- Submissions

Full Text
Modern Research in Dentistry
First Clinical Experience with the ICX-Active Master Implant System: A 3-year Retrospective Study
Patrik Prachar1*, Ivan Tresnak2* and Sonia Bartakova1
1Assistant professor, Masaryk University, Faculty of Medicine, Brno, Czech Republic Dental clinic, St. Anne´s University Hospital, Brno, Czech Republic
2Private practise, Sand in Taufers, Italy
*Corresponding author: Patrik Prachar, Assistant professor, Masaryk University, Faculty of Medicine, Brno, Czech Republic Dental clinic, St. Anne´s University Hospital, Brno, Czech Republic
Submission: March 10, 2022;Published: March 31, 2022

ISSN:2637-7764Volume7 Issue2
Abstract
Aim:. The aim of this retrospective study was to report on the clinical experience with the ICX-Active
Master implant system. The design of the implant corresponds to modern findings in the modelling of
final elements. It corresponds to minimum bone stress in close connection with the implant.
Materials and Methods: This study retrospectively evaluated clinical data from patients treated with the
ICX-Active Master implant system. Patients received at least on implant in the maxilla or mandible and
were used ICX-Active Master, ICX-Narrow and ICX-Active White implants. The implant primarily suits the
indications of immediate implantation and immediate load in a manner similar to that during use in cases
with bone availability of poorer quality and quantity.
Result: The authors evaluated experience with 500 implants inserted at 4 different sites in an age range
from 18 to 82 years. 286 implants were inserted in 125 men, and 214 implants in 105 women. Implants
were used in all bone qualities (D1-D4). The diameters of the implants were 3,3mm, 3,75mm, 4.1mm and
4.8mm with length of 10mm, 12.5mm and 15mm. The evaluation period is currently two years with 100
% success rate.
Conclusion: In spite of its use not only in conventional indications, but also in immediate and delayed
indications, including immediate loading, the Active Master has become a safe and suitable alternative in
the field of implantology.
Keywords: Concept active; Osseointegration, Immediate implantation, Implant freezing
Introduction
ICX-Active Master implant constitutes a consequent expansion of the ICX system portfolio from Medentis. This implant represents a fundamental simplification of the concept of immediate implantation, i.e., implantation which follows immediately after a tooth is extracted or lost due to injury. Immediate implantation also remains the first indication for this type of implant. Another strong point is the use of implants in bones which are compressed in terms of quality and availability. The unusually high primary stability (strength) of the implant frequently also allows its immediate loading. In addition to the standard diameters 3.75-4.1- 4.8mm and lengths of implants 8-10-12.5-15mm, ICX-Active-Master Narrow implants are available with a diameter of 3.3mm. These come in three lengths 8-10-12.5mm. Whereas in view of the prosthetic supra-structure standard active implants are compatible with the ICX Premium system, Narrow active implants have a prosthetic range completely of their own. Ceramic implants (zirconium oxide, ZrO2/Y-TZP) with diameter of 4,1mm and lengths 8-10- 12.5mm constitute a separate range of active implants [1,2]. The long-term success of loaded implants depends on many factors.
These are derived for one thing from the individual clinical situation of the patient and also to a significant extent from the quality and special properties of the individual components of the implantology system. One of the important factors are the modalities of the edge surface for the implant surfaces. The physical-chemical and morphological properties of the implant surface are also important. In general, it applies that the structuring of a surface or its working leads to an acceleration of the early healing processes and thus an increase in the quality of the healing process along with increase in the quality of direct contact between the implant and bone [3,4]. For a specific and verified ICX implant surface this involves a mechanical and thermochemical modification of this surface. A roughening and subsequent increase of this surface is achieved through this process. In the first step the surface is blast abraded with titanium corundum. In the next step the implant surface is exposed to the action of a strong acid in a special thermochemical process [3]. It has been generally demonstrated that compared with other implant surfaces of the same geometry surfaces treated in this way display the fundamental advantage of this combination of treatment compared with other surface treatments of implants. This process creates a three-dimensional microstructured surface representing the ideal physical, chemical and biological conditions for addition and growth (firstly addition) of the relevant cells responsible for the formation of new bone. This encourages and positively influences the formation of new bone. The join between the bone and implant surface is stable, and the healing time is reduced. ICX implants are subject to strict quality control. The implant’s surface topography and roughness are checked. Implants are subject to strict quality control using a scanning electron microscope. They must display very strict chemical purity during this check.
And this is verified regularly at two mutually independent facilities in Germany. There is also a quantitative analysis of the surface using optical profilometry (NanoFokus). As part of quality control there are also regular tests with cell cultures to ascertain the quality of the impact of the implant’s material at the cellular level in the immediate surroundings. In general terms four mutually linked properties of the implants’ surface were shown to have a direct impact on bone cells: chemical composition, energy, roughness and morphology of the surface. It was seen that the fixing and colonisation of the surface, and the consequent division and differentiation of these cells is influenced and modified by one or a combination of the aforementioned factors. The study of these processes results in a continuous improvement of the surface properties, such as hydrophilia or initial fixing of osteoblasts [5,6]. Another advantage of the ICX Active system is that if the surgical protocol is introduced and adhered to, there is no so-called “freezing” of the implant. Another important feature in this is the thread, which allows the implant to be moved back whilst adhering to the protocol. This range of implants has been created not only due to the great pressure on implantology for early and delayed solutions, but also with the possibility of conventional placement after sufficient healing of the bone.
Materials and Methods
Characteristics of system
The ICX-Active implant system has several characteristic
elements
A. Bevelled edge of implant, which should result in lower
stress in the area of the cortical bone and thus prevent and reduce
resorption in this most important area of the implant
B. Aggressive thread for perfect primary stability,
which is absolutely fundamental primarily for immediate and
delayed implantation. This thread utilises a self-tapping double
compression thread, and in spite of its “aggression” is very simple
during placement - it guides the operator very precisely in the
implantation osteotomy.
C. Type of thread: self-tapping double thread allows faster
yet more sparing insertion of the implant
D. Combination of compressive and progressive type of
thread. Whereas the angle of the compressive thread increases
the stability of a conical implant through compression of bone
particles, the self-tapping progressive thread on the apex of the
implant’s conical body allows subsequent fixing of the implant
often in residual bone beyond the peak (end?) of the extraction
socket. The progressive thread offers a significant increase in the
contact surface of the implant with the surrounding bone in the
aforementioned apical area with non-compressed bone.
E. Verified structured surface with hydrophilic properties
allowing faster, quality healing of implant
F. All ICX implants are made of pure grade 4 titanium.
G. Abutment, its internal part complies with compatibility
with the premium range without use of other components. The
Narrow range constitutes an exception. The actual abutment
combined with the implant has an anti-rotation element (hexagon)
allowing the insertion and anchoring of the crown in a clearly given
position. A self-locking angle is also used, which is significant in that
it prevents the penetration of bacteria and so increases resilience
against (one of the causes of) peri-implantitis.
The surgical protocol is a highly precise instruction for the insertion of an implant. It corresponds with the specifics of bone density, where it uses individual drills marked with either one, two or three bands. These
bands are a guide for the given bone density. This may seem pointless until the transplant dentist really feels differences in bone density. Another important thing is that the threads allow compression-increase in bone density. A screw-tap for densities 1 and 2 is essential. Another important element is that during the insertion of a dental implant we must not exceed 35Nm so that we can still manipulate the implant and so that we do not create a so-called frozen implant which is typical for some implantation systems. So, during manipulation we are capable of manipulating the implant up to a range of 20-25Nm of torque. Not adhering to these conditions leads to destruction of the implant insertion tool, which is dimensioned in such a way as not to destroy the antirotation elements of the implant when the torque limit is exceeded. The surgical protocol is different for immediate implants, where the procedure tends to be reduced by one or two steps back with regard to the seat following extraction preserving commensurate primary retention. It is similar for delayed implantation.
We talk of so-called under-preparation, where drills are used for a diameter smaller than the installed implant. Naturally for the healing of the implant we need at least 0.5mm of embedding under the corticalis, which goes hand in hand with the thicknesshorizontal of the alveolus. Here the rule applies that if we get to a 1mm minimum bone thickness around the implant fixture, we try to drill up to 1-1,5mm deeper, because this corresponds to resorption, which is physiological with a smaller availability of bone in the area around the implant. It is possible to introduce the fixture with the aid of a mechanical device or manually with precise setting of torque. Manual insertion is a natural advantage for all implants. The actual implantation appears simple, but we might change the direction of insertion compared with the original pilot hole during installation, so an experienced implant dentist is required. But the strength (stability) of implant does not change with this shift in direction thanks to the type of threads. Naturally the system uses both analogous and navigated implantation.
Result
Table 1: Statistic data of inserted implants over a period of three years.
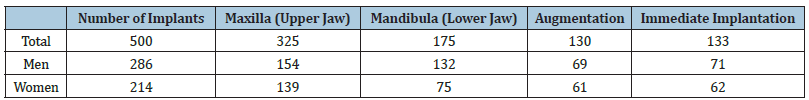
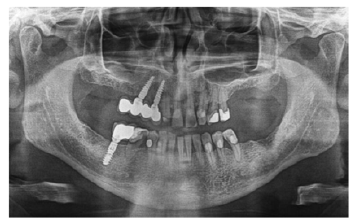
Figure 1: Delayed implantation for lateral incisorsubcrestal implantation.

Figure 2:Implantation jointly with bilateral sinus augmentation.

Over a period of three years the authors inserted 500 implants in 230 patients ranging from 18 to 82 years old. There were 286 implants in 125 men, and 214 implants in 105 women. Implants were used in indicative bone qualities from D1 to D4 in diameters 3.3mm, 3.75 mm, 4.1mm and 4.8mm in lengths of 10mm, 12.5mm and 15mm. The largest number of implants (nearly one third) were implanted in the gap after the loss of one tooth. Implants were used in indications solo abutment, shortened dental arch, joint of implants in fixed work in edentulous jaws and use of implants in edentulous jaws with hybrid transfer attachments. Implants were used for solo abutments in the main in indications of immediate or delayed implantation. The indication areas include sinus augmentation (sinus lift) in a single phase with implantation. Statistically speaking no implant was rejected (Table 1). In the case of an implant talk of prosthetic flexibility, which includes interchangeability of suprastructures between the Active system and Premium (conventional) system. Also, adaptation to the required direction in spite of other preparation osteotomy and finally use of screwable and cemented work, moreover with hybrid transfer (Figure 1-4).
Figure 3:Ceramic implant from in situ after insertion.

Discussion
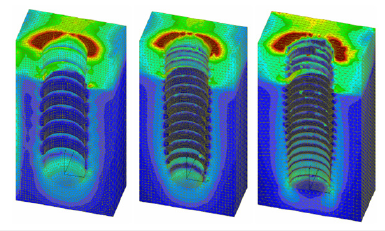
The system ICX Active Master is a system range belonging to the implant range ICX. One of the ranges is “Premium” with use of micro threads, which from the aspect of stress in the corticalis area is also one of the advantages for reducing this stress. There is a possibility here to compare with the Nobel Active or Astra system, which has similar parameters of design, implantation and use [7-11]. Only the financial aspect, including other instruments, is currently reducing the sales potential of this system on the market. One can also make a comparison with Neodent Drive, originally from Brazil and since 2015 under the name Straumann [12,13]. This system is financially comparable with the ICX system, primarily in the single set of instruments for the entire Neodent range. The only issue here is that it is not possible to use it in bone density 1 and in part also 2 because there are no thread taps for such use. This series is exclusively for the upper jaw, and here there is little danger of the implant “freezing” after insertion. Much depends on the experience of the implant dentist, and he then has no such problem. In general terms one can say that the system ICX Active is a range of implants using elements of micro-threads - ICX Premium, and slim implants Slim Boy for the given slim type of alveolus, and it also uses anchoring of supra-structures without threads, which is a highly advantageous element against peri-implantitis. The ICX system uses anti- rotational elements and elements of a self-locking angle in connection of the supra-structure, which reduces or prevents bacteria colonisation and thus peri-implantitis [14,15]. The systems Ankylos, Astra Tech have similar elements. And this self-locking angle allows the transmission of pressure over a greater area than only over the thread of the superstructure. This is important for the strength of the join without possibility of damage or breaking. At present there exists several materials for implantation, which include conventional titanium, alloys of titanium combined with zirconium-titanium, beta-titanium alloys and finally ceramic implants [16-23]. Everything undergoes biological testing and mechanical- physical tests so that the strictest parameters for the biocompatibility of material used in bone are met. The use of supra structures most often embedded in the fixture of the implant is also associated with this. Here there is a preference for fixing using antirotation elements and very often a self-locking angle to prevent bacterial colonisation in the cortical layer [24-26]. During the development of implants the first actual design analysis currently is by the end elements method. This does not involve just the design of the implant, but simulation of environment in which the implant is inserted [27-30] (Figure 5).
Figure 4: Active Master implants 1,5 years after implantation.
Here the most important part of the implant is in the cortical layer of the bone, and so here a reduction in the bone- implant stress is of primary importance in order that there should be no unwanted resorption of bone at the point of the implant neck. In general terms according to the modelling of final elements, i.e., study of stress in area of entire implant, a slope towards the right-angle termination of the implant in the head part (face) turns out to be the best. It also applies that a narrowing of the implant face in terms of the fixing part of the implant, which is thus wider, is important for reducing pressure in the corticalis area and thus preventing resorption processes [31,32]. Naturally we must take into account the fact that simulation helps when creating an implant of the most ideal design, but the bone as a living organ may react differently than it did during the simulation. This corresponds, for example, to the angle of the implant, the diameter of the implant and the stress of the thus embedded implants at a certain angle. This is evident in the lower bi-foraminal jaw, where implants with a smaller diameter do not have such resorption as during simulations using the end elements method.
Figure 5: Illustration of modelling of final elements with use of various types of threads
Conclusion
ICX Active Master is a modern, flexible system covering an entire range of indications, from conventional implantation right up to immediate implantation, including immediate loading of implant. Thanks to the surgical protocol the implantation is very simple, with a certain level of attention necessary during the actual insertion, where the implant may change the direction of insertion away from the prepared bed for the implant. The threads of this implant allow significant bone compression and thus an increase in bone density during insertion. Ceramic single-phase implants are also part of the Active system portfolio.
During clinical use this system had a 100 % success rate in statistical evaluation over a short tree-year period. The ICX implant surface is distinguished by optimal and reproducible surface topography. Pre- clinical and clinical data from the literature show that the combination of blast abrasion and etching of the surface, as is the case for the ICX system, displays excellent osseointegration properties. If we add to this the system’s many positive clinical factors, the ICX system represents a safe and verified alternative for the implanting doctor.
References
- Fandkidejski R (2019) Ceramic competence. Dental Magazin 37(6): 26-27.
- Von Sterberg N (2019) An implant for all bone qualities. Z Oral Implant 35(9): 126-128.
- Buser D, Broggini N, Wieland M, Schenk RK, Denzer AJ, et al. (2004) Enhanced bone apposition to a chemically modified SLA titanium surface. J Dent Res 83(7): 529-533.
- Buser D, Nydegger T, Oxland T, Cochran DL, Schenk RK, et al (1999) Interface shear strength of titanium implants with a sanblasted and acid-etched surface: a biomechanical study in the maxilla of miniature pigs. J Biomed Mater Res 45(2): 75-83.
- Andreiotelli M, Wenz HJ, Kohal RJ (2009) Are ceramic implants a viable alternative to titanium implants? A systematic literature review. Clin Oral Implants Res 20(Suppl 4): 32-47.
- Schwarz F, Wieland M, Schwartz Z, Zhao G, Rupp F, et al. (2009) Potential of chemically modified hydrophilic surface characteristics to support tissue integration of titanium dental implants. Journal of Biomedical Materials Research Part B: Applied Biomaterials 88(2): 544-557.
- Aspriello SD, Rasicci P, Ciolino F (2011) Immediate loading of Nobel Active implants in postmenopausal osteoporotic women: 2-years follow up study. Clin Oral Implants Res 22: 222.
- Babbush CA, Brokloff J (2012) A single-center retrospective analysis of 1001 consecutively placed Nobel Active implants. Implant Dent 21(1): 28-35.
- Irinakis T, Wiebe C (2009) Clinical evaluation of the Nobel Active implant system; a case series of 107 consecutively placed implants and a review of the implant features. J Oral Implantol 35(6): 283-288.
- Kolinski ML, Cherry JE, McAllister BS, Parrish KD, Pumphrey DW, et al. (2014) Evaluation of a variable-thread tapered implant in extraction sites with immediate temporization: A3-year multi-center clinical study. J Periodontol 85(3): 386-394.
- Yamada J, Kori H, Tsukiyama Y, Matsushita Y, Kamo M, et al. (2015) Immediate loading of complete-arch fixed prostheses for edentulous maxillae after flapless guided implant placement: a1-year prospective clinical study. Int J Oral Maxillofac Implants 30(1): 184-193.
- Martin C, Thomé G, Melo AC, Fontão FN (2015) Peri-implant bone response following immediate implants placed in the esthetic zone and with immediate provisionalization-a case series study. Oral Maxillofac Surg 19(2): 157-163.
- Sartori IAM, Latenek RT, Budel LA, Thomé G, Bernardes SR, et al. (2014) Retrospective analysis of 2,244 implants and the importance of follow-up in implantology. Journal of Research in Dentistry 2(6): 555-564.
- Schweikert MT, Botticelli D, Sbricoli L, Antunes A, Favero V, et al. (2015) Sequential healing at implants with different configuration and modified surfaces: An experimental study in the Dog. Clinical Implant Dentistry and Related Research 18(3): 438-448.
- Rustamova EK (2018) Optimization of adaptation to orthopedic construction in patients support into dental implants by occlusion kappa. Russian newsletter of dental implantology 1-2(39-40): 55-59.
- Hollander DA, Von Walter M, Wirtz T, Sellei R, Rohlfing BS, et al. (2006) Structural, mechanical and in vitro characterization of individually structured Ti-6Al-4V produced by direct laser forming. Biomaterials 27(7): 955-963.
- Fukuda A, Takemoto M, Saito T, Fujibayashia S, Neo M, et al. (2011) Bone bonding bioactivity of Ti metal and Ti-Zr-Nb-Ta alloys with Ca ions incorporated on their surfaces by simple chemical and heat treatments. Acta Biomaterialia 7(3): 1379-1386.
- Hanawa T (1991) Titanium and its oxide film: a substrate for formation of apatite. In: Davies JE (Ed.), The Bone-Biomaterial Interface, University of Toronto Press, Toronto, Canada, pp: 49-61.
- Hansson S, Werke M (2003) The implant thread as a retention element in cortical bone: the effect of thread size and thread profile: a finite element study. J Biomech 36(9): 1247-1258.
- Josset Y, Oum’Hamed Z, Zarrinpour A, Lorenzato M, Adnet JJ, et al. (1999) In vitro reactions of human osteoblasts in culture with zirconia and alumina ceramics. Journal of Biomedical Materials Research 47(4): 481-493.
- Shimakura M (2007) Efficient polishing method of titanium. J Soc Titanium Alloys in Dentistry 5: 32-33.
- Wang BL, Li L, Zheng YF (2010) In vitro cytotoxicity and hemocompatibility studies of Ti-Nb, Ti-Nb- Zr and Ti-Nb-Hf biomedical shape memory alloys. Biomed Mater 5(4): 044102.
- Zhao SF, Jiang QH, Peel S, Wang XX, He FM (2013) Effects of magnesium-substituted nanohydroxyapatite coating on implant osseointegration. Clinical Oral Implants Research 24(Suppl A 100): 34-41.
- Norton M (1997) An in vitro evaluation of the strength of an internal conical interface compared to a butt joint interface in implant design. Clin Oral Impl Res 8(4): 290-298.
- Romanos GE, Nentwig GH (2009) Immediate functional loading in the maxilla using implants with platform switching: five-year results. Int J Oral Maxillofac Implants 24(6): 1106-1112.
- Silvennoinen R, Vetterl V, Hasoň S, Tuononen H, Silvennoinen M, et al. (2008) Sensing of human plasma fibrinogen on polished, chemically etched and carbon treated titanium surfaces by diffractive optical element-based sensor. Optics Express 16(14): 10130-10140.
- Reddy MS, Sundram R, Abdemagyd HAE (2019) Application of finite element model in implant dentistry: A systematic review. HAE Journal of Pharmacy and Bioallied Sciences 11(Suppl 2): S85-S91.
- Nakamura K, Tajima K, Chen KK, Nagamatsu Y, Kakigawa H, et al. (2013) Dental application of novel finite element analysis software for three-dimensional finite element modeling of a dentulous mandible from its computed tomography images. Proc Inst Mech Eng H 227(12): 1312-1318.
- Shi ML, Li HY; Liu XM (2017) Multidisciplinary design optimization of dental implant based on finite element method and surrogate models Journal of Mechanical Science and Technology 31(10): 5067-5073.
- Yamaguchi S, Yamanishi Y, Machado LS, Matsumoto S, Tovar N, et al. (2018) In vitro fatigue tests and in silico finite element analysis of dental implants with different fixture/abutment joint types using computer-aided design models. J Prosthondont Res 62(1): 24-30.
- Abraham JA, Grenón MS, Sánchez HJ, Pérez CA, Valentinuzzi MC (2002) Titanium based implants, metal release study in the oral environment LNLS 2006 Activity Report Geurtsen W. Biocompatibility of dental alloys. Crit Rev Oral Biol Med 13(1): 71-84.
- Albrektsson T, Zarb G, Worthington P, Ericsson AR (1986) The long-term efficacy of currently used dental implants. A review and proposed criteria of success. Int J Oral Maxillofac Implants 1(1): 11-25.
© 2022 Patrik Prachar. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






