- Submissions

Full Text
Medical & Surgical Ophthalmology Research
A Chronic Post Cataract Surgery Endophthalmitis with Suspended Intraocular Lens: A Case Report
Shuting, Liang Mingwu Li and Li Wenzhen Yu*
Department of Ophthalmology, Peking University People's Hospital, China
*Corresponding author: Li Wenzhen Yu, Department of Ophthalmology, Peking University People's Hospital, Beijing Key Laboratory of Diagnosis and Therapy of Retinal and Choroid Diseases, Beijing, China, Email: wenzhen_yu@sina.com
Submission: October 30, 2017; Published: December 14, 2017

ISSN: 2578-0360 Volume1 Issue1
Abstract
Purpose: Present a case of endophthalmitis that occurs after cataract surgery with suspended intraocular lens implantation.
Methods: Case report.
Results: Diagnosis of endophthalmitis caused by Staphylococci was confirmed by positive culture of aqueous humor. His visual outcome was satisfactory with good preserved vision.
Conclusion: Bacteria from conjunctival sac can invade into the eyeball through underlying tunnel of the suture knot, leading to endophthalmitis.
Introduction
Endophthalmitis is one of the most devastating complications of intraocular surgeries, leaving patients with permanently poor vision. Since cataract surgery consists of a large part of ophthalmic operations, the majority of literature reports about the endophthalmitis is focused on cataract surgery [1]. Chronic post cataract endophthalmitis generally caused by propionibacterium acnes, and this entity is an indolent form of endophthalmitis usually presented 6 weeks or more after cataract surgery [2]. We display a post traumatic cataract endophthalmitic case.
Case Report
A 45 year-old man presented to the emergency room (ER) of Peking University People's Hospital in June 2017, with sudden vision loss accompanied by severe pain and redness in his right eye for one day.
In 1999, the patient was hurt by an iron screw and had undergone suture of corneoscleral laceration in a local hospital. Several months after the first surgery, he was performed with traumatic cataract extraction and pars plana vitrectomy. In 2002, the patient came to the ophthalmology department, expecting to improve his right eye vision. In the absense of capsular/zoonular support, posterior chamber-intraocular lens (PC-IOL) was suspended with double-armed polypropylene, size 10-0 for sutured scleral fixation at ciliary sulcus by an experienced cataract surgeon. After the surgery, the BCVA of the affected eye improved from 0.01 to 0.6.
In 2009, the patient referred to the ER, complaining of blurred vision in his right eye for one day after being hurt by somebody's finger. Visual acuity of right eye at presentation was 0.02 and IOP was 12 mmHg. Slit-lamp examination revealed IOL was decenterd to the inferior and the superior optic edge remained above the central visual axis. Repositioning was performed with the remaining IOL and superior haptic was re-fixed at ciliary sulcus with poly propylene suture and the knot was buried in the lamellar scleral flap. The inferior knot was covered by the conjunctival flap.
Figure 1:
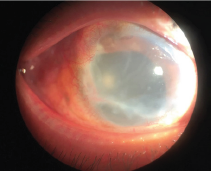
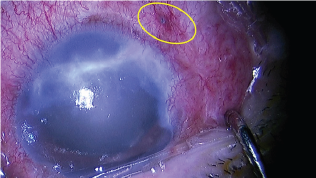
He was found to suffer from type 2 diabetes one year ago and did not use oral drug or insulin to control glucose. Fasting blood glucose reached 10mmol/L.At this time, the visual acuity was hand motions and intraocular pressure was 8 mmHg of the right eye. The visual acuity of the unaffected eye was 0.6 and IOP was 21mmHg. Slip-lamp examination revealed severe congestion in the right eye, with an infratemporal knot at a distence of 3 mm from the limbus, untransparent cornea with a scarring, numerous dust keratic precipitates (KPs), anterior cells 4+, aqueous flare (++), no obvious hypopyon and a PC-IOL. The fundus could not be visualized (Figure 1). B scan showed dispersed dot echoes throughout the vitreous cavity with low to medium reflectivity and a posterior-temporal band with high reflectivity (Figure 2). So, a diagnosis of endophthalmitis was presumed and aqueous humor (AH) samples were immediately obtained for pathogenic identification. At the same time, empirically vancomycin (2mg) combined with dexamethasone (0.4mg) was injected intravitreally and topical 0.5% levofloxacin eye drops 4 times one day were administered. AH smears were subjected to Gram's stain for detection of bacteria and showed Gram-possitive cocci.On the 2th day, the anterior and posterior inflammation was not improved. The conventional cultures characterized the bacterium as a staphylococcus epidermidis on the basis of colony morphology and convetional biochemical reactions. Meanwhile genechip arrays verified Staphylococci in aqueous humor at genetic level. Therefore, a complete pars plana vitrectomy combined with intraviteous injection of vancomycin (2mg) and ceftazidime (2mg) was performed. Massive white purulent clusters in the vitreous body and on the posterior retinal surface were found during the surgery (Figure 3). Neither retinal breaks nor retinal detachment were found after the purulent clusters had been completely removed. Unexpectedly, we found the infratemporal suture knot was loose which was used to fix the suspended IOL (Figure 4). Weak iodine solution was used to disinfect the knot and topical area after exposing tropical sclera. Foreign sclera was applied to cover the reinforced knot. Post-operative administration included intravenous ceftazidime 1000mg once a day for three days, topical 0.5% levofloxacin and 1% prednisolone acetate eye drops 4 times one day for two weeks. Medium intracameral inflammation was observed three days after the operation, and BCVA improved to 0.1. According to the drug sensitive test result, an intraviteous injection of vancomycin (2mg) was performed again. A relatively normal fundus with slight intracameral inflammation was observed two days after the injection, and the BCVA recovered to 0.15.
Figure 2:
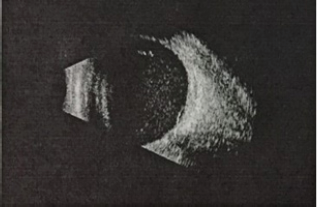
Figure 3:

Figure 4:
Discussion
In the absence of capsular support, the IOL could be implanted into the anterior chamber or sewn into the posterior chamber ciliary sulcus. PC-IOL implantation is a more optimal choice in eyes without capsular support, because of the long-term postoperative complications of anterior chamber IOL such as endothelial decompensation, secondary glaucoma and pupillary ectopia [3]. Gram-positive bacteria are the most common cause of postoperative endophthalmitis in the West [4]. Staphylococci was the most frequent bacterial flora isolated from conjuctival sac of patients prior to cataract surgery [5]. The conventional method is transscleral fixation of PC-IOL in the ciliary sulcus with a scleral flap. In this case, the patient underwent PC-IOL through pars plana fixation with inferior knot buried in the conjunctiva. After eigtht years, the knot was loose and exposed above the conjuctiva, and bacteria invaded into eyeball from the underlying tunnel of suture. Meanwhile, diabetes mellitus was proposed as patient-associated risk factor for the occurrence of endophthalmitis [6]. Intravitreal antibiotics, IOL extraction and vitrectomy are treatment options based on clinical course [7]. Above all, we prefer the knot beneath a scleral flap to burries in the conjunctiva when performing a suspended PC-IOL, because the knot is easier to expose without a scleral flap.
References
- Sandvig KU, Dannevig L (2003) Postoperative endophthalmitis: establishment and results of a national registry. Journal of cataract and refractive surgery 29(7): 1273-1280.
- Roussel TJ, Culbertson WW, Jaffe NS (1987) Chronic postoperative endophthalmitis associated with Propionibacterium acnes. Archives of ophthalmology 105(9): 1199-1201.
- Mandal AK, Bagga H (2002) Pupillary block glaucoma following implantation of a posterior chamber pseudophakos in the anterior chamber. Indian journal of ophthalmology 50(1): 54-56.
- Packer M, Chang DF, Dewey SH, Little BC, Mamalis N, et al. (2011) Prevention, diagnosis, and management of acute postoperative bacterial endophthalmitis. Journal of cataract and refractive surgery 37(9): 1699-1714.
- Suto C, Morinaga M, Yagi T, Tsuji C, Toshida H (2012) Conjunctival sac bacterial flora isolated prior to cataract surgery. Infect Drug Resistm 5: 37-41.
- Jabbarvand M, Hashemian H, Khodaparast M, Jouhari M, Tabatabaei A, et al. (2016) Endophthalmitis Occurring after Cataract Surgery: Outcomes of More Than 480 000 Cataract Surgeries, Epidemiologic Features, and Risk Factors. Ophthalmology 123(2): 295-301.
- Meisler DM, Mandelbaum S (1989)Propionibacterium-associated endophthalmitis after extracapsular cataract extraction. Review of reported cases. Ophthalmology 96(1): 54-61.
© 2017 Shuting, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






