- Submissions

Full Text
Medical & Surgical Ophthalmology Research
Unexplained Visual Loss; Different Etiologies, Costs and Diagnostic Guideline Proposal
Hassan Khojasteh, Mostafa Mafi*, Masoud Aghsaei Fard, Mina Ojani, Bita Momenaei, Fereshteh Tayebi and Masoud Mirghorbani
Eye Research Center, Farabi Eye Hospital, Tehran University of Medical Sciences, Tehran, Iran
*Corresponding author: Mostafa Mafi, Eye Research Center, Farabi Eye Hospital, Tehran University of Medical Sciences, Tehran, Iran
Submission: August 02, 2019;Published: September 19, 2019

ISSN 2578-0360 Volume2 Issue5
Abstract
Purpose: to present a practical approach for unexplained visual loss.
Methods: In a prospective case series, we documented characteristics, clinical and paraclinical evaluations, relevant costs and the final diagnosis of patients referred to a tertiary eye hospital for evaluation of unexplained visual loss with no apparent structural abnormalities.
Results: 28 cases were documented. 9(32%) out of all referred patients were found to have nonretinal/ neurologic pathologies, while 19(68%) had a retinal/neurologic disorder. Different conditions masqueraded as non-organic visual loss including central visual pathway pathology, serous chorioretinopathy, occult macular dystrophy, inherited optic neuropathies and autoimmune retinopathies. In 30% of cases, the final diagnosis was made based on optical coherence tomography (OCT). Also, in many other cases, findings of OCT were helpful to rule out other diagnosis. Electrophysiologic tests including full field electroretinogram (ERG) and visual evoked potential (VEP) were the key in diagnosis of various conditions including central visual pathway pathology, retinal dystrophy, and autoimmune retinopathy. Unnecessary expenditure spent by each patient and all cases was estimated to be 72.5 US$ and 2028.8 US$ respectively (about 44.5 % of the total amount of expenditure spent on each case).
Conclusion: We proposed a practical approach for this group of cases in an attempt to prevent unnecessary paraclinical investigations and to alleviate the socio-economic burden of both patients on the health system.
Keywords: Visual loss; Unexplained visual loss; Electrophysiology; Macula; Dystrophy; Neuroophthalmology
Introduction
Unexplained visual loss (UVL) is one of the challenging problems are faced by ophthalmologists and is defined as decreased best-corrected visual acuity (BCVA), which cannot be explained by underlying pathology of visual pathways or is out of proportion of identifiable lesion [1,2]. UVL is a common problem among patients presenting to ophthalmic care services and neuro-ophthalmology clinic, which poses distress and anxiety to both patients and physicians [3,4]. It is necessary to search for any definable pathology of decreased vision before arriving at the diagnosis of functional vision loss (FVL) which is a label that affects further investigations as well as treatment strategies [5]. Scott and Egan have shown that organic etiologies account for a large proportion of UVL with more than half of the patients with FVL had concurrent organic disease [6]. Herein, we describe the final diagnosis of 28 cases with application of our step-by-step approach to discover the etiology of UVL more rapidly to prevent unnecessary and irrelevant paraclinical testing. Since there is not a well stablished diagnostic protocol for UVL, we believe that the application of this approaches would decrease the cost imposed on both the patients and the health system in addition to other benefits such as protection of patients from exposure to side effects of some diagnostic modalities.
Methods
This prospective case series included patients who were referred to retina clinic of eye hospital - a tertiary eye care center in Tehran- for evaluation of the possibility of a retinal pathology for UVL between February 2017 to June 2017. After obtaining informed consent, patients with complaint of decreased visual acuity without accountable structural abnormality examined by previous ophthalmologist were recruited in the study. The following data were collected from the medical records of patients: demographic information, pattern of decreased vision, initial BCVA, duration of the symptoms, time from the first visit to presentation to our clinic, number of workups done before and amount of money spent by patients as well as the expenses imposed on medical insurances for each workup. Then we started to approach to each patient based on our step-by-step algorithm (Figure 1) which starts with rechecking BCVA based on subjective refraction. Ophthalmologic examinations included the following for all the patients:
a) Slit-lamp examination of anterior and posterior segment with +90 diopter lens and other ocular structures.
b) Relative afferent pupillary defect (RAPD) examination by the swinging flashlight method [7].
c) Goldmann applanation tonometry.
d) Ocular motility examination including cover-uncover and Hirschberg test.
e) For relevant cases these tests were done accordingly: f) Fogging tests with gradually increasing power of plus lenses which were placed before the unaffected eye and the vision was measured with the affected eye while both eyes were open.
g) Worth 4-dot test and stereoacuity testing to find the presence of peripheral fusion with the absence of bifoveal fusion for diagnosis of the monofixation syndrome (MFS) [8].
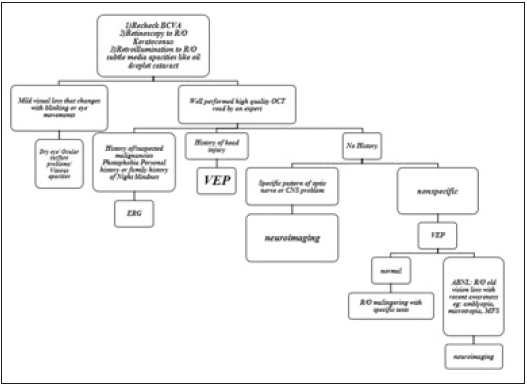
Figure 1:The proposed approach to a patient with unexplained visual loss
In any stage, if the final diagnosis could be made or any structural pathology could explain the corresponding decreased visual acuity, we would terminate our investigations. Otherwise, further evaluations were performed until we came to a conclusion. We reviewed the results of previous documents including macular and retinal nerve fiber layer (RNFL) optical coherence tomography (OCT), fluorescein angiography (FA), standard achromatic automated perimetry visual fields (VF), electroretinography (ERG), electrooculography (EOG), visual evoked potential (VEP), brain magnetic resonance imaging (MRI) and orbital computerized tomography scan (CT), if needed based on our approach protocol. We excluded the cases in which the final diagnosis could be made by the reviewing of previous imaging and tests done in other centers and only included the inconclusive situations in which additional workups were requested. All data were collected and statistical analyses were performed using SPSS version 23 (SPSS Inc., Chicago, IL, USA).
Compliance with ethical standards
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Results
Patient characteristics
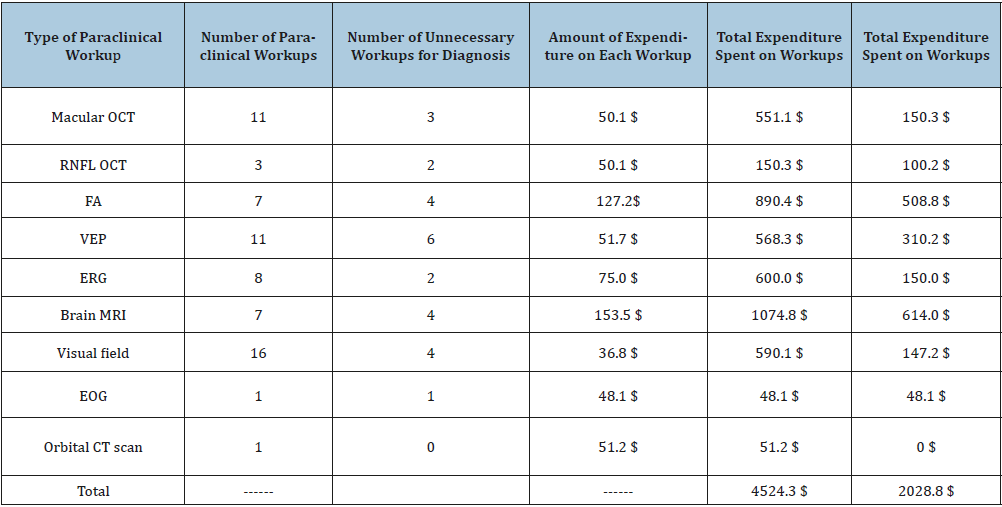
We evaluated 28 cases referred to our clinic from other medical specialties for further workups for UVL. They consisted of 18 Males and 10 Females. The mean age of symptom onset in cases was 27.6 (standard deviation (SD): 10.7 years, range: 12- 62). The mean duration of symptoms prior to presentation to our center was 7.75 months (range 2-13). The median level of visual acuity for the affected eyes was 6/20 with the range of 16/20 to light perception. Paraclinical testing and imaging performed by other ophthalmologist or neurologist consultants for all the cases included 11 macular OCT, 3 RNFL OCT, 7 FA, 11 VEP, 8 ERG, 7 brain MRI, 16 VF, 1 EOG, and 1 orbital CT scan. Considering the fact that, US$ 1.00 was equal to 42000 Iranian Rials at the time of analyzing the data of this article, the mean estimated expenditure on these paraclinical testing for all the patients was 4524.3 US$ with the mean amount of 161.6 US$ spent by each patient. After application of our step-by-step approach protocol to each patient to find the relevant pathology and to make the final diagnosis, we defined the number of unnecessary or irrelevant workups as well as the waisted expenditure on them (Table 1). The amount of unnecessary expenditure spent by each patient and all cases was 72.5 US$ and 2028.8 US$ respectively which equals to 44.5 % of the total amount of expenditure spent on each case. Based on final diagnosis, the cases were categorized into Non- retinal diagnosis and Retinal/ Neurologic diagnosis. It is worth saying there was no statically significant difference between these groups in terms of age, sex and initial BCVA at presentation (P>0.05).
Table 1: Expenditure on unnecessary paraclinical workups; CT=Computed Tomography; EOG= Electrooculogram; ERG=Electroretinogram; FA=Fluorescein Angiography; MRI=Magnetic Resonance Imaging; OCT=Optical Coherence Tomography; RNFL=Retinal Nerve Fiber Layer; VEP=Visual Evoked Potential.
Non- retinal diagnosis
We found two cases of 20/20 BCVA after repeating visual acuity (VA) measurement and subjective refraction. In one case retinoscopy revealed faint scissor reflex and requested corneal topography was compatible with a diagnosis of forme fruste keratoconus (KCN), while the amount of astigmatism was less than 2 diopters. Two cases were diagnosed as having monofixation syndrome after referral to strabismus clinic for further evaluation because of microtropia and prolonged history of decreased vision. In two cases, ocular surface disorders including dry eye disease and blepharitis were found to be the etiology of decreased vision which was intermittent. In one case mild cataract, which was more prominent in retinoscopy rather than slit lamp examination, was the companion etiology. Finally, two patients were diagnosed with malingering based on disproportionate decreased VA despite normal ocular or brain evaluating, which were confirmed with fogging test.
Retinal/neurologic diagnosis
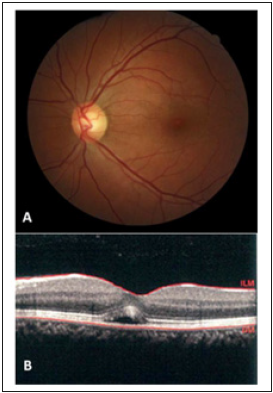
Four patients were diagnosed as occult macular dystrophy after careful interpretation of their fundus OCT and based on normal findings of ERG. We found five cases of retinal dystrophy (three cases of cone-rod and two cases of rod-cone dystrophy), which were diagnosed simply by ERG. All of these cases had near normal or normal fundi with no bony spicule which made the diagnosis impossible by examination only (Figure 2). Two cases had mild, shallow chronic central serous chorioretinopathy (CSCR) which was evident in OCT; FA confirmed the diagnosis which shows the expansile dot pattern of leakage (Figure 3). Three cases of hereditary optic neuropathy were diagnosed according to RNFL OCT loss and color vision testing. There was one case of melanomaassociated retinopathy (MAR) and one case of cancer-associated retinopathy (CAR) both of which had normal fundus appearance and macular OCT but the former had a history of melanoma for 5 years and the latter had a history of breast cancer for 3 years. ERG confirmed the diagnosis for both cases with severely reduced a- and b- wave signals. Eventually, VEP revealed the diagnosis of central visual pathway pathology in three cases with a past history of head trauma Table 2. summarizes the presentation features of the patients as well as the number of paraclinical tests done for each case before presentation to our clinic, the relevant diagnostic tests we ordered based on our approach protocol and the final diagnosis made for each case accordingly.
Table 2:the presentation features of the patients and final diagnosis; CSCR=Central Serous Chorioretinopathy; CT=Computed Tomography; EOG=Electrooculogram; ERG=Electroretinogram; FA= Fluorescein Angiography; KCN=Keratoconus; MAR=Melanoma Associated Retinopathy; CAR=Cancer Associated Retinopathy; MFS=Monofixation Syndrome; MRI=Magnetic Resonance Imaging; OCT=Optical Coherence Tomography; PERG=Pattern Electroretinogram; RNFL=Retinal Nerve Fiber Layer; VEP=Visual Evoked Potential.
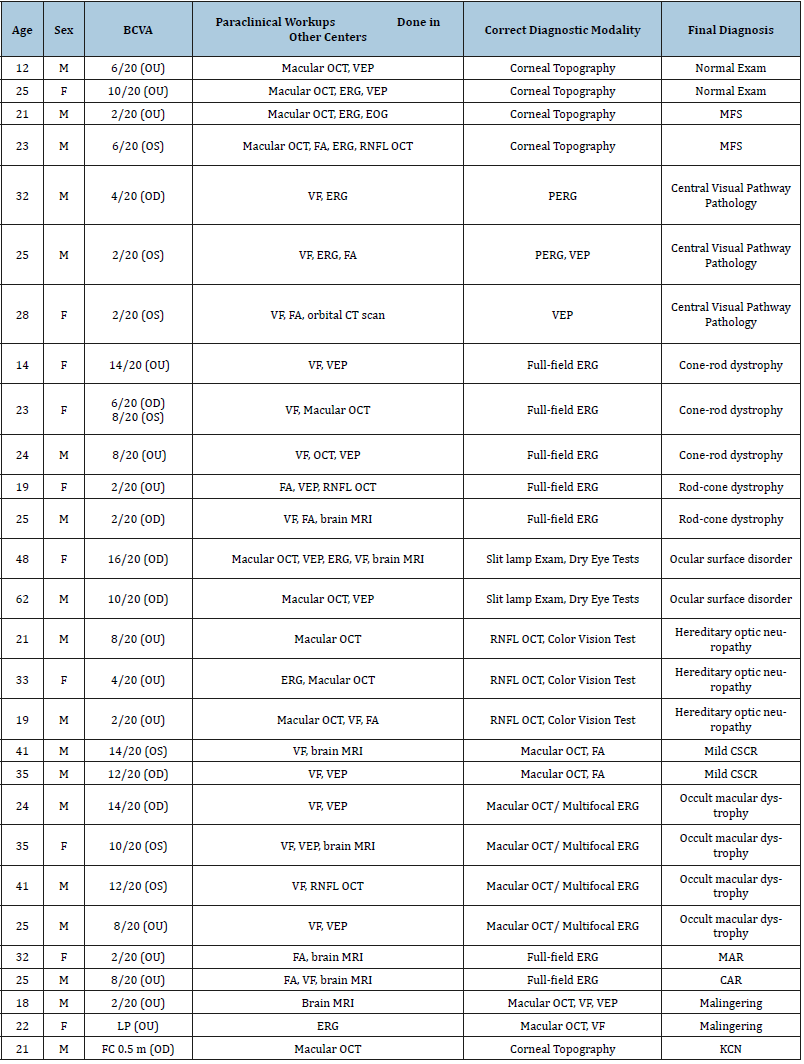
Figure 2:Severely reduced flicker and scotopic response in a case of retinitis pigmentosa sine pigmento.
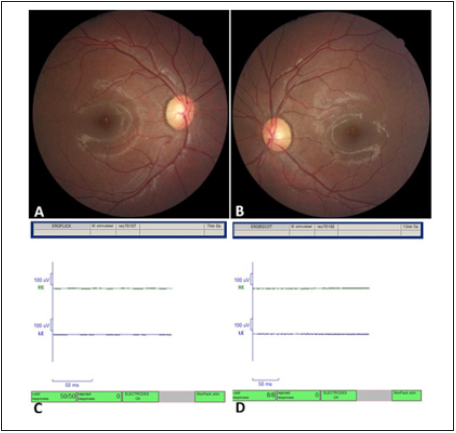
Figure 3:Neurosensory detachment in optical coherence tomography (OCT) with normal fundus photo and examination compatible with the diagnosis of central serous chorioretinopathy.
Discussion
Approach to a patient with UVL remains a matter of concern. In the literature review, there was no previous study to guide ophthalmologists on how to approach to these groups of patients to avoid excessive and unnecessary paraclinical workups. In this prospective case series, 9 (32%) out of all referred patients for probable retinal pathology for decreased vision were found to have non-retinal pathologies. Some of these could be simply discovered by a thorough history taking e.g. two patients were found to have amblyopia after showing evidence of decreased VA from childhood and they were referred to strabismus clinic and were diagnosed as MFS. History of intermittent decreased VA could also raise the suspicion of an ocular surface disease and preclude further costly investigations. Two patients (7%) in this study had functional vision loss due to malingering. This is in concordance with a study by Villegas and IIsen who reported that between 5%-12% of patients referring with visual loss to neuro-ophthalmology clinic were subsequently diagnosed with medically unexplained/functional visual loss [9]. Again, FVL is estimated to account for approximately 5% of cases in a general ophthalmology practice in other studies [10]. On the other side Scott et al, found that about 53% of patients with functional visual loss had concurrent organic pathology. So, in the context of functional features, searching for an organic disease should be kept in mind [6]. There are different conditions that can masquerade as non-organic visual loss including occult macular dystrophy, cortical visual impairment, inherited optic neuropathies and autoimmune retinopathies [1,11]. 14% of their patients were diagnosed with occult macular dystrophy. These patients had normal examination with original unremarkable EOG, ERG studies and only careful interpretation of OCT showed localized disruption of outer retinal layers and multifocal ERG demonstrates the abnormality of central retina [12,13]. Inherited optic neuropathy is another condition sometimes diagnosed as FVL incorrectly [11]. Careful history taking regarding the existence of such a condition especially among the male members of the family and relevant testing like RNFL OCT and color testing and VEP could make the diagnosis. Similarly, three of our patients were diagnosed as autosomal dominant optic atrophy. We believe that macular OCT plays a pivotal role in diagnosis of UVL and therefore we consider it at the earlier stages of our approach protocol (Figure 1). With the help of non-invasive OCT imaging, a large percentage of patients previously labeled with UVL due to missed retinal pathology during fundus examination were excluded from this category of diagnosis. In our study, in about 30% of the patients the final diagnosis was made based on OCT and in many other findings of OCT was necessary to rule out other diagnosis.
Electrophysiologic tests could provide beneficial tests in visual loss of unexplained etiology [14]. In a review of 410 subjects referred for visual electrophysiology from neuro-ophthalmologists, electrophysiology including pattern, full-field, and multifocal ERG and pattern, flash and multifocal VEP were effective in differentiating between retinopathy, post-retinal pathology and normality in 91% of subjects [15]. In another study by Renner on 72 patients with UVL, combined evaluation of VEP and multifocal ERG were useful to localize the area of dysfunction and defining the normality of the visual pathway. They recommended electrophysiologic testing prior to neuroimaging in patients with no clinical evidence of cerebral disorders in order to reduce the frequency of unnecessary neuroimaging and exposure to radiation [16]. In the present series, electrophysiologic tests including full-field ERG, and VEP were the key in diagnosis of various conditions including central visual pathway pathology, retinal dystrophy, and autoimmune retinopathy. We believe that these tests should be ordered in the context of recent or previous history of head trauma, family history of decreased vision, past medical history of cancer/melanoma, or an autoimmune disease. We found many unnecessary or irrelevant workups done by other medical specialties before referring patients to our clinic which inflict a large amount of expenditure on both patients and health insurances. Based on our estimation for each patient 161.6 US$ was spent as paraclinical workup expenses -based on the tariffs in governmental hospitals and not private ones which are much higher- to find out the etiology for UVL before they were referred to our clinic. After application of our given approach, we found that about 45 percent of this amount of expenditure was unnecessary and preventable besides the amount of preventable wasted time spent by each patient for these tests. As shown by other investigates this amount of wasted money and time imposes a huge socioeconomic burden to both patients and health system meanwhile leads to an unreasonable increase in number of visits by the physicians and also generates stress and anxiety in patients.
In our tertiary center, we are frequently encountering many UVL patients for whom lots of workups for evaluation of all probable sites of decreased vision including the retina, optic nerve or brain have been requested by ophthalmologists or neurologists regardless of the chief complain of the patients and/ or their family history of decreased vision. We believe that taking history-based approaches for UVL like what we have proposed here, will lower the frequency of visits by the physicians, the amount of time wasted for any workup or visit and the stress and anxiety imposed to patients before and after each workup. Some of these tests are invasive and stressful for patients such as electrophysiologic tests and taking such an approach will prevent the unwanted early and late adverse effects of some paraclinical tests like hypersensitivity reactions to contrast or fluorescein, anaphylaxis, ionizing radiation side effects, etc. This study has limitations as well. Some data were selfreported, and it is difficult to be validated independently. The small sample size is another limitation. In addition, the history-based approach protocol we applied for UVL was based on our experience and further studies are needed to validate our proposed algorithm by defining the specificity and sensitivity for each paraclinical test. Evaluation of patients with a primary diagnosis of UVL who referred to ophthalmologic clinics is almost always a challenging matter. Application of history-based approaches like what we proposed here is a beneficial guide to a quicker, more accurate and more economical diagnosis of the masquerader conditions in cases known as UVL.
References
- Griffiths PG, Ali N (2009) Medically unexplained visual loss in adult patients. Curr Opin Neurol 22(1): 41-45.
- Griffiths PG, Eddyshaw D (2004) Medically unexplained visual loss in adult patients. Eye (Lond) 18(9): 917-922.
- Nimnuan C, Hotopf M, Wessely S (2001) Medically unexplained symptoms: an epidemiological study in seven specialities. J Psychosom Res 51(1): 361-367.
- Kathol RG, Cox TA, Corbett JJ, Thompson HS, Clancy J (1983) Functional visual loss: I. A true psychiatric disorder? Psychol Med 13(2): 307-314.
- Acosta PC, Trobe JD, Shuster JJ, Krischer JP (1981) Diagnostic strategies in the management of unexplained visual loss. A cost-benefit analysis. Med Decis Making 1(2): 125-144.
- Scott JA, Egan RA (2003) Prevalence of organic neuro-ophthalmologic disease in patients with functional visual loss. Am J Ophthalmol 135(5): 670-675.
- Bell RA, Waggoner PM, Boyd WM, Akers RE, Yee CE (1993) Clinical grading of relative afferent pupillary defects. Arch Ophthalmol 111(7): 938-942.
- Scott MHN, Nobel AG, Raymond WR, Parks MM (1994) Prevalence of primary monofixation syndrome in parents of children with congenital esotropia. J Pediatr Ophthalmol Strabismus 31(5): 298-301.
- Villegas RB, Ilsen PF (2007) Functional vision loss: a diagnosis of exclusion. Optometry 78(10): 523-533.
- Bose S, Kupersmith MJ (1995) Neuro-ophthalmologic presentations of functional visual disorders. Neurol Clin 13(2): 321-339.
- Buono LM, Foroozan R, Sergott RC (2003) Unexplained visual loss. Survey of Ophthalmology 48(6): 626-630.
- Brockhurst RJ, Sandberg MA (2007) Optical coherence tomography findings in occult macular dystrophy. Am J Ophthalmol 143(3): 516-518.
- Lubinski W, Goslawski W, Penkala K, Drobek-Slowik M, Karczewicz D (2008) A 43-year-old man with reduced visual acuity and normal fundus: occult macular dystrophy--case report. Doc Ophthalmol 116(2): 111-118.
- Matthews GP, Sandberg MA, Berson EL (1992) Foveal cone electroretinograms in patients with central visual loss of unexplained etiology. Arch Ophthalmol 110(11): 1568-1570.
- Yap GH, Chen LY, Png R (2015) Clinical value of electrophysiology in determining the diagnosis of visual dysfunction in neuro-ophthalmology patients. Doc Ophthalmol 131(3): 189-196.
- Renner AB, Kellner U, Tillack H, Kraus H, Foerster MH (2005) Recording of both VEP and multifocal ERG for evaluation of unexplained visual loss electrophysiology in unexplained visual loss. Doc Ophthalmol 111(3): 149-157.
© 2019 Mostafa Mafi. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






