- Submissions

Full Text
Modern Research in Dentistry
Geriatric Periodontal Disease (GPD): Will our Teeth Outlive the Aging Process? A Perspective
Eric Shapira DDS, MAGD, MA, MHA
Professor of Geriatric Medicine and Dentistry, USA
*Corresponding author: Eric Z Shapira, Professor of Geriatric Medicine and Dentistry,USA
Submission: August 08, 2022;Published: August 19, 2022

ISSN:2637-7764Volume7 Issue4
Abstract
Aging is a continuous process from birth until death. It is filled with many metabolic reactions that define the integrity of our Being over time. The human animal is a fragile entity, susceptible to harmful as well as what we think are normal bacteria that can become deleterious to our overall health throughout ones’ existence. In the formation of the human body, the periodontium is formed from primordial stem cells creating a supportive system of bone, ligaments, and several levels of gingiva; all of which support the subsequent onset of teeth. The aging process is fraught with catabolic activity, which can deteriorate healthy tissue in the body and mouth, jeopardizing the longevity of teeth. Systemic disease, long-term smoking, diabetes, dementias of different origins, lack of self-efficacy, poor oral healthcare habits and the aging process itself also accelerate the loss of teeth due to heightened disease states and can shorten ones’ lifespan as well.
This author is using the new term, Geriatric Periodontal Disease (GPD), as a combined system of chronic, aggressive, and disease-related periodontal disease, which in the presence of advanced age, creates a chronic intraoral disease state resulting in the diminishment of bone, increase in infection of the gingiva, as well as the degradation of the ligaments between the tooth structure and the remaining bone around the teeth. With the presence of such ‘catabolic’ activity surrounding one’s teeth in their elder years; a process occurs creating a nidus for eventual tooth loss as well as the possibility of intensified, already diagnosed, or clandestine systemic disease states.
Geriatric Periodontal Disease
According to a report by the Surgeon General in his Oral Health in America address; dental caries and periodontal disease are two of the most pandemic disease states known to mankind [1]. Geriatric periodontal disease is the presence of a chronic intraoral disease state affecting the bone, gingiva, and ligaments surrounding the teeth, which occurs more frequently during the elder years of a person’s life and is a nidus for eventual tooth loss, as well as the possibility of the presence of intensified systemic disease states. Cognitive, functional, and systemic medical conditions decline, coupled with a workforce decline with limited training to deal with these complex problems, can and will constitute primary challenges to providing oral health services for this cohort of individuals [2]. These disease states can be life threatening in these cases, which, in turn, can cause oral disease that is most destructive. Tooth loss was and is in many ethnic sectors of our Society an expected event. However, it is prudent for dental practitioners of all types to be on the look-out for oral disease states as well as systemic disease telltale’s in the oral cavity, and head and neck region as a sign of immediate action on their part’s; with the instigation of preventative techniques, such as diagnosis and education, to help promote improved self-efficacy among people who have less understanding about these entities than those persons who have learned what to do to maintain their overall health.
Being old does not necessarily mean that one will lose their teeth or even be subject to periodontal disease; however, it has been found that there is a correlation to aging and increased oral disease, such as periodontal disease, due to cognitive decline, for one, as well as lack of self-efficacy, low energy, mindset that dental care is not important, low dental IQ, lack of finances, lack of access to care, lack of transportation, inability to hold a toothbrush due to severe arthritic states or muscular degeneration leading to poor motor skills and the lack of resistance to chronic inflammatory diseases of the gingiva and surrounding bone. More recently, in a recent study published in the Journal of the American Medical Directors Association, found that dementia has been associated with the loss of teeth. Researchers found that those persons missing more teeth had, on average, a 48% higher cognitive impairment and a 28% higher risk of dementia than those who had their teeth [3].
Systemic Disease States Having an Effect on Periodontal Disease
A. Diabetes mellitus
B. Parkinson’s Disease
C. Dementia’s: (Alzheimer’s Disease, Vascular, Lewy-Body,
Frontal-Temporal Lobe, Mixed, Creutzfeldt-Jacob, Normal
Pressure Hydrocephalus, Huntington’s, Wernicke-Korsakoff
syndrome and Mild Cognitive Impairment)
D. Multiple Sclerosis
E. Rheumatoid Arthritis
F. Leukemia
G. Metabolic Disorders
H. Alcoholism
The Cause of Periodontal Disease
Periodontal disease is essentially instigated by plaque, or biofilm as it is now referred to: a potential formation of harmful bacteria. Periodontal disease seems to develop when there is an overabundance of bacteria in the mouth that changes the balance from harmless to harmful disease producing bacteria. These bacteria fulminate, develop into large colonies, become aggregated into sticky masses of cellular material coupled with food particles and other debris and are labeled as biofilm. Plaque can be subject to inorganic minerals found in the foods we eat and in our saliva. Calcium, for instance, secreted in saliva is a major ingredient in calculus. Where plaque is a ‘chemical’ irritant, calculus is a ‘physical’ irritant.
Research has shown us that plaque organisms can and do live under calculus and on top of it as well. Dental calculus, both supra- and subgingival types, occurs in most adults worldwide. Dental calculus is calcified dental plaque, composed of primarily calcium phosphate mineral salts deposited between and within viable microorganisms. A viable dental plaque covers mineralized calculus deposits; therefore, research by White and others suggests subgingival calculus may expand the radius of plaque induced periodontal injury [4]. There are two things now working against the normalcy of the gingiva: the harmful chemicals of the bacterial metabolic cycle and the physical irritation that the harder, fast growing calculus produces. Both processes cause an inflammatory response in the tissues of our mouths, with the creation of swollen gingiva, receding gingiva, various shades of gingival color: red, magenta, or blue indicating the chronicity and severity of the infection at hand, periodontal pocketing greater than 3mm and bleeding with accompanying discomfort at times. The process can be insidious without discomfort as well as symptoms of halitosis, suppuration, spontaneous bleeding, loose teeth, little to no discomfort and swelling of the gingiva around the teeth (Figure 1 & 2).
Figure 1: 73-year-old (Deceased) with Chronic GPD with associated risk factors and no discomfort.

Figure 2: A 70-year-old with GPD etiology including: Biofilm, Calculus, Stain, Mobility, Halitosis with no discomfort.

Risk Factors
Most Americans have some form of gum disease, but are
unaware that it exists; especially, not knowing what their respective
risk factors are in the first place. This state of unawareness is what
keeps people from going to the dentist and can be affected by
factors such as:
1. A low dental IQ
2. Family history
3. Lack of finances and discretionary income
4. Lack of access to care
5. Loss of transportation
6. No time
7. Aging and frailty
8. Fear and anxiety
9. Smoking or tobacco use in any form
10. Excessive use of alcohol
11. Poor nutrition
12. Hormonal changes, especially in women.
13. Chronic illness such as diabetes, HIV/AIDS, Hepatitis B and
C, and various arthritic conditions; COPD; chronic autoimmune
diseases
14. Side-effects of some medications
15. Genetic predisposition
16. Psychological disease and oral fixations
Inflammatory response to plaque and calculus produces HSCRP, or high sensitivity C-reactive protein as well as other forms of protein factors such as interleukin’s, Tissue Necrosis Factors (TNF) and cytokines, which are carried into the blood stream and help create inflammation, exacerbating both localized and systemic disease elsewhere in the body [5]. Recently, a blood test detecting C-reactive protein as a marker for inflammation within the body has been introduced as a clinical blood test. The dental practitioner should consider using this test when clinical signs and symptoms point to evidence of advanced periodontal disease in any form as there may be undetected systemic problems present [6].
Human Reaction
The psychological factors regarding tooth loss and periodontal disease are those that have not been looked at in depth. They seem to be a clandestine risk factor and nidus for oral disease and periodontal tooth loss. Older individuals who have some forms of cognitive decline are at risk for periodontal disease, especially if a direct caregiver or family member does not supervise their dental homecare. All too often memory loss can cause people to ignore their teeth. Some drugs taken by elder’s cause proliferation of gingiva, disabling people from really getting their teeth clean and some drugs create Xerostomia, with different degrees of dryness and saliva loss, which in turn creates increased sticky Biofilm, calculus build-up and an increase in inflammation and subsequent disease. Products such as: XyliMelts, ® OralBalance, ® Xerolube, ® to name a few, can mitigate the effects of xerostomia; keeping ones’ mouth lubricated and lessening the negative symptoms brought on by an increased accumulation of biofilm and disease-producing bacteria.
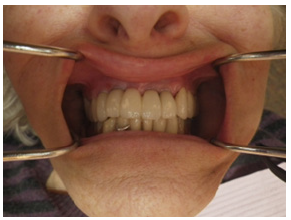
This author has a patient who is 86 years old and suffers from vascular dementia. She takes medication to enhance her memory or slow down its’ loss. Her medication also causes xerostomia. She has an early-onset GPD. Because of dementia she has regular teeth cleanings every two to three months. After lengthy discussion with her daughter, we decided to place implants in the maxillary anterior of her mouth with the hope that fixed prosthetics would help her sense of self, ease the loss she has been experiencing by the loss of her teeth and stay plate, maintaining her smile, as well as lessening the chances of continued decay (Figure 3 & 4). Risks of all kinds provoke a variety of human reaction. Since periodontal disease does not cause overt discomfort in most cases, many people are shocked to learn they have it. Periodontal disease may be multi-factorial. Factors such as “supervised neglect,” by both the patient and the dentist may be present. Other factors may be parafunctional habits, such as grinding or clenching ones’ teeth, genetic predisposition to having chronic periodontal disease and systemic disease that can cause xerostomia with subsequent increased colonization of bacteria in the mouth. Older people may have less resistance to infection due to their advancing age, diminished capacity to fight a variety of infections, diabetes, autoimmune diseases, chronic health problems, blood dyscrasias and the like. Human response to disease is as varied as the disease itself. No two people will react the same to disease.
Figure 3: 88-year-old (Now Deceased) patient with vascular dementia showing anterior implants.

Figure 4: Dementia patient with restored anterior implants with E-max crowns.
Dementia patients have earned the title, “silent sufferers” because most of the time, they cannot report accurately enough where they are having a problem, especially in the mouth. Because chronic advanced periodontal disease can be non-painful, having dementia as a disease entity only complicates both the finding of the disease, the treatment of the disease and the over-all diminishment of the disease to a healthy state. People, who become infirm in some way, who are compromised physically and cannot brush adequately, leaving them at risk for GPD.
According to an article written by Boehm and Scannapieco, “Periodontal disease is common in older adults. It may lead to root caries, impaired eating, and socialization. Treatment is not limited by chronological age but depends on the patient’s medical and emotional status and the availability of financial resources [7]. Increased risk of systemic disease such as diabetes mellitus, lung disease, heart disease and stroke may be apparent in those older persons with advanced periodontal disease that neglect themselves and do not treat the disease. Lack of socialization is a very difficult symptom of older age to diagnose and treat. It is the result of loss, grief, depression, anger, guilt, and sorrow; and in many cases changes in visual perception about the way one looks or feels.
This author had an 88-year-old widow for a patient who hardly left the house. She had large abfraction’s around her dental arches due to extensive bone loss and advanced geriatric periodontal disease, which had exposed her roots. Brushing with a hard brush had caused the great notches that greeted one when she smiled. Her periodontal disease was controlled to some extent. She never would allow me the opportunity to bleach or bond her teeth to make them more esthetic, leaving “notches” in her roots: a nidus for root caries. This denial about a potential problem probably was a direct effect of her depression and sadness, coupled with self-pity. She moved to an assisted-living facility, where she was forced to relate to others who lived there. After a while, she came back to this author’s practice and had her teeth bleached and bonded. Once this occurred, her symptoms of long-term depression, sadness and grieving almost disappeared overnight. Dentistry works in strange ways.
However, this woman was able to see the benefits and advantages of renewing her smile in a social setting and this may have been all she needed to come out of her long-standing “blue funk.” She had several good years in the assisted-living facility and then died of a massive heart attack. It is possible that the inflammatory by-products from her chronic GPD were contributory to her cardiac disease [8]. In reality, her teeth outlived the aging process (Figure 5A & B).
Figure 5A: Pre-treatment maxillary arch on an 88 yr. old woman (Pt now deceased)

Figure 5B: Post-treatment Maxillary arch on an 88 yr. old woman. Pt wanted to wait for the restorations on the mandibular arch, but passed away before she had the treatment done (Pt deceased)

Human Statistics about Longevity and Periodontal Disease
According to a study done in 2009 on the effects of human aging on periodontal disease, “Improvement in both social living conditions and health care has led to a greater life span for people across the globe, resulting in an increase in periodontal disease expectancy among the dentate elderly. Some loss of periodontal attachment and alveolar bone may be expected in older persons, but age alone in a healthy adult does not lead to a critical loss of periodontal support. Although moderate loss of both alveolar bone and periodontal attachment is common in elderly people, severe periodontitis-defined as attachment loss of 6 mm or more and radiographic bone loss of 50% or more involving at least one toothis not a natural consequence of aging [9].
According to Huhner and colleagues, it seems then that the greater the propensity for inflammation in the oral cavity, the greater the responsiveness of the periodontal ligamental cells in elderly patients to a degradation of extracellular matrix and to resorption of bone. Changes that are visible throughout the human aging process with respect to periodontal tissues are based on biomolecular changes of the cells of the periodontium that exacerbate bone loss in the elderly with chronic periodontitis. Inflammatory cells, such as cytokines, lead to a proliferation of osteoclastic activity. These cells, seen throughout the body, are also responsible for bone resorption in the mouth; but responsible for catabolic cell destruction in the body undergoing the aging process as well. Recent research has pointed out a deleterious biochemical relationship involving nitric oxide, a free radical capable of both helping to prevent inflammation in the mouth yet being implicated in the pathogenesis of over 100 conditions, including: rheumatoid arthritis, cancer, acute respiratory distress syndrome, AIDS, and periodontal disease [10]. Nitric Oxide can be stimulated by dental plaque and in turn becomes a messenger molecule in stimulating harmful chemicals that destroy the periodontium such as inflammatory cytokine’s, tissue necrosis factor, interleukins and other deleterious chemicals that break down the periodontium, according to the researchers who discovered this process, Simran and Raji kumar.
Statistics show an approximate increase of 58% in people over 65-years of age, to arthritic diseases; a staggering increase from 5 million persons now to 14 million people in the United States, a tripling effect, of Alzheimer’s Disease, a form of dementia, in the next five to six years; a 2-5% bone loss annually in people over the age of 65 years; and a very high incidence of stroke, heart disease and diabetes as well in people over 65- years of age [11].
We may be living longer but the statistics are against longevity to some degree. The risks are there. Periodontal disease, tooth loss and oral inflammation are prospects that will always be there as they are multi-factorial. There are many things that can contribute to tooth loss and disease in the mouth. It takes a great deal of selfefficacy to keep disease at-bay. The same is true for systemic disease and aging. The longer one lives, statistically he or she is subject to a lowered resistance to infection, an increase in susceptibility of disease that may be life-threatening, the possibility of tooth loss either through disease or by choice due to circumstances beyond ones’ control and the probability that at some point our elder’s may elect to do nothing to help themselves.
Poor nutrition may be a big part in the inflammatory process and GPD. The older one gets, the less likely they are to eat a totally healthy diet. With loss of income, older people tend to decrease spending on healthy food as they would on ‘cheaper’ food or fast food, which may not be all that nutritious. According to a recent literature search about nutrition, “the goal of nutritional support in periodontal disease should be to provide adequate energy and nutrients to meet the increased requirements for synthesis of acute phase proteins, inflammatory mediators, antioxidant defenses and the promotion of tissue repair and restoration of cellular function [12]. A healthy diet can and does lessen the effects of biofilm in the severity of periodontal disease. Nutritional deficiencies are known to reduce ones’ ability to provide a barrier to the inflammatory response, hence causing a reduction in the body’s’ defense system against infection. In effect, malnutrition can lead to an increased severity of oral infections leading to GPD. Oral health is central to nutrition and socialization, two of the hallmarks of successful aging. Untreated oral disease and loss of oral function can result in pain, difficulty chewing, swallowing, and eating, resulting in food avoidance and/or modification and eventually, nutritional inadequacy [13-16].
Clinical Examination and Evaluation
A clinical examination with subsequent evaluation should be done on all elderly patients on a routine basis. The heightened risk of systemic and oral disease in this cohort of people should stimulate the practitioners desire to have a ‘set’ protocol for this cohort. Should the older adult present with dementia, it will be necessary to have a designated family member or caregiver with them, with the Power of Attorney for Healthcare, who can answer specific health questions for the compromised patient. A systematic method of organizing the exam should begin with the written history, followed by an assessment of the patients’ cognition, and a full head and neck examination.
All too often, practitioners forget to get a medical approval for treatment and a copy of the written request. This documentation should be placed in the patient chart as well as the written response from the medical professional; indicating any contraindications to treatment based on medical findings. Alternate treatment plans should be presented to get to ‘yes,’ with respect to getting treatment needs met, and ultimately restoring dental and systemic health for the patient. Working as a team, referring to ancillary professionals who can enhance ones’ dental treatment is necessary and professional. Many practitioners may not be knowledgeable about the special needs of older, frail and medically challenged individuals. Therefore, it is incumbent upon the practitioner to learn what to look for in the process of an examination that will keep them comfortable, allow them to provide care in a foremo manner and be forward thinking when it comes to prevention; not just treating issues and neglecting the cause. It is also prudent for the dental practitioner to assess ones’ own ability to treat the older, more compromised individual.
Statement of Condition
Will our teeth outlast the aging process? If we deduce that those of us who practice self-efficacy in our younger years and continue throughout our lifetimes will keep our teeth; then our teeth will surely outlast the aging process. However, if we are subject to systemic diseases that take away our function of self-efficacy; causing an inability to perform the normal activities of daily living (ADL’s), then there is a good possibility that our teeth will not survive our lifetimes. The onset of geriatric periodontal disease GPD can be considered a result of functional loss.
It is incumbent upon all practitioners to be aware of the many co-factors that can cause diseases in the aging process. Coupling this awareness with the onset and recognition of the signs and symptoms of oral disease, such as those associated with the two pandemic diseases of periodontal disease and caries, will then allow an experienced professional to contribute to the prevention of tooth loss and perhaps the “early” loss of life.
References
- (2000) Report of the Surgeon General, Oral Health in America 2000, Speech by David Satcher MD, Surgeon General of the United States.
- Lamster IB, Kavita PA (2014) Oral health care affects quality of life. Today’s Geriatric Medicine 7(6): 22-26.
- Qi X, Zhu Z, Plassman BL, Wu B (2021) Dose-response metal analysis on tooth loss with the risk of cognitive impairment and dementia. Journal of the American Medical Directors Association 22(10): 2039-2045.
- White DJ (1997) Dental calculus: recent insights into occurrence, formation, prevention, removal and oral health effects of supra-gingival and sub-gingival deposits. Eur J Oral Sci 105(Pt2): 508-522.
- Hoefer IE, Steffens S, Ala-Korpela M, Back M, Berdimon L, et al. (2015) Novel Methodology for biomarker discovery in atherosclerosis. Eur Heart J 36(39): 2635-2642.
- Elgharib N, Chi DS, Younis W, Weltbe S, Keishnaswamy G (2003) C-reactive protein as a novel biomarker reactant can flag atherosclerosis and help predict cardiac events. Post Grad Med 114 (6): 39-44.
- Boehm TK, Scannapieco FA (2007) The epidemiology, consequences and management of periodontal disease in older adults. Am Dent Assoc 138 Suppl: 26S-33S.
- Beck J, Garcia R, Heiss G, Vokonos PS, Offenbacher S (1996) Periodontal disease and cardiovascular disease. Journal of Periodontology 67(10 Suppl): 1123-1137.
- Eder AH, Denise CM, Rogerio Belle, Andre Gustavo, Eduardo H, et al. (2009) Effects of human aging on periodontal tissues. Special Care Dentist 29(4): 149-155.
- Simran RP, Rajkumar NP (2015) Nitric oxide and inflammatory periodontal disease. General Dentistry 63(2): 34-40.
- (2012) Biological Resource of Animals and People.
- Kulkarni V, Bhatavadekar NB, Uttamani JR (2014) The effect of nutrition on periodontal disease: A systematic review. J Calif Dent Assoc 42(5): 302-311.
- Oral health for older Americans. Center for Disease Control and Prevention website
- Gil-Montoya JA, Subira CR, Gonzalez-Moles JM (2008) Oral health-related quality of life and nutritional status. J Public Health Dent 68(2): 88-93.
- Marshall S, Northridge ME, De La Cruz LD, Vaughab RD, O’Neil-Dunne, et al. (2009) ElderSmile: A comprehensive approach to improving oral health for seniors. Am J Public Health 99(4): 595-599.
- Marshall SE, Cheng B, Northridge ME, Kunzel C, Huang C, et al. (2013) Integrating oral and general health screening at senior centers for minority elders. Am J Public Health 103(6): 1022-1025.
© 2022 Eric Shapira DDS, MAGD, MA, MHA. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






