- Submissions

Full Text
Modern Research in Dentistry
Fibula Free Vascular Flap and Endosseous Dental Implant for Reconstruction of Mandibular Defect after Surgical Resection of Ameloblastoma
Wael Ahmed Elmohandis1* and Samy Saeed Elnaas2*
1Professor and Head of Department of Oral and Maxillofacial Surgery, Egypt
1Lecturer of Department of Oral and Maxillofacial Surgery, Egypt
*Corresponding author: Wael Ahmed Elmohandis, Professor and Head of Department of Oral and Maxillofacial Surgery, Cairo, Egypt and Samy Saeed Elnaas, Lecturer of Department of Oral and Maxillofacial Surgery, Cairo, Egypt
Submission: September 16, 2021;Published: September 27, 2022

ISSN:2637-7764Volume7 Issue4
Abstract
Objectives: Reconstruction of mandibular defect after resection of ameloblastoma using free vascular
fibula flap and endosseous dental implants.
Surgical Procedure: Ameloblastoma was resected under general anesthesia with proper safety margins
and the mandibular defect was reconstructed immediately with vascularized free fibula flap connected
to surgical ped vessels. Pre-contoured reconstruction titanium plate was manipulated to fix proximal
and distal segment of the mandible together with the fibula flap. After healing phase, endosseous dental
implants were installed via transmucosal approach under local anesthesia.
Conclusion: Reconstruction of mandibular defects using free vascular fibula flap and endosseous
implant is considered as a valid and successful technique to obtain proper function and esthetics.
Moreover, it seems that using regular diameter dental implants in fibular bone is much more successful
than using wider diameter fixtures in stability and osseointegration.
Keywords: Ameloblastoma; Fibula flap; Endosseous implant
Introduction
Ameloblastoma is ‘a benign, but locally aggressive odontogenic tumor arising from the enamel organ of the dental tissue’. It is considered the second most common odontogenic tumor after the odontogenic keratocyst. It is most commonly found in the mandible (85%), maxilla (15%) and rarely other sites [1]. Generally, the diagnosis can be made by a combination of imaging plain radiographs, Computed Tomography (CT) scanning and biopsy. The mutlicystic/ solid type appears mostly as a multilocular radiolucency. Unicystic usually appears as a unilocular radiolucency. The denominator from other cystic lesions of the jaw is the expansion and destruction of cortical bony walls. Although initial biopsy helps to diagnose ameloblastoma, types and subtypes can only be diagnosed by histology examination of the entire specimen excised [2].
Ameloblastomas is characterized by a high rate of local recurrence. Because of this peculiarity, radical treatment is generally preferred than conservative surgery. Resection with free margins is associated with lower risk of recurrence but is not recurrence free; thus, the importance of long and scrupulous follow-up is evident [3].
After resection of the affected mandibular bony segment, a strong titanium reconstruction plate is fixed to the proximal and distal segments providing mono-maxillary and intermaxillary arch stabilization. In spite of the role of the reconstruction plate in rigid fixation and load bearing, loss of bony contact after tumor resection is considered as a weak point and a devastating drawback for prosthetic rehabilitation. Mandibular resection and reconstruction with autogenous bone is the most reliable treatment for mandibular tumors. In addition, surgeons generally prefer vascularized fibula flaps for the treatment of mandibular defects [4].
Precisely designed jaw reconstruction rehabilitation is important to the integrity of the structure of the jaw and is considered as a corner stone to preserve oral functions such as speech, mastication, and swallowing as well as facial esthetics and consequently social interactions [5]. Although fibula free tissue reconstruction alone can restore the natural arch of the mandible as well as restore a natural facial contour, patients are still left with a potential cosmetic and functional deficit. Primary and secondary dental implantation has been used for oral rehabilitation. This results in improved function by allowing the patient to masticate using an implant-supported fixed prosthesis. Patient aesthetics are also improved by providing lip support and aiding in oral competence [6].
Use of endosseous implants has modernized dental, oral, and facial rehabilitation because it provides a stable, reliable, and long-term option for reconstruction. Prosthetic rehabilitation of maxillofacial subunits using free tissue transfer and endosseous implants has been well described in the literature. The first reports of dental prosthetic rehabilitation of the mandible using free tissue transfer and endosseous implants dates back to 1989. Since then, this technique has been further refined, and nowadays dental prosthetic rehabilitation of large maxillofacial defects using free tissue transfer and endosseous implants is considered the standard of care [7].
Case Report
A 26-year-old Nigerian male patient with long-term expansion of the mandible was admitted to the Outpatient Clinic of Department of Oral and Maxillofacial Surgery, Faculty of Dental Medicine, Al Azhar University. He was diagnosed with the ameloblastoma in the mandible.
Stage I: Preoperative diagnosis and treatment plannin
Computed tomographic scanning was obtained from the patient to assess the extension of the osteolytic mandibular lesion and demonstrate its internal structure and peripheral behavior and relation with adjacent structures. Under local anesthesia, a mucoperiossteal flap was raised and reflected to expose the expanded buccal mandibular cortex. The cortex was drilled, and a punch biopsy was taken including the internal spongiosa and pathological intraosseous soft tissue. The biopsy was stored immediately in 10% formalin container and sent for histopathological examination. Histopathological examination has revealed a solid multilocular ameloblastoma with no malignant cellular deviation.
Stage II: Surgical procedure
The patient was hospitalized and routinely prepared for tumor resection. He was admitted at Maxillofacial Surgery ward, Sayed Galal University Hospital, Al Azhar University. For the real-time operation under general anesthesia, the surgeons were divided into two teams one to carry out the mandibular ameloblastoma resection and the other to harvest the fibula flap.
The mandible was approached through a submandibular incision and finished the mandibular resection with the help of our mandibular osteotomy guide to provide a safety surgical margin. The proximal and distal segments of the mandible were fixed to maxilla and an intraoperative intermaxillary fixation was achieved. The preformed reconstruction plate was fixed onto the remaining mandible with bicortical titanium screws supporting the two segments of the mandible into a whole while retaining a proper space for the fibular flap in between.
Meanwhile, the other surgical team cut the fibula using the fibular osteotomy guide plate. Lastly, the vascularized fibula flap was fixed to the mandible with the reconstruction plate to restore normal contour of the mandible. The contoured free fibula flap was fixed to the reconstruction plate with titanium screws maintaining contact with proximal and distal segments of the mandible. Both the arterial and venous vascular ped of the fibula flap were connected to the pre-clamped facial artery and common facial vein respectively to provide a competent blood supply to the free flap.
Vascular anastomosis was closely checked for patency, flow and absence of leakage. The wound was meticulously closed in layers providing a watertight seal suturing. The excisional biopsy was sent to histopathological examination and the patient was closely monitored after extubations for patent airway for 48 postsurgical hours. Antibiotics, analgesics, antiedematous medications were prescribed and local wound care was routinely maintained. Good fluid replacement is crucial for postoperative flap revascularization and viability.
Stage III: Endosseous implant installation
After six months, the vitality of the fibula flap was confirmed with ideal soft tissue healing over the flap and acceptable maxillomandibular relation with condylar range of movement. The patient was prepared for endosseous implant installation. Computed tomographic scanning was obtained to evaluate fibular bone quantity and quality and to determine implant number, locations and dimensions. Buccal and lingual local anesthetic infiltration technique was applied to obtain a profound anesthesia (Articain 4% with adrenalin 1: 100000).
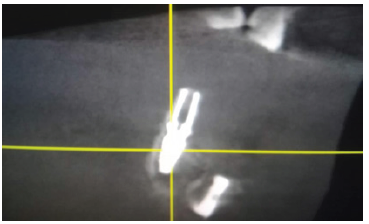
A flapless technique was followed with transmucosal drilling into the fibular bone under copious amount of saline irrigation. After pilot drilling, paralleling pins were inserted into the osteotomy hole and a periapical radiograph was taken to assess position, angulation and spacing. According to manufacturer instruction, sequential drilling was done to the predetermined length and diameter. It was predetermined to use a wider diameter implant in order to increase the Bone Implant Contact Area (BIC). The implant (Oxy Implant Dental System, Italy) was manually loaded into the osteotomy drill hole using a torque wrench. Cover screws were screwed into the implants platform and the patient was prescribed routine postsurgical medications (Figure 1-5).
Figure 1:Transmucosal drilling for dental implant in fibular bone.
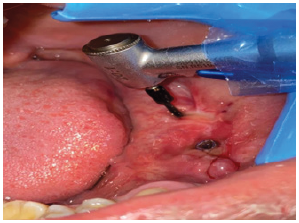
Figure 2: Drilling for dental implant in fibular bone through an open approach.
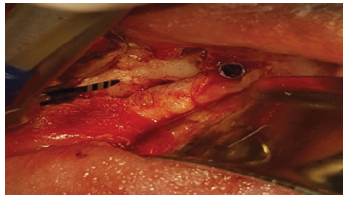
Figure 3: Osteotomy sites drilled in parallel direction for dental implants in fibula flap.

Figure 4: Panoramic view of dental implants installed into fibula flap.

Figure 5: Cross sectional cut of CT scanning of dental implant installed into fibula flap.
During follow up visits, unfortunately one of the implanted fixtures has developed localized infection. The infection was managed with local care and prescribing an empirical systemic antibiotic for 7 days until resolution has achieved. The implant osseointegration process was interrupted by infection and the offending implant was loosened and eventually removed. After one week, another visit was planned, and a regular diameter implant was inserted through a flap technique into a sound location of fibular bone. The regular diameter was preplanned in order to increase the thickness of both buccal and lingual cortices around the implant. It was hypothesized that the vascularity of fibular bone is much more different from native alveolar bone of the jaw. So, it was believed that leaving a thicker bone plate around the implant may favor a more optimal local vascularity for osseointegration of dental implants in the fibular bone.
Conclusion
Reconstruction of mandibular defects using free vascular fibula flap and endosseous implant is considered as a valid and successful technique to obtain proper function and esthetics. Moreover, it seems that using regular diameter dental implants in fibular bone is much more successful than using wider diameter fixtures in stability and osseointegration.
References
- Shi S, Liu Y, Shan Y, Fu T, Shan Y, et al. (2014) Enucleation combined with peripheral ostectomy: Its role in the management of large cystic ameloblastomas of the mandible. J Craniomaxillofac Surg 42(8): 1659-1663.
- Parmar S, Al-Qamachi L, Aga H (2016) Ameloblastomas of the mandible and maxilla. Curr Opin Otolaryngol Head Neck Surg 24(2): 148-154.
- Becelli R, Morello R, Renzi G, Matarazzo G, Dominici C (2011) Treatment of recurrent mandibular ameloblastoma with segmental resection and revascularized fibula free flap. J Craniofac Surg 22(3): 1163-1165.
- Yuan X, Xuan M, Tian W, Long J (2016) Application of digital surgical guides in mandibular resection and reconstruction with fibula flaps. Int J Oral Maxillofac Surg 45(11): 1406-1409.
- Chuka R, Abdullah W, Rieger J, Nayar S, Seikaly H, et al. (2017) Implant utilization and time to prosthetic rehabilitation in conventional and advanced fibular free flap reconstruction of the maxilla and mandible. Int J Prosthodont 30(3): 289-294.
- Jackson R, Price D, Arce K, Moore E (2016) Evaluation of clinical outcomes of osseointegrated dental implantation of fibula free flaps for mandibular reconstruction. JAMA Facial Plast Surg 18(3): 201-206.
- Patel S, Kim D, Ghali G (2019) Maxillofacial reconstruction using vascularized fibula free flaps and endosseous implants. Oral Maxillofac Surg Clin North Am 31(2): 259-284.
© 2022 Wael Ahmed Elmohandis. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






