- Submissions

Full Text
Medical & Surgical Ophthalmology Research
Photorefractive Keratectomy for Myopia: 100Hz Versus 500Hz Repetition Rate Excimer Laser
Hassan Razmjoo1, Farhad Fazel1, Zeynab Raei2* and Alireza Peyman3
1 Professor of Ophthalmology, Iran
2 Medical Student, Iran
3 Associated Professor of Ophthalmology, Iran
*Corresponding author: Zeynab Raei, Medical Student, Iran
Submission: September 04, 2018;Published: November 19, 2018

ISSN 2578-0360 Volume2 Issue4
Abstract
Propose: The aim of this study was to evaluate and compare the results of two devices with different repetition rates (100Hz Vs. 500Hz) in Photorefractive keratectomy (PRK) surgery.
Methods: In this research, we studied post-operative outcomes of PRK surgeries performed with two different repetition rates (100 and 500Hz). One-hundred-ten patients underwent PRK, 110 eyes with Technolas 217z100 and 110 eyes with Technolas 317. After 6 months uncorrected distant visual acuity (UCDVA), best-corrected distant visual acuity (BCDVA), refraction and wave-front aberrometry were compared between two groups.
Results: Ninety-four eyes (85.45%) in the 100Hz group and 98 eyes (89.09%) in the 500Hz group had a UCDVA of 20/20 or better at the last follow-up examination. The mean SE attempted correction was -3.68D±1.66 in 100Hz group and -3.80D±1.46 in 500Hz group respectively. About high order aberrations (HOAs), The mean of vertical coma, was 0.031±0.241μm in group 100Hz, and -0.062±0.285μm in group 500Hz. Mean postoperative vertical coma was significantly different between two groups (P=0.033). The vertical trefoil, horizontal trefoil and horizontal coma were not significantly different between the groups (P>0.05).
Conclusion: Both excimer laser systems were effective, improving the UCDVA in comparison with the pre-operation UCDVA. The results showed that Technolas 217z100 (100Hz repetition rate) in PRK surgeries might have better visual quality outcome.
Keywords: Photorefractive keratectomy; Myopia; Excimer laser; Refractive surgery; Ocular aberrations
Introduction
In many studies refractive surgery using an excimer laser is considered secure and efficient, with very good results [1,2]. However, prolongation of the ablation process will lower the ability of the patient to fixate thoroughly and increases the possibility of making the eye dry. One important feature of different lasers is the variety in their repetition rates [3]. Increasing pulse repetition rate without making impairment in eye-tracker latency, ablation depth of single pulse, and size of the spot, can help us to lower the treatment time [4]. Thus, it seemed rational to raise the repetition rate of the excimer lasers. Raising the repetition rate might cause significant changes in the ablation effect of the laser because of photochemical or photo-thermal changes that occur during the ablation process, such as ablation depth per pulse [5]. Increasing the repetition rate may lead to a raise in the transmission of mean laser power to the corneal surface, and this might result to a much higher temperature on the corneal surface during the ablation [4]. Measuring ocular aberrations, higher order aberrations (HOAs), after refractive surgery procedures, a correlation between reduced image quality and these aberrations, especially spherical aberrations and coma was found in many studies [6].
It is demonstrated that corneal and ocular aberrations (wave front aberrations) are significantly increased after laser refractive surgery and this increase correlates with the increase in loss of lowcontrast visual acuity and glare visual acuity [7]. Flying spot lasers by smaller spot sizes are introduced to improve the predictability and ability to correct lower- and HOAs. The use of smaller laser spots allows correction of specific substructures of aberrations, which is especially important in custom corneal surgery [8,9]. However, the smaller spot size increases treatment time if the excimer laser is not working at a high repetition rate. The interest in reducing the duration of refractive surgery procedures has risen the tendency to use excimer lasers with high repetition rates [10]. The purpose of this study is to evaluate and compare the visual outcomes and higher order aberrations in two excimer laser systems (Technolas 217z, and Technolas 317) with different repetition rates of 100 and 500Hz.
Material and Methods
Study design
This study comprised 220 eyes of 110 patients amongst 123 subjects who were visited and examined in ophthalmology clinic. These 110 patients underwent PRK surgery using scanning spot 100Hz laser and scanning spot 500Hz pulsed ArF laser (110 eyes in each group) and were followed between May 2016 and October 2016. The study approval was gained from the ethical committee and written informed consents were obtained from all patients before surgery. Inclusion criteria of the study was; age between 21 to 45 years, Best preoperative corrected distance visual acuity (BCDVA) of 0.00 log MAR or better, no previous eye surgery, spherical equivalent (SE) not more than -8, astigmatism not more than -4, no existing pathology in cornea and fundus (which can result in decreased corrected visual acuity or any disturbance in outcomes of the operation), and patients with myopia or myopiaastigmatism as refractive errors. Exclusion criteria were subjects not cooperating for follow up and patients suffering diabetes mellitus or autoimmune diseases. The patients and the person who analysed the data were not informed about the repetition rate used for the groups.
Surgical method
All procedures were performed by one surgeon. Eyes were anesthetized by instilling two drops of topical Tetracaine hydrochloride 0.5% two minutes apart before the procedure. During the procedure, the eyes were first irrigated with balanced salt solution and after exposure to alcohol 20% for 20 seconds, the epithelium was removed with a hockey knife and photoablation was performed. At the end, patients received Mitomycin 0.02% for 30 seconds then a bandage soft contact lens was placed over the cornea surface. After the surgery patients were prescribed topical ciprofloxacin and betamethasone drops 4 times daily for 7 days. The bandage soft contact lens was kept in place until full corneal reepithelialization. After re-epithelialization, patients were treated with fluorometholone sodium 2% (FML) 4 times daily for 4 weeks. No additional steroid drops were prescribed for patients.
Follow up setting
Postoperative follow-up after 6 months included; uncorrected distant visual acuity (UCDVA), BCDVA, refraction and wave front aberrometry. Using the wave-front aberrometer, elements such as vertical trefoil, horizontal trefoil, vertical coma, horizontal coma and spherical aberration were measured. UCDVA, BCDVA and manifest refraction were measured and compared between the groups after 6 months.
Statistical analysis
Data were analyzed by SPSS version 21 and the results were presented as mean±SD. To analyze the quantitative data independent sample T test was used. For the qualitative data we used chi-square test. A P value less than 0.05 was considered statistically significant.
Results
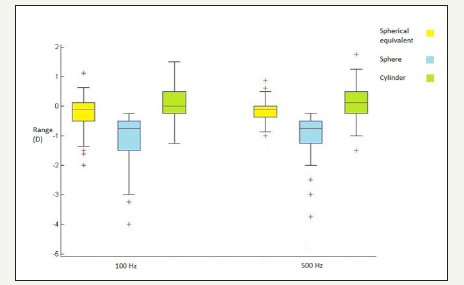
The study was performed on 110 patients, 37(33.63%) men and 73(66.37%) women. Mean age of the patients was 32.58±7.03 years (mean±SD) (range 22 to 45 years). The preoperative and postoperative sphere, cylinder and spherical equivalent refractive error are shown in Figure 1 & 2. The mean SE attempted correction was -3.68D±1.66 in 100Hz group and -3.80D±1.46 in 500Hz group. The results revealed that SE were significantly different pre and post-operation (P>0.001) but not between the groups (P=0.594). The mean spherical aberration (SA) was -0.166±0.164 μm (range -0.57 to 0.16μm) in the 100Hz group and -0.191±0.226μm (range -0.64 to 0.21μm) in the 500Hz group. SA was not significantly different between groups (P=0.433). The surgical induced astigmatism (SIA) and target induced astigmatism (TIA) were not significantly different between two groups (P=0.371 and P=0.118) and the abundance of these variables was in the range of 1.056±0.87D and 1.027±0.88D, respectively.
Figure 1:The preoperative sphere, cylinder and spherical equivalent refractive error.
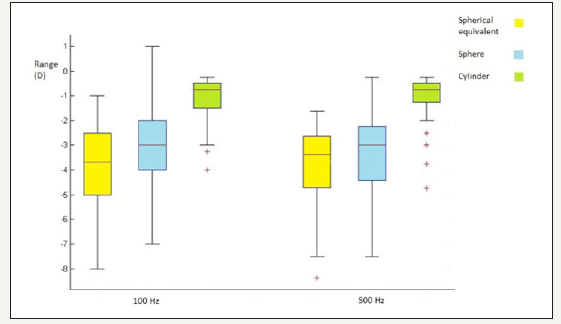
Figure 2:The postoperative sphere, cylinder and spherical equivalent refractive accuracy.
Visual outcomes
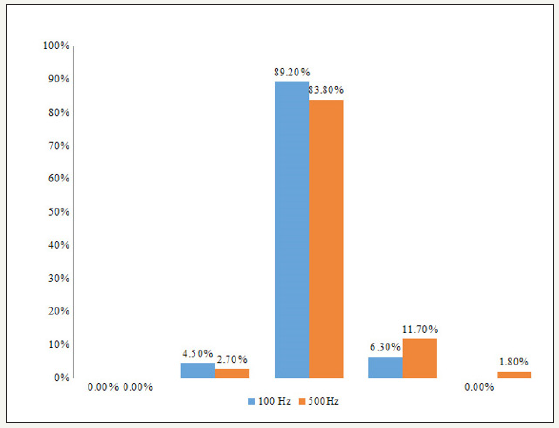
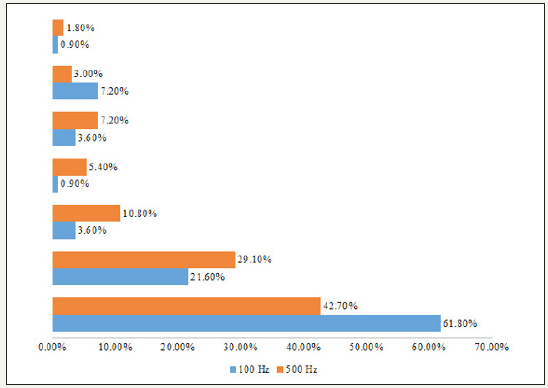
The mean UCDVA improved significantly in all eyes in both groups (preoperative, counting fingers to 8/20). Ninety-four eyes (85.45%) in the 100Hz group and 98 eyes (89.09%) in the 500Hz group had a UCDVA of 20/20 or better at the last followup examination. The BCDVA remained unchanged or improved in all eyes in both groups. In the 100Hz group, 98 eyes (89.09%) had unchanged BCDVA and 12 eyes gained 1 to 2 lines. In the 500Hz group, 103 eyes (93.63%) had unchanged BDCVA and 7 eyes gained 1 to 2 lines. Magnitude of error of astigmatic correction was not significantly different between the groups (P=0.22) and it was mainly in the range of -1 to 0.5D (Figure 3). The logMAR calculation showed no significant change in the UCDVA and BCDVA pre and post-operatively between both groups (P< 0.05).
Figure 3:The ranges of the absolute angle of error of astigmatic correction in both groups.
Astigmatic correction outcomes
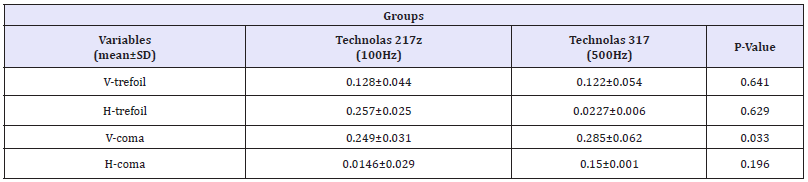
The predictability for both lasers were defined by the correction spherical equivalent at 6 months. The mean post-operation vertical trefoil in 100Hz group was 0.044±0.128 μm and in 500Hz group was 0.054±0.122μm. The mean of vertical coma, which was significantly different between groups (P-value=0.03), was 0.031±0.241μm and -0.062±0.285μm, respectively in groups 100Hz and 500Hz. The vertical trefoil, horizontal trefoil and horizontal coma were not significantly different between two groups as mentioned in Table 1. Figure 4 & 5 shows the postoperative corneal aberration between the ranges in group 100Hz and 500Hz respectively.
Figure 4:Postoperative corneal aberration in group 100Hz PRK (the reported number is the percentage of data between the ranges).
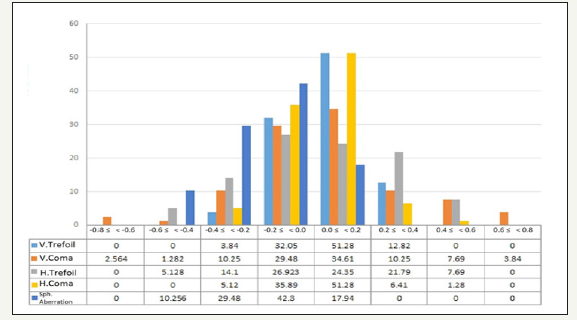
Figure 5:Postoperative corneal aberration in group 500Hz PRK (the reported number is the percentage of data between the ranges).
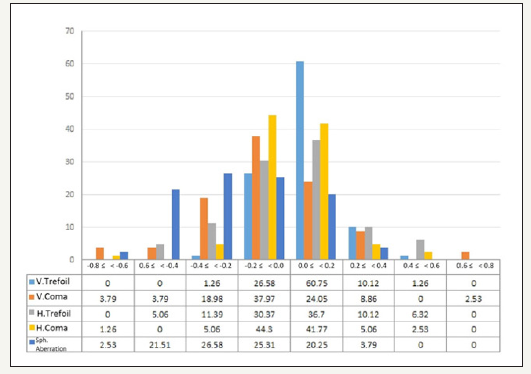
Table 1:Corneal wave front aberration parameters after photorefractive keratectomy in both groups.
The absolute angle of error was mainly in the range of 0 to 15 degree in both groups and there was no significant difference between two groups (P=0.076) (Figure 6). In addition, arithmetic angle of error was in the range of -10 to 15 degree in all eyes; as the same, there was no significant difference between two groups (P=0.56). There was no difference between using the 100Hz and 500Hz excimer laser because the index of success of astigmatism surgery was not significantly different between groups (P=0.136).
Figure 6:The magnitude of error of astigmatic correction of the 100Hz and 500Hz groups.
Discussion
The results showed both excimer laser systems were safe and effective in PRK surgeries. Also, the Technolas 217z100 system (100Hz repetition rate) have less mean of vertical coma in aberrometry. Refractive surgery using excimer lasers has been developed in order to achieve repeatable, safe, predictable and acceptable results. Newer laser platforms have been introduced over decades. Recent generation of excimer lasers acquire higher repetition rates, smaller laser spot size, and better delivery system [11]. Flying-spot technology has been introduced regarding avoid corneal thermal loading [12], however increasing the ablation rate over a threshold induces the probability of eliminating the advantage of flying-spot technology [11]. This study examined and compared the visual outcome and higher order aberrations (HOAs) after PRK surgery with 2 excimer lasers with different repetition rates. In one study by Fahim et al. [13] the preoperative UCDVA was count fingers, 1month and 3months after surgery, in all eyes, the mean UCDVA improved to 0.04±0.06 Log MAR (9/10) and 0.0±0.0 Log MAR (10/10), respectively. At 12 months after surgery, mean UCDVA had a significant increase, compared to preoperative UCDVA (P=0.010) [13-19]. In our study, pre and post-operative UCDVA significantly improved in both groups and there was no significant difference between the improvements of two groups. These results suggest that although the astigmatic change was slightly overcorrected in both groups, astigmatic correction was similarly effective in both groups. Our study found both repetition rates acceptable in efficacy, safety, and predictability. Our results were in line with previous research; most of these studies were done using different methods of excimer lasers and they did not compare the different repetition rates in PRK procedures [20-27]. Earlier generation excimer lasers were established for lower order aberrations, while HOAs were not considered [3,11,18]. In the current study, there were two eyes with high myopia, which were not significantly improved after PRK surgery. The number of the patients should be considered as a limitation in this study and we suggest larger sample size studies. However, some other studies reveal great results of PRK surgery for high myopia and HOAs [18].
From the previous studies we know the effect of excimer laser photo refractive surgery on increasing HOAs. The quality of optical performance of these corneas are low and less than acceptable rang. The induction of higher order aberrations (HOAs) is a problem that increases in relation to amount of correction after excimer laser procedures [19]. In a study Fahim et al. [13] assessed level of higher order aberrations root mean square (HOA RMS) before the surgery and 12months after the surgery. Preoperative and postoperative values of comma and trefoil showed no significant difference, but spherical aberration increased significantly 12months after surgery. In a study done by Michael Mrochen.et al the results showed that PRK-induced aberrations were significantly greater than the preoperative aberrations (a major increase in coma- and spherical- like aberrations) [7]. In a study authors demonstrated that, for spherocylindrical correction, 2mm or smaller beam is adequate (Zernike second order), but for correction of up to fourth order Zernike modes a 1mm or smaller beam is needed, and a 0.6mm or smaller beam is adequate for correction of up to sixth order Zernike modes [28]. The use of a smaller laser spots (Current scanning lasers with a beam diameter of 1mm or less) theoretically allows eliminating most of the higher order aberrations, which is important in custom corneal surgery [10,28]. Smaller laser spots will be able to create finer depth variation by producing proper ablation patterns [28]. However, using smaller spot size in ablation will increases surgical time, so performing excimer laser with higher repetition rate seems to be a logical solution to adjust the treatment time [10]. In this study we compared HOAs induced by these two types of excimer lasers and resulted in no statistically significant difference in RMS variables except for vertical-coma which was greater in 500HZ excimer laser group. However, SA was not significantly different between the groups.
Conclusion
Both excimer laser systems were effective, improving the UCDVA in comparison with the pre-operation UCDVA. Meanwhile, although the absolute and arithmetic angles of error were not significantly different in both groups, the results showed that Technolas 217z100 (100Hz repetition rate) in PRK surgeries might be more effective and efficient.
Ethical Standards
Ethical approval
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration.
References
- Nakamura K, Bissen MH, Toda I, Hori Y, Tsubota K (2001) Effect of laser in situ keratomileusis correction on contrast visual acuity. Journal of Cataract & Refractive Surgery 27(3): 357-361.
- Bansal A, Veenashree M (2001) Laser refractive surgery: technological advance and tissue. Bioscience Reports 21(4): 491-512.
- Von MCW, Khoramnia R, Lohmann CP (2009) Comparison of different excimer laser ablation frequencies (50, 200, and 500Hz). Graefe’s Archive for Clinical and Experimental Ophthalmology 247(11): 1539- 1545.
- Mrochen M, Schelling U, Wuellner C, Donitzky C (2009) Effect of time sequences in scanning algorithms on the surface temperature during corneal laser surgery with high-repetition-rate excimer laser. Journal Cataract & Refract Surg 35(4): 738-746.
- Mrochen M, Wuellner C, Rose K, Donitzky C (2009) Experimental setup to determine the pulse energies and radiant exposures for excimer lasers with repetition rates ranging from 100 to 1050Hz. Journal of Cataract & Refract Surg 35(10): 1806-1814.
- Fares U, Otri AM, Al Aqaba MA, Faraj L, Dua HS (2012) Wave frontoptimized excimer laser in situ keratomileusis for myopia and myopic astigmatism: refractive outcomes and corneal densitometry. Journal of Cataract & Refract Surg 38(12): 2131-2138.
- Mrochen M, Kaemmerer M, Mierdel P, Seiler T (2001) Increased higherorder optical aberrations after laser refractive surgery A problem of subclinical decentration. Journal of Cataract & Refract Surg 27(3): 362- 369.
- Mosquera SA, Sauer U, Brunsmann U (2012) In vivo measurements of thermal load during ablation in high-speed laser corneal refractive surgery. Journal of Refractive Surgery 28(1).
- Kitazawa Y, Tokoro T, Ito S, Ishii Y (1997) The efficacy of cooling on excimer laser photorefractive keratectomy in the rabbit eye. Survey of ophthalmology 42(1): S82-S88.
- Khoramnia R, Lohmann CP, Kobuch CA, Donitzky C, Von Mohrenfels CW (2010) Effect of 3 excimer laser ablation frequencies (200Hz,500Hz,1000Hz) on the cornea using a 1000Hz scanning-spot excimer laser. Journal of Cataract & Refract Surg 36(8): 1385-1391.
- Kymionis GD, Diakonis VF, Kounis G, Bouzoukis DI, Gkenos E, et al. (2008) Effect of excimer laser repetition rate on outcomes after photorefractive keratectomy. Journal of Cataract & Refractive Surgery 34(6): 916-919.
- Vetrugno M, Maino A, Valenzano E, Cardia L (2000) Corneal temperature changes during photorefractive keratectomy using the Laserscan 2000 flying spot laser. Journal of refractive surgery 17(4): 454-459.
- Fahim A, Rezvan B, Hashemi H (2013) Assessment of contrast sensitivity and aberrations after photorefractive keratectomy in patients with myopia greater than 5 diopters. Acta Medica Iranica 51(8): 520-524.
- Arbelaez MC, Vidal C, Mosquera S (2009) Excimer laser correction of moderate to high astigmatism with a non-wave front guided aberrationfree ablation profile: six-month results. Journal of Cataract & Refractive Surgery 35(10): 1789-1798.
- Stein HA, Salim AG, Stein RM, Cheskes A (1999) Corneal cooling and rehydration during photorefractive keratectomy to reduce postoperative corneal haze. Journal of Refractive Surgery 15: S232-S233.
- Kitazawa Y, Maekawa E, Sasaki S, Tokoro T, Mochizuki M, et al. (1999) Cooling effect on excimer laser photorefractive keratectomy. Journal of Cataract & Refractive Surgery 25(10): 1349-1355.
- Alpins N (2001) Astigmatism analysis by the alpins method. Journal of Cataract & Refractive Surgery 27(1): 31-49.
- Arora R, Goel Y, Goyal JL, Goyal G, Garg A, et al. (2014) Refractive outcome of wavefront guided laser in situ keratomileusis and wavefront guided photorefractive keratectomy in high pre-existing higher order aberration. Contact Lens and Anterior Eye 38(2): 127-133.
- Estrada A, Alió JL, Arba MS, Moreno LJ (2012) Corneal higher order aberrations after LASIK for high myopia with a fast repetition rate excimer laser, optimized ablation profile, and femtosecond laserassisted flap. Journal of Refractive Surg 28(10): 689-696.
- Ferreira TB, Marques EF, Rodrigues A, Montes MR (2013) Visual and optical outcomes of a diffractive multifocal toric intraocular lens. Journal of Cataract & Refractive Surgery 39(7): 1029-1035.
- Mojzis P, Piñero DP, Ctvrteckova V, Rydlova I (2013) Analysis of internal astigmatism and higher order aberrations in eyes implanted with a new diffractive multifocal toric intraocular lens. Graefe’s Archive for Clinical and Experimental Ophthalmology 251(1): 341-348.
- Alió JL, Piñero DP, Tomás J, Plaza AB (2011) Vector analysis of astigmatic changes after cataract surgery with implantation of a new toric multifocal intraocular lens. Journal of Cataract & Refractive Surgery 37(7): 1217-1229.
- Lane SS, Ernest P, Miller KM, Harris B, Waycaster CR (2009) Comparison of clinical and patient-reported outcomes with bilateral acrys of toric or spherical control intraocular lenses. Journal of Refractive Surgery 25(10): 899-901.
- Bauer NJ, Vries NE, Webers CA, Hendrikse F, Nuijts RM (2008) Astigmatism management in cataract surgery with the acrysof toric intraocular lens. Journal of Cataract & Refractive Surgery 34(9): 1483- 1488.
- Khokhar S, Lohiya P, Murugiesan V, Panda A (2006) Corneal astigmatism correction with opposite clear corneal incisions or single clear corneal incision: comparative analysis. Journal of Cataract & Refractive Surgery 32(9): 1432-1437.
- Qammar A, Mullaney P (2005) Paired opposite clear corneal incisions to correct pre-existing astigmatism in cataract patients. Journal of Cataract & Refractive Surgery 31(6): 1167-1170.
- Pop M, Payette Y, Amyot M (2001) Clear lens extraction with intraocular lens followed by photorefractive keratectomy or laser in situ keratomileusis. Ophthalmology 108(1): 104-111.
- Huang D, Arif M (2001) Spot size and quality of scanning laser correction of higher order wave front aberrations. Journal of Refractive Surgery 17: 588-591.
© 2018 Zeynab Raei. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






