- Submissions

Full Text
Medical & Surgical Ophthalmology Research
Computerized Ophthalmic Diagnostic Testing: An Engineer Looks Back at Lessons Learned
Harley R Myler*
Professor of Electrical Engineering, Lamar University, USA
*Corresponding author: Harley R Myler, Professor of Electrical Engineering, Lamar University, USA
Submission: December 8, 2020;Published: December 15, 2020

ISSN 2578-0360 Volume3 Issue1
Opinion
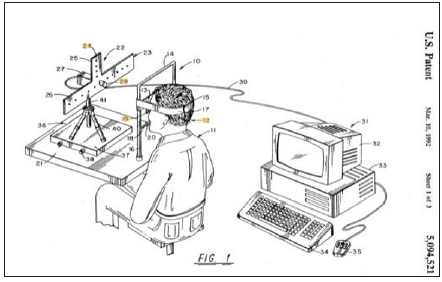
Over thirty years ago and along with two other colleagues, one an ophthalmologist (MD), I invented a device that we called the Trophorometer a device to “measure tropias (manifest ocular misalignment) and phorias (latent deviation compensated for by the fusional reflex) to within one to two degrees” [1]. This was not my first foray as an engineer into the fascinating world of ophthalmology as I had designed and coded a system for the American Academy of Ophthalmology to allow practitioners to track and bill patients-this was a new concept back then and although I was well-paid as a consultant in the project, it really was not my passion. Since then, others have taken up patient database development and done a commendable job. My involvement in the design and construction of a proof-of-principle model of the Trophorometer was due to my expertise in computer vision. (Figure 1) (from the patent [1]) illustrates the basic concept of the device. Clinicians and anyone who has had a general eye exam will immediately recognize the architecture. The patient sits in front of the device and rests their chin on a rest and looks into the device. For our prototype we employed a bitebar and a head restraint because we had to have absolute fixation and no eye movement. We identified the pupil using a generalized Hough Transform [2] and achieved very good results. Our goal was to provide a rapid and inexpensive technique for screening children for strabismus. What we had not considered was the fact that the existing method of strabismus evaluation would make our invention a white elephant.
Figure 1:Design and construction of a proof-of-principle model of the Trophorometer.
Shortly after we patented our device, we consulted with a pediatric ophthalmologist to solicit his opinion as to the salability of our new device. He listened to our presentation, which included diagrams and data run from our instrument-and at this point I will add that one of our inventors had a somewhat severe and uncorrected lateral trope so he made an excellent subject for evaluating the device. The doctor then asked how much the machine would cost and we said in the neighborhood of $10K in 1990’s dollars. Then he told us that no one would buy it. We were shocked and asked why given how automated and accurate our device was. He then explained that the way strabismus is measured is via a set of prisms, which he then showed us. A good set of prisms at the time ran roughly $400 and they can be found on the Internet for significantly less than that. For any practice to invest in an instrument, the cost of said device would have to have a payback of three or four years and our instrument would not be cost effective as insurance companies would not pay for an exam with it given that the far less expensive prism exam was available. In fact, using prisms to evaluate strabismus exists to this day [3].
Conclusion
So, the moral of this story is that although a practitioner might have a good idea and also have access to colleagues with the requisite engineering skills to implement it, a major consideration is the ultimate marketability of the device. What we failed to do was look at what our Trophorometer would be replacing and that inexpensive set of prisms was not going to be dethroned.
References
- Jolson Alfred S, Myler Harley R, Weeks A (1990) Apparatus for evaluating eye alignment. USA.
- Duda RO, Hart PE (1972) Use of the hough transformation to detect lines and curves in pictures. Comm ACM 15(1): 11-15.
- Antony J (2017) Prisms in clinical practice. Kerala J Ophthalmol 29(2): 79-85.
© 2020 Harley R Myler. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






