- Submissions

Full Text
Modern Research in Dentistry
Evaluation of treatment for Advanced Periodontitis affected with Molar Furcation Involvements and Secondary Occlusal Traumatism
Kuei-Lin Hou1,2* and Yi-Yuh Hong3
1Department of Periodontics, and Graduate Institute of Dental Science, Department of Periodontal Prosthesis, Kaohsiung Medical University, Taiwan
2Department of Periodontal & Prosthetic Therapeutic Center, Chang Gung Memorial Hospital, Taiwan
3Master Degree of Graduate Institute of Dental Science, Kaohsiung Medical Univer- sity, Taiwan
*Corresponding author: Kuei-Lin Hou, Department of Periodontics, and Graduate Institute of Dental Science, Department of Periodontal Prosthesis, Kaohsiung Medical University, Kaohsiung City, Taiwan
Submission: May 04, 2022;Published: May 20, 2022

ISSN:2637-7764Volume7 Issue2
Abstract
Objective: The purpose of this study was to evaluate the treatment of molar affected FI using combined
TPP, non-surgical RSR, and occlusal therapy may provide effective technique in treating SAP with molar
FI and SOT.
Background: It was thought that the cause of periodontal disease was related to the alignment of teeth.
In addition, uneven occlusal contact is associated with periodontitis, such as SOT, tooth mobility.
Methods: A total 50 molars which consisted of 17 molars without RSR are classified as the control group;
the other 33 molars with RSR and 25 units of TPP are classified as the experimental group (14.8±2.0
months; from 12 to 18 months). Both groups of patients were recorded periodontal parameters including
plaque index, gingival index, probing pocket depth, periodontal attachment level, tooth mobility, SOT.
Result: The results showed that the experimental group of molars affected FI had a significant
improvement in both tooth mobility and SOT, as compared to the control group. It can be seen that the
use of RSR combined TPP in SAP affected molar Classes II and III FIs to treat tooth mobility and SOT has
a remarkable effect.
Conclusion: We can conclude that the treatment of molar affected FI using combined TPP, non-surgical
RSR, and occlusal therapy may provide effective technique in treating SAP with molar FI and SOT.
Keywords: Furcation involvement; Root separation/resection; TPP; SOT; NSPT
Introduction
In the distribution of bite force, the molar region shares most of the bite force in the vertical direction; in the distribution of stress, the molar furcation position is the concentrated area of the bite force. When treating periodontal disease in the molar area, the consideration of occlusal, lateral and torque forces distribution should not be underestimated. It was once thought in the early stage that the cause of periodontal disease was related to the alignment of the maxillary and mandibular teeth, and uneven occlusal plane were also closely related to certain specific periodontal diseases such as SOT, tooth mobility. However, in the 1960s, after the “microorganism is the main cause of periodontal disease” was gradually established, although the bite was no longer considered the main cause of periodontal disease, its role was gradually regarded as a cofactor for the destruction of periodontal disease. The so-called cofactor means that this factor does not directly lead to the etiology of the disease but can change the order or presentation of the course of the disease [1].
Animal experiments by Glickman et al. [2] found evidence that occlusal factors are cofactors: in general, periodontal tissue inflammation is routed from the gingiva into the alveolar crest, but if periodontal inflammation is combined with secondary occlusal traumatism (SOT), the path of periodontal inflammation and destruction is not only towards the alveolar crest, also along the periodontal ligament. This is particularly pronounced on the pressure side of the tooth. A similar result was obtained from the observation of autopsies in cadavers [2]: excessive occlusal force, if the inflammation was confined to the periodontal ligament area, the occlusal injury can change the route of the reaction to spread around the periodontal bone. Later studies confirmed that occlusal injury can cause more severe periodontal attachment loss in periodontitis caused by microbial dental plaque, but as long as plaque control is done well and the distribution of its bite force is improved, its mobility degree and periodontal condition will gradually improve [3-8].
Material and Methods
Research sample collection
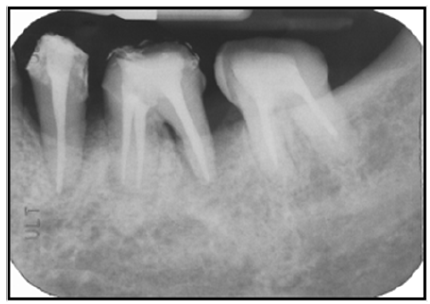
This study sample was taken from August 2001 to April 2003, and among patients who attended the Periodontology Department of the of Kaohsiung Medical University Hospital, after full-mouth periodontal parameter evaluation, according to the diagnostic method of our hospital, [9] patients with molars with class II and III FI (Figure 1) were diagnosed with teeth with root molar class II FI or above after the first stage of treatment of periodontal disease. Subjects are required to undergo a full-mouth periodontal examination and the collection of basic information includes plaque Index (PlI), gingival Index (GI), probing pocket depth (PPD), periodontal attachment level (PAL), classification of molar FI, SOT, tooth mobility [10], and full mouth periapical radiographs (Figure 1).
Control group (non-RSR): (Figure 1)
Patients are not willing to undergo root canal therapy and removable dentures but are willing to complete the first stage (Phase I periodontal therapy) of periodontal treatment (subgingival calculus scaling and root planning). Periodic three-month recall visits to receive professional plaque control (PLC), including meticulous subgingival scaling and planning on the teeth and molar root furcation areas as the control group. In addition, periodontal parameters included gingival index, plaque index, PPD, PAL, tooth mobility and injury of SOT (Figure 1) were measured at first month, third month, sixth month, and twelfth month.
Figure 1: Indicated that left mandibular first molar (# 36) affected Class III furcation involvement (FI) with secondary occlusal traumatism (SOT) and tooth mobility with non-RSR (The control group=non RSR).
Experimental group (RSR): (Figure 2)
Patients with class II to class III molar furcation invasion (FI)
selected by the above steps still have severe advanced class II FI
above the stage I treatment, that is, included in the parent group
of the sample. Subjects collected by the experimental group were
required to undergo:
A. The preparation of TPP.
B. For the treatment and refer to intentional root canal
therapy, if the tooth that has completed root canal therapy (RCT),
the density of filling, the completion time and the presence of
periapical lesion until the completion of treatment and then patient
was transferred back to the periodontal department for nonsurgical
RSR (Figure 2).
Figure 2: Demonstrated the non-surgical root separation (mesiobuccal and distobuccal roots) and palatal root resection (RSR) on the maxillary first molars (The experimental group= RSR).

Non-surgical root separation and/or recession (RSR) separates the severe affected classes II and III molar root furcation using a nonsurgical flap manner, using a high-speed bur to separate the root along the furcation and reshape the root with no residue undercut. If the partially supportive alveolar bone level of the root of the tooth has been destroyed more than 4/5, the root of the tooth is extracted and the other remained roots with adequate bone support are act as the abutments of the therapeutic provisional prosthesis (TPP). The plaque index (PlI), gingival index (GI), periodontal probing depth (PPD), periodontal attachment level (PAL), tooth mobility and SOT injury of residual abutments were recorded at the first month, the third month, the sixth month, and the twelfth month, respectively.
Tooth mobility
a) Intra-examiner: for the first examiner, the correlation
coefficient between the first measurement and the second
measurement is 1.0000(p<0.001); For the second examiner, the
correlation coefficient between the first measurement and the
second measurement is 1.0000 (p<0.001).
b) Inter-examiner: measurement accuracy (inter-examiner):
The correlation coefficient between the first examiner and the
second examiner’s measurement is 0.9388 (p<0.001); The
correlation coefficient between the first examiner and the
second examiner’s measurement was 0.9165 (p<0.001).
Result
The use of RSR combined with TPP in severe molar furcation involvement can be effective in improving the occlusal injury and is far superior to patients who only perform ultrasound scaling alone and regular plaque control. The baseline data of tooth mobility was 1.68±0.62, the first week was 1.250.59; in addition, there is remarkable decrease from 1.030.53, 0.690.71, 0.470.53 after the 3, 6, and 12 months decreased by 1.22 (0.67 (P<0.001). Therefore, before and after the phase I periodontal therapy, the change of tooth mobility in the experimental group (p<0.001) during the first year was significantly improved as compared to the control group (p>0.05). (Table 1).
Table 1: The comparison of the tooth mobility between the control and the experimental group (RSR) before and after therapy.
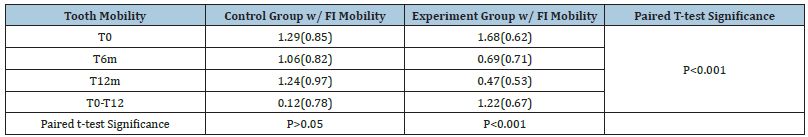
T0: baseline data; T6: 6 months later; T12: 12 months later; T0-T12: The data difference from T01 to T12.
The SOT injury in the molar roots before treatment and the postoperative first 1 week was 41.5% (27/65). In addition, molar roots had SOT injuries were 26.15% (17/65) and 7.7% (5/65) after 6 months and 12 months, respectively. And there was a significant difference in the before and after (Chi-square test) statistically significance in the experimental group (p<0.001) as compared to the control group (p>0.05) (Table 2). with SOT. From this point of view, it can be seen that in addition to proper oral hygiene training, periodic return diagnosis, combined with RSR and TPP, in addition to reducing mobility of the root, it can also effectively improve the situation of the molar root being injured by the SOT (Table 2).
Table 2: The comparison of the secondary occlusal traumatism (SOT) between the control and the experimental group before and after therapy.
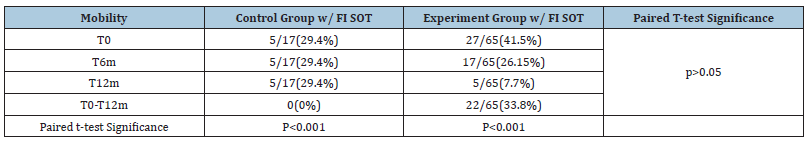
T0: baseline data; T6: 6 months later; T12: 12 months later; T0-T12: The data difference from T0-T12.
Discussion
In cases of individuals with SAP were most common affected by SOT. Once not only characterized by severely periodontal attachment loss and reduced height of the alveolar bone but frequently also of a remarkably increased mobility of teeth. SOT of the jigging type with concomitant increased hypermobility of teeth induced a series of periodontal tissue alterations associated with clinical and radiographic symptoms such as teeth hypermobility, pathological migration, angular bone defects, disappearance of lamina dura, widening of PDL. In order to present a gradual mechanical extraction of teeth with SAP, splinting using the periodontal prosthetic therapy for full mouth rehabilization should be carried out as a prevention of therapeutic purposes of masticatory function, the patient’s comfort, elimination of SOT, and esthetic dentistry.
Treatment of occlusal injuries in the treatment of periodontal disease, not only the morphology of the molar FI should be considered, but also when the lesion is SAP with SOT. When a healthy tooth is subjected to excessive bite force due to changes in the occlusal distribution, there is a clinical increase in mobility, improper displacement, and even a fremitus when the upper and lower bites are in contact. On the periapical radiographs, PDL widening is found, alveolar crest, and vertical bone loss. These are the characteristics of primary trauma from occlusion [11]. However, there is no increase in periodontal pockets and loss of periodontal attachments at this time. When the supporting tissue around the tooth is destroyed by a periodontal inflammatory response, the alveolar bone level reduces its ability to withstand the bite, and the periodontal tissue cannot bear the damage caused by the normal bite force, which is called the SOT [11].
In general, when severe advanced periodontitis (SAP) occurs in the molar area, the destruction of the alveolar bone in the molar furcation area of the molar is mostly more than one-half of the root (but it will vary according to the length of the root trunk), [12] and the tolerance of the affected tooth to normal occlusal force is greatly reduced. When performing the general occlusal function, even if the rate, occlusal force, frequency, and time are similar before, due to the decrease in adaptability, the tooth mobility degree gradually increases, the periodontal membrane widening and other secondary occlusal injury. If the inflammation of the molar furcation is combined, not only will the vertical alveolar bone be destroyed, but also the periodontal attachment will be lost [13,14]. The treatment at this time is not only to exclude the source of infection for the affected area to reduce the inflammatory response, but also to alleviate or eliminate the abutment teeth of SOT, which are called occlusal therapy.
Using primary or secondary splinting or with good complement design to eliminate abnormal occlusal force, lateral force and torque force, stabilize its functional occlusion, reduce tooth mobility and reduce patient discomfort, [15] is the treatment of teeth with SAP, especially for patients with molar FI, it is imperative. The more reliable treatment method for the serious invasion of the molar FI of the molar as mentioned in the first section is RSR, but at this time, if it is reshaped with a fixed cementum till necessary to face the problem that the molar furcation areas are controlled by professional and personal plaque. Therefore, how to apply the design of periodontal prosthesis to permanently resolve the problem of molar affected furcation involvement and prevent the problem of post-treatment complications is the main consideration in the treatment of periodontal disease.
A series reports of SAP affected molar with severe furcation involvement, SOT, and hypermobility of inadequate bony support in individuals were treated effectively and documented in recent literatures [16-21]. All the conclusions showed that the treatment for patients affected SAP with advanced molar FI, SOT, and grades II and III tooth mobility could be effective therapy under the combination of periodontal and prosthetic therapies included NSPT, TPP, RSR, fixed prosthesis and CSC telescopic denture.
References
- Gher ME (1998) Changing concepts. The effect of occlusion on periodontitis. Dent Clin North Am 42(2): 285-299.
- Glickman I, Smulow JB (1965) Effect of excessive occlusal forces upon the path- way of gingival inflammation in humans. J Periodontol 36: 141-147.
- Lindhe J, Svanberg G (1974) The influence of trauma from occlusion on progression of experimental periodontitis in the beagle dog. J Clin Periodontol 1(1): 3-14.
- Lindhe J, Ericsson I (1976) The influence of trauma from occlusion on reduced but healthy periodontal tissues in dogs. J Clin Periodontol 3(2): 110- 122.
- Lindhe J, Ericsson I (1982) The effect of elimination of jiggling forces on periodontally exposed teeth in the dog. J Periodontol 53(9): 562-567.
- Polson AM (1974a) Trauma and progression of marginal periodontitis in squirrel monkeys. II. Co-destructive factors of periodontitis and mechanically - produced injury. J Periodont Res 9(2): 108-113.
- Polson AM, Kennedy JE, Zander HA (1974b) Trauma and progression of marginal periodontitis in squirrel monkeys. I. Co-destructive factors of periodontitis and thermally-produced injury. J Periodont Res 9(2): 100-107.
- Polson AM, Metner SW, Zander HA (1976a) Trauma and progression of marginal periodontitis in squirrel monkeys. III. Adaptation of inter- proximal alveolar bone to repetitive injury. J Periodont Res 11(5): 287-289.
- Hou GL, Chen YM, Tsai CC, Weisgold AS (1998) A new classification of molar furcation involvement based on the root trunk and horizontal and vertical bone loss. Int J Periodont Res Dent 18(3): 257-265.
- Lindhe J (1989) Textbook of clinical periodontology. (2nd edn), Munksgaard, Copenhagen, Denmark, p. 317.
- Newman MG, Takei HH, Carranza FA (1996) J Clin Periodontol (8th edn), pp: 314- 315.
- Hou GL, Chen SF, Wu YM, Tsai CC (1994) The topography of the furcation entrence in Chinese molars. Furcation entrance dimensions. J Clin Periodontol 21(7): 451-456.
- Ramfjord SP, Ash MM Jr (1981) Significance of occlusion in the etiology and treatment of early, moderate, and advanced periodontitis. J Periodontol 52(9): 511-517.
- Zinner ID, Panno FV, Landa LS (1989) Provisional prosthodontic appliances in the combination fixed-removable reconstruction. Dent Clin North Am 33(3): 379-397.
- Bernal G, Carvajal JC, Muňoz CA (2002) A review of the clinical management of mobile teeth. J Contemporary Dental Practice 3(4): 1-11.
- Hou GL (2020) A non-surgical root separation and/or resection for the treatment of advanced furcation involved molars- A longitudinal study for 5-18.5 years. J Dent & Oral Disorder 6(1): 1151.
- Hou GL (2021a) Difference of annual radiographic alveolar bone loss rates of anterior and posterior teeth of individuals affected with secondary occlusal traumatism between with and with without perioprosthetic therapy. Advances in Dent & Oral Health 14(4): 1- 6.
- Hou GL (2021b) A long-term evaluation of bone levels using digital scanning radiographic image analysis on the CSC telescopic abutments in severe advanced periodontitis affected secondary occlusal traumatism. Advances in Dent & Oral Health 14(5): 1- 6.
- Hou GL (2021c) A long-term study of oral rehabilitation for the treatment of severe advanced periodontitis with secondary occlusal traumatism using intentional replantation, fixed prosthesis and perioprosthetic design of CSCTD. Advances in Dent & Oral Health 14(5): 1- 6.
- Hou GL (2021d) A dynamic technique of oral rehabilization using fixed prosthesis and CSC telescopic denture for severe advanced periodontitis with secondary occlusal traumatism-A long-term case report. European J Dent and Oral Health 2(6): 1- 4.
- Hou GL (2022) Oral rehabilitation of case affected severe advanced periodontitis with furcation involvement and secondary occlusal traumatism. Advances in Dent & Oral Health 15(3): 1- 7.
© 2022 Kuei-Lin Hou. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






