- Submissions

Full Text
Medical & Surgical Ophthalmology Research
Diagnosing and Managing a Case with a Fourth Nerve Palsy and Papilledema
Andrea Fernández-Menéndez1 and Alfonso Casado2*
1Department of Pediatrics, Marqués de valdecilla Universitary Hospital, Spain
2Department of Ophthalmology, Marqués de Valdecilla Universitary Hospital, Spain
*Corresponding author: Alfonso Casado, Department of Ophthalmology, Marqués de Valdecilla Universitary Hospital, Spain. Email: casadorojo@hotmail.es
Submission: November 01, 2017; Published: February 23, 2018

ISSN: 2578-0360 Volume1 Issue4
Case Report
A 14-year-old boy presented to the Hospital with new-onset vertical binocular diplopia. Medical history was notable for a recent cranial traumatism. On examination, visual acuity was 20/20 in each eye. Pupils were equal and reactive. Visual fields (VF) were full to confrontation. A slight right head-tilt was observed (Figure 1A), as well as a left hypertropia of 3 Diopters (DP) in primary gaze. Ductions and versions revealed mild over-elevation in adduction and under-depression in adduction on the left eye. Left side Bielschowski maneuver was positive (Figure 1B). Red filter in right eye-test showed an oblique diplopia, but the patient had no torsion on Maddox testing. However, dilated fundus examination revealed bilateral fundus torsion and papilledema (Figure 2). Optical coherence tomography (OCT) revealed an abnormal thickness of the retinal nerve fiber layer (RNFL) and a normal values of retinal ganglion cells (GC).
Figure 1A & 1B.:
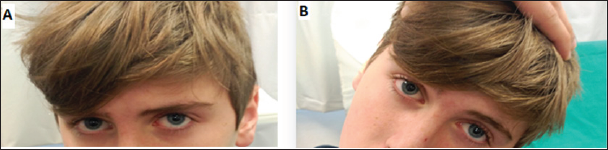
Figure 2:

The clinical diagnosis was left fourth (trochlear) nerve palsy with associated papilledema. Considering also the cranio-facial traumatism, urgent neuroimaging was recommended. X-ray computed tomography imaging of the brain revealed a broken arachnoid cyst in left temporal pole, with a partial collapse of the ipsilateral ventricle and deviation of 5 mm of the middle line. Steroid intravenous treatment was prescribed and no surgery was performed.
Figure 3:
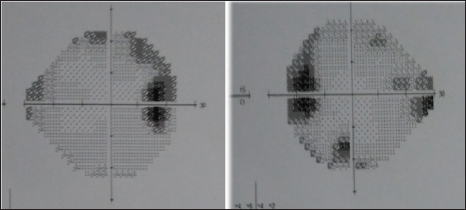
Figure 4:
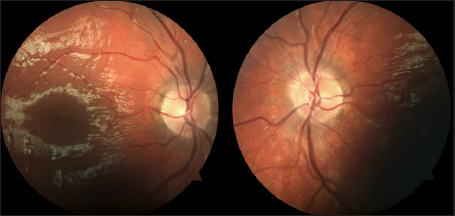
Four weeks later, torticollis and diplopia disappeared. However, the papilledema persisted and VF showed an increase in the blind spot (Figure 3). After 4 months of follow-up through periodic visits, monitoring with optical coherence tomography and retinographies, a marked decrease in papilledema was observed (Figure 4), and no damage of VF was depicted.
Discussion
The trochlear nerve has the longest intracranial course of all cranial nerves, so it is not surprising that its function could be affected by cranial traumatisms, and that could be related with papilledema [1]. It is mandatory the exploration with a neuroimaging test in the presence of any of these signs, and even more if both signs are presented together [1]. On the other side, most of the arachnoid cysts are asymptomatic [2]. In fact, only around 33% of those cysts underwent surgery, depending on their size [3]. Observation or steroid treatment is a common behavior in these cases [3].
Clinically, traumatic trochlear nerve palsy could solve also with observation. If diplopia or torticollis are annoying, unilateral shift occlusions during those symptoms could be a correct action, but if both diplopia or torticollis are significant, usually when Maddox testing reveals torsion, botulinum toxin injection in the ipsilateral inferior oblique could be performed [4].
Although the diagnosis of papilledema should be performed clinically with a retinal funduscopy, OCT could be useful in these cases. Firstly, it could serve to assess the progression of RNFL thickness increase. It is important, however, to correctly confirm the segmentation of RNFL, as with large thickness values of RNFL, OCT could make mistakes in segmentation. Secondly, retinal GC could be used to anticipate possible future damage of papilledema in VF, as it has been described in optic neuritis [5]. GC could be a powerful tool in cases of papilledema or pseudo papilledema, as OCT analysis reflects RNFL increase and could not reveal real damage of this layer that could be depicted with this analysis [6].
References
- Mollan SP, Edwards JH, Price A, Abbott J, Burdon MA (2009) Aetiology and outcomes of adult superior oblique palsies: a modern series. Eye (Lond) 23(3): 640-644.
- Eidlitz-Markus T, Zeharia A, Cohen YH, Konen O (2014) Characteristics and management of arachnoid cyst in the pediatric headache clinic setting. Headache 54(10): 1583-1590.
- Ali M, Bennardo M, Almenawer SA, Zagzoog N, Smith AA, et al. (2015) Exploring predictors of surgery and comparing operative treatment approaches for pediatric intracranial arachnoid cysts: a case series of 83 patients. J Neurosurg Pediatr 16: 275-282.
- Talebnejad MR, Tahamtan M, Nowroozzadeh MH (2015) Botulinum Toxin Injection for Treatment of Acute Traumatic Superior Oblique Muscle Palsy. J Ophthalmic Vis Res 10(3): 263-267.
- Rebolleda G, de Dompablo E, Munoz-Negrete FJ (2015) Ganglion cell layer analysis unmasks axonal loss in anterior optic neuritis. J Neuroophthalmol 35(2): 165-167.
- Casado A, Rebolleda G, Guerrero L, Leal M, Contreras I, et al. (2014) Measurement of retinal nerve fiber layer and macular ganglion cell-inner plexiform layer with spectral-domain optical coherence tomography in patients with optic nerve head drusen. Graefes Arch Clin Exp Ophthalmol 252(10): 1653-1660.
© 2018 Andrea Fernández-Menéndez, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






