively. Patients in stages T1 and T2 were treated with ‘no touch’ technique complete excision, cryotherapy and adjunctive MMC. Two patients in stages T3 and T4 disease underwent exenteration.
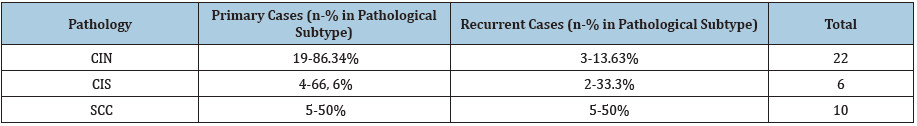
Results: The pathological diagnoses were Conjunctival Intraepithelial Neoplasia (CIN) in 22, carcinoma in situ in 6, and invasive Squamous Cell Carcinoma (SCC) in 10 eyes. Tumor was primary in 28 and recurrent in 10 eyes. The rates of previously recurrent cases were highest in invasive SCC group and lowest in CIN group. No serious complications associated with MMC occurred. A recurrence was observed in only one eye out of 36 eyes in stages T1 or T2. One patient in stage T4 that was treated with subtotal exenteration presented with preauricular lymphadenopathy after 19 months.
Conclusion: Recurrences and treatment complications can still be seen today despite the new developments and facilities regarding the treatment of the OSSN. These recurrences and side effects impair the success rate by increasing morbidity. We recommend a complete excision followed by cryotherapy and routine postoperative adjuvant MMC application to decrease the risk of unsuccessful results.
Keywords: Conjunctiva; Squamous neoplasia; Ocular surface; Mitomycine C
Abbreviations: CIN: Conjunctival Intraepithelial Neoplasia; Ocular Surface Squamous Neoplasia; SCC: Squamous Cell Carcinoma; MMC: Mitomycine-C
Introduction
The term Ocular Surface Squamous Neoplasia (OSSN) includes neoplastic squamous
epithelial abnormalities ranging from mild dysplasia to invasive carcinoma of conjunctiva
and cornea. Its incidence is estimated to be 17 to 20 cases per million people per year [1].
Proposed risk factors are human papilloma virus, exposure to ultraviolet light, cigarette
smoking, human immunodeficiency virus, petroleum products, age, and male sex [1,2].
Symptoms may include foreign body sensation, redness and irritation. The most common
localization is the interpalpebral area of perilimbal conjunctiva. Its clinical appearance may
be described as gelatinous, papilliform, leucoplakic, and diffuse [3]. Occasionally some lesions
may contain a dark pigmentary area occasionally. The lesions are often well demarcated from
the normal tissue and frequently accompanied by a feeder vessel. Diffuse type is the least
common, and may masquerade as chronic conjunctivitis [4].
Simple surgical excision as a traditional treatment method has a reported recurrence rate
as high as 33% despite clear margins and incomplete resection results in recurrence rates
up to 56% [3]. In 1994 Shields et al. described a method involving wide surgical excision
that avoids contact with the tumor (no-touch technique), accompanied by double freezethaw
cryotherapy to the edge of conjunctiva and alcohol application to the corneal edge [4].
Further studies confirmed that this technique is more effective in preventing recurrences [5-
7]. Because of the relatively high recurrence rate of OSSN after surgery, topical chemotherapy
agents have been studied as adjuvant therapy or monotherapy as an alternative to surgery.
Three main agents shown to be effective are Mitomycine-C (MMC) [8-10], 5-Fluorouracil (5-FU) [11,12] and interferon-α2b (INF-α2b) [13,14]. Other treatment
modalities include subconjunctival ranibizumab [15] and external
beam radiation therapy [16,17]. Unsuccessful treatment and
invasive disease may require enucleation or orbital exenteration
[18,19]. The purpose of this study is to report clinical features,
recurrence rates, outcomes and complications in the management
of OSSN by surgery and adjuvant MMC.
Materials and Methods
We retrospectively reviewed the records of cases that were operated as conjunctival tumor and diagnosed as OSSN by histopathological examination between 2007 and 2017. This study was approved by the Ethical Board of the Institutional Ethics Committee of Kafkas University, Kars/Turkey (80576354-050- 99/105) and followed the tenets of the Declaration of Helsinki. Written informed consent was obtained from all patients. Of the 44 patients, 6 with xeroderma pigmentosum were excluded and 38 eyes of 37 patients were included in the study. All surgeries were performed by the same surgeon. Patients with a follow up time less than 6 months and patients treated with adjunctive chemotherapy other than MMC were not included in the study. Two patients were in stage T3 and T4 according to AJCC (American Joint Committee of Cancer) classification. Remaining patients that were in lower stages were treated with complete excision under local anesthesia using the ‘no touch’ technique with a -4mm margin of normal-looking epithelium. No touch technique is a gentle technique without touching the tumor, since cells from these friable tumors can seed into adjacent tissues. Adjacent corneal epithelium was removed by alcohol and crescent knife. In case of scleral invasion, superficial lamellar sclerectomy was performed. Cryotherapy was applied to the remaining conjunctival edges, and alcohol was applied to the base of lesion. Large conjunctival defects were reconstructed with Amniotic Membrane Transplantation (AMT) in patients with wide tumors. Patients with stage T1 and T2 tumors were further treated with 0.02% MMC four times a day on a week-on-week–off basis for 2-4 cycles according to clinical findings during follow-up.
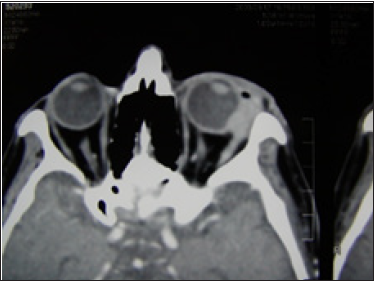
Figure 1a: Advanced conjunctival carcinoma that invaded fornices.

Scar tissue and suspicious lesions involving whole surface were observed in one patient in stage T3 disease who has been previously operated on 8 times. After topical MMC administration, a wide excision with AMT was performed. The lesions continued growing intraorbitally, so the patient was opted for subtotal exenteration (Figures 1a & 1b). The stage T4 tumor in the other patient involved fornices, resulting in absolute vision loss. Therefore subtotal exenteration was carried out. All patients were followed on increasing intervals and a complete eye examination performed at every visit. All treatment complications and recurrences were recorded. Statistical tests were mainly used to investigate the relationship between recurrence and histopathological subtype. Chi-square test was used to compare percentages, and statistical significance was set at P<0.05. Statistical analysis was performed through SPSS Windows version 16 (SPSS, Inc., Chicago, IL).
Figure 1b: CT of the same patient.
Results
Thirty eight eyes of 37 patients were included in this study. Fourteen were female and 23 were male. Mean age of patients was 65.97±14.03 (range: 29-90 years). Pathological diagnosis was conjunctival intraepithelial neoplasia in 22 eyes, Carcinoma In Situ (CIS) in 6 eyes and invasive squamous carcinoma in 10 eyes. Right eye was affected in 20 patients and left eye was affected in 16 patients. The disease occurred bilaterally two years apart in one patient. Localization of conjunctival lesion was at medial limbus in 27 eyes, at lateral limbus in 2 eyes, at multiple quadrants in 7 eyes and diffuse in 2 eyes. Tumor was primary in 28 eyes. Ten eyes had a history of surgery, where 5 patients were operated on once, one patient 4 times, and one patient 8 times for conjunctival tumor. Each of the remaining 3 patients had a history of pterygium surgery and there were no histopathology reports. Mean follow up time was 32.53±21.45 (min:6, max:84) months. Data is shown at (Table 1). Clinical appearances of lesions were very diverse. (Figures 2a-2c) shows leucoplakic, papilliform and diffuse form of OSSN. A large gelatinous OSSN lesion with brown patches is shown in (Figure 3). Table 2 shows histopathological distribution according to status of primary or previously recurrent. Although statistically insignificant, previously recurrent cases are highest in invasive SCC group and lowest in CIN group (Table 2).
Table 1:Summary of patient characteristics.
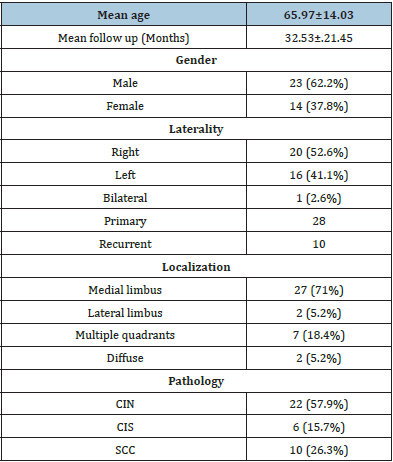
Figure 2a: Leukoplakic type of OSSN.
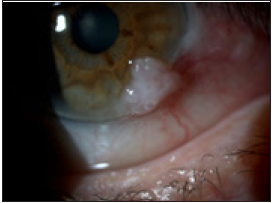
Figure 2b:Papillomatous type of OSSN.
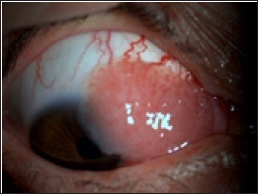
Figure 2c: Diffuse type of OSSN.
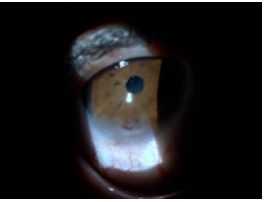
Figure 3: Large gelatinous OSSN lesion, with brown patches.

Table 2:Distrubition of primary and recurrent cases according to histopathological stage. CIN: Conjunctival Intraepitelial Neoplazia, CIS: Carcinoma In Situ, SCC: Squamous Cell Carcinoma.
In one case with sclerectomy, during postoperative period, scleral patch and AMT were needed because of scleral thinning. The tumor recurred in one patient after 6 years. Patient was reoperated and treated with postoperative topical MMC again. The patient with 8 previous surgeries was treated with preoperative MMC and wide excision with AMT. Upon failure, this was followed by exenteration. No complications were observed in this patient. The patient treated with subtotal exenteration presented with preauricular lymphadenopathy after 19 months and was referred to the oncology department. Five patients suffered from side effects of the drug while being treated with postoperative adjunctive MMC. In these cases adjuvant therapy was chased until the signs related to irritation healed. Afterwards, the treatment protocol was completed. This protected patients from serious side effects related to topical MMC treatment.
Discussion
Today, the treatment of choice for conjunctival malign tumors is a
wide local excision accompanied by cryotherapy to the conjunctival
edges. Cryotherapy and radiation therapy were used in order to
decrease recurrence rates but alternative treatment methods
have been searched due to high recurrence rates and serious
complications. Radiation therapy is not preferred anymore due to
complications such as dry eye syndrome, cataract, scleral ulceration
and scar formation. In recent years, topical chemotherapeutic
agents like INF- α2b , MMC, 5-FU and cyclosporine for treatment of
conjunctival neoplasia were searched and successful results were
reported [12,13]. The recurrence rate was 2.7% in 36 noninvasive
(stage T1 and T2) OSSN cases in this series. We routinely performed
adjunctive cryotherapy and postoperative topical MMC. Recurrence
rates for OSSN were reported to be as high as 53% with simple
excision alone [3]. Combining cryotherapy to conjunctival edges
resulted in a significant decrease in recurrence rates. Reported
recurrence rates range from 0% to 12.3% after surgical excision
combined with cryotherapy [5,6,7,20]. Sudesh et al. showed a
7.7% recurrence rate for excision combined with cryotherapy,
compared to 28.5% for simple excision in primary tumors in
their retrospective study [5]. Galor et al. [21] reported a 0.51 fold
decrease in recurrence rate with adjuvant cryotherapy [21]. Current
evidence supports that cryotherapy effectively destroys residual
tumor cells that may be left behind and reduces recurrence rates.
Complications of cryotherapy include corneal scarring and
pannus, iris atrophy, ocular hypotony and conjunctival scarring
[22]. We didn’t observe any transient or permanent complications
related to cryotherapy. Main reason for such complications is
excessive freezing. This should be avoided especially if it is applied
to scleral bed. MMC for OSSN treatment was first described by
Frucht-Perry et al. [23]. The complete cure rate ranges between
82% and 100% when used as a monotherapy or combined with
surgical excision [24]. Birkholz et al. [25] reported a significantly
reduced prevalence of recurrence with the adjunctive MMC (5.9%
vs. 66.7%) in their retrospective review [25]. Gupta et al. [9] also
showed no recurrence in 73 localized primary tumors treated with
surgery and accompanied with cryotherapy and postoperative
MMC in their prospective study [9]. In a previous study of Soysal
et al. [10] 16 cases with tumor cells in at least one surgical margin
were treated with postoperative adjuvant MMC. Throughout
a mean follow up period of 29 months, no recurrences were
observed [10]. In recent years, there has been a trend towards
using topical chemotherapies in treating OSSN as an alternative to
surgery. A survey in 2012 reported that 58% of ophthalmologists
used topical monotherapy in OSSN, and an increase in the use of
postoperative topical therapy was noted compared to 2003 survey
[26]. We don’t employ chemotherapy as a monotherapy. We think
that it is more ideal to have a pathologic confirmation of the
disease with excisional biopsy. Sometimes it is difficult to evaluate
invasiveness with imaging methods alone. Furthermore, surgical
excision provides significant debulking of tumor that results in a
shorter time for healing. Although very successful results have
been reported, especially with interferon monotherapy, it requires
a very long period of time, and has high cost, which adds to its
disadvantage. On the other hand, postoperative MMC treats the
whole surface of conjunctiva and presumably eliminates neoplastic
cells in extralesional regions, thus decreases the recurrence rates
[27].
Common side effects of MMC are usually transient and mild
including allergy, epiphora, and punctate epithelial keratopathy.
Serious complications due to limbal stem cell deficiency may be
observed occasionally. We didn’t observe any serious side effects
during any of the follow up. This result may be due to the temporary
interruption of topical chemotherapy when we observe slight side
effects. We had 2 cases with local invasion. One of these patients
had 8 previous surgeries. The other patient was a neglected case
presented with absolute vision loss. Conjunctival squamous cell
carcinoma tends to grow superficially first, but it can invade deeper
structures if not treated. Sclera and Bowman’s layer act as a barrier
against invasion in most cases. Majority of the invasive cases in
the literature are previously operated patients where these layers
are impaired [26]. It should be noted that 3 of the 4 patients with
scleral invasion had a history of surgical intervention in this case
series. SCC rates are also higher as insufficient surgery facilitates
transformation from intraepithelial stage to the invasive stage in
recurrent cases (Table 2). Failure to differentiate from pterygium
and eventually incomplete excision of the lesion is not uncommon.
Therefore, all excised conjunctival lesions should be sent to
histopathological evaluation. The patient with advanced squamous
cell carcinoma (T4) that involved fornices causing absolute vision
loss was treated with subtotal exenteration. However, the patient
was presented with preauricular lymphadenopathy and was
referred to oncology department 19 months later. For the other
patient with 8 previous surgeries, we initially performed wide
excision with preoperative and postoperative topical MMC. However,
since the tumor continued to grow intraorbitally, an exenteration
was carried out. Local tumor excision may be performed in some
advanced cases, but intraocular invasion generally necessitates
enucleation or exenteration. In the study of Miller et al., 71% of the
38 cases with SCC greater than stage T3 were treated with local
tumor excision and 28% were treated with orbital exenteration
[28]. Despite a 52% recurrence rate in the first group of patients,
none were reported to require an orbital exenteration.
In conclusion, despite the new developments and facilities
regarding the early diagnosis and treatment of the OSSN,
recurrences and treatment complications still exist. These
recurrences and side effects impair success rate by increasing
morbidity. The course of the cases that have a history of previous
surgery is more challenging. We recommend a complete excision
followed by cryotherapy and routine postoperative adjuvant MMC
application to decrease the number of unsuccessful results.
Acknowledgement
The authors declare that they have no conflict of interest. Informed consent was obtained from all individual participants included in the study.
References
- Lee GA, Hirst LW (1992) Incidence of ocular surface epithelial dysplasia in metropolitan brisbane. A 10-year survey. Archives of Ophthalmology 110(4): 525-527.
- Carreira H, Coutinho F, Carrilho C, Lunet N (2013) HIV and HPV infections and ocular surface squamous neoplasia: Systematic review and meta-analysis. British Journal of Cancer 109(7): 1981-1988.
- Tabin G, Levin S, Snibson G, Loughnan M, Taylor H (1997) Late recurrences and the necessity for long-term follow-up in corneal and conjunctival intraepithelial neoplasia. Ophthalmology 104(3): 485-492.
- Shields JA, Shields CL, De Potter P (1997) Surgical management of conjunctival tumors. The 1994 Lynn B. McMahan lecture. Archives of Ophthalmology 115(6): 808-815.
- Sudesh S, Rapuano CJ, Cohen EJ, Eagle RC, Laibson PR (2000) Surgical management of ocular surface squamous neoplasms: The experience from a cornea center. Cornea 19(3): 278-283.
- Nanji AA, Moon CS, Galor A, Sein J, Oellers P et al. (2014) Surgical versus medical treatment of ocular surface squamous neoplasia: A comparison of recurrences and complications. Ophthalmology 121(5): 994-1000.
- Li AS, Shih CY, Rosen L, Steiner A, Milman T et al. (2015) Recurrence of ocular surface squamous neoplasia treated with excisional biopsy and cryotherapy. American Journal of Ophthalmology 160(2): 213-219.
- Ballalai PL, Erwenne CM, Martins MC, Lowen MS, Barros JN (2009) Long-term results of topical mitomycin C 0.02% for primary and recurrent conjunctival-corneal intraepithelial neoplasia. Ophthalmic Plastic and Reconstructive Surgery 25(4): 296-299.
- Gupta A, Muecke J (2010) Treatment of ocular surface squamous neoplasia with Mitomycin C. Britis Journal of Ophthalmology 94(5): 555-558.
- Soysal Gokmen H, Yazar Z (2008) The efficacy of postoperative topical Mitomycin C in the treatment of conjunctival surface neoplasia. Turkish Journal of Ophthalmology 38(6): 464-467.
- Parrozzani R, Lazzarini D, Alemany Rubio E, Urban F, Midena E (2011) Topical 1% 5-fluorouracil in ocular surface squamous neoplasia: A long-term safety study. British Journal of Ophthalmology 95(3): 355-359.
- Bahrami B, Greenwell T, Muecke JS (2014) Long-term outcomes after adjunctive topical 5-flurouracil or Mitomycin C for the treatment of surgically excised, localized ocular surface squamous neoplasia. Clinical and Experimental Ophthalmology 42(4): 317-322.
- Krilis M, Tsang H, Coroneo M (2012) Treatment of conjunctival and corneal epithelial neoplasia with retinoic acid and topical interferon alfa-2b: Long-term follow-up. Ophthalmology 119(10): 1969-1973.
- Mills RA (2014) Ocular surface squamous neoplasia: to cut or not to cut. Clinical and Experimental Ophthalmology 42(4): 307-308.
- Teng CC, Chin KJ, Finger PT (2009) Subconjunctival ranibizumab for squamous cell carcinoma of the conjunctiva with corneal extension. British Journal of Ophthalmology 93(6): 837-838.
- Cervantes G, Rodríguez AA, Leal AG (2002) Squamous cell carcinoma of the conjunctiva: Clinicopathological features in 287 cases. Canadian Journal of Ophthalmology 37(1): 14-19.
- Graue GF, Tena LB, Finger PT (2011) Electron beam radiation for conjunctival squamous carcinoma. Ophthalmic Plastic and Reconstructive Surgery 27(4): 277-281.
- Rootman DB, McGowan HD, Yücel YH, Pavlin CJ, Simpson ER (2012) Intraocular extension of conjunctival invasive squamous cell carcinoma after pterygium surgery and cataract extraction. Eye and Contact Lens 38(2): 133-136.
- Iliff WJ, Marback R, Green WR (1975) Invasive squamous cell carcinoma of the conjunctiva. Archives of Ophthalmology 93(2): 119-122.
- Palamar M, Kaya E, Egrilmez S, Akalin T, Yagci A (2014) Amniotic membrane transplantation in surgical management of ocular surface squamous neoplasias: long-term results. Eye 28(9): 1131-1135.
- Galor A, Karp CL, Oellers P, Kao AA, Abdelaziz A, et al. (2012) Predictors of ocular surface squamous neoplasia recurrence after excisional surgery. Ophthalmology 119(10): 1974-1981.
- Peksayar G, Soytürk MK, Demiryont M (1989) Long-term results of cryotherapy on malignant epithelial tumors of the conjunctiva. American Journal of Ophthalmology 107(4): 337-340.
- Frucht-Pery J, Rozenman Y (1994) Mitomycin C therapy for corneal intraepithelial neoplasia. American Journal of Ophthalmology 117(2): 164-168.
- Peer J (2015) Ocular surface squamous neoplasia: Evidence for topical chemotherapy. International Ophthalmology Clinics 55(1): 9-21.
- Birkholz ES, Goins KM, Sutphin JE, Kitzmann AS, Wagoner MD (2011) Treatment of ocular surface squamous cell intraepithelial neoplasia with and without mitomycin C. Cornea 30(1): 37-41.
- Adler E, Turner JR, Stone DU (2013) Ocular surface squamous neoplasia. Cornea 32(12): 1558-1561.
- Hirst LW (2007) Randomized controlled trial of topical mitomycin C for ocular surface squamous neoplasia: Early resolution. Ophthalmology 114(5): 976-982.
- Miller CV, Wolf A, Klingenstein A, Decker C, Garip A et al. (2014) Clinical outcome of advanced squamous cell carcinoma of the conjunctiva. Eye 28(8): 962-967.
© 2021 Hülya Gökmen Soysal. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






