- Submissions

Full Text
Modern Research in Dentistry
Case Report-Soft Tissue Healing in Exposed Bone Grafted Socket Using Laser-Assisted Blood Coagulation: 14 Year Review
LUK Kenneth*
Private practitioner, Laserdontic, 502 Winway Building, Hong Kong
*Corresponding author: LUK Kenneth, Private practitioner, Laserdontic, 502 Winway Building, 50 Wellington Street, Central, Hong Kong
Submission: February 15, 2022;Published: March 29, 2022

ISSN:2637-7764Volume7 Issue2
Abstract
A 37-year-old male patient presented with pain and ulceration at the corner of the mouth. Bone graft was exposed in the socket three days after surgery. Materials and methods: An 810nm laser with selected parameters and technique was used to relieve pain at the angle of the mouth. Laser-assisted blood coagulation technique (LBC) was used to promote soft tissue healing over the socket using 810nm and Erbium YAG (Er:YAG) lasers. Results: Immediate pain relief was achieved after laser irradiation. Soft tissue coverage was established in three days. On re-entry after six months, bone regeneration was successful in the socket. Thirteen-year review after implant placement showed good bone quality. Bone level at the implant was comparable to initial placement.
Introduction
Bone grafts are commonly used in socket preservation immediately after extraction. Primary closure of the socket ensures good bone regeneration in the socket. Primary soft tissue closure failure may affect the quality or cause bone regeneration to fail. A 37-year-old male patient presented with pain and ulceration at the left corner of his mouth. Mouth opening range was limited due to pain. Patient was placed under intravenous sedation for extraction and immediate placement of an implant at Tooth 36. However, implant placement was not possible, and a bone graft was placed. The covering over the socket was dislodged three days after surgery. The patient was a healthy non-smoker and not under long term medication.
Investigation
Some ulceration at the left angle of mouth was caused by operative trauma (Figure 1). Mouth opening range was painful and limited. A wound without sutures with bone graft material was exposed in the socket (Figure 2). Periapical radiograph showed complete removal of the molar tooth with bone graft filled in the root spaces (Figure 3).
Figure 1: Ulceration at left angle of mouth.

Figure 2: Exposed bone grafted socket.

Figure 3:Pre-op radiograph.
Objectives and rationale for using lasers
The objective was to re-establish primary closure by flap surgery under local anaesthesia. Mouth opening posed a problem to operate, and the patient rejected this recommendation.
.Pain relief at corner of the mouth
Photobiomodulation (PBM) is a non-thermal photochemical interaction between cells and light / laser in the red and near infrared electromagnetic spectrum. The effect of PBM on tissue on modulating the host’s inflammatory response has been well documented [1]. The pro-inflammatory factors (chemical mediators) such as TNF𝛼 (pain related) and INF𝛾 can be decreased using PBM. 810nm diode laser wavelength was selected for pain relief in this case. Although the parameters described here were above the PBM energy level, the high intensity laser therapy can also achieve similar results with much shorter irradiation time [2,3].
Bone graft decontamination
Although our search on bone graft decontamination using Er: YAG laser was not found, Kreisler et al [4] concluded that at low energy densities, Er: YAG laser has a bactericidal effect on implant surfaces. At 0.1J/cm2 energy density, Er: YAG laser can dissociate water molecules into singlet oxygen and OH radicals which are highly toxic to bacteria. Er: YAG laser was also shown to be effective in biofilm reduction on titanium surfaces [5].
Re-establishing blood clot to promote soft tissue healing
An in vitro study showed that laser irradiation stimulates fibroblast proliferation [6]. Soft tissue proliferation at an exposed bony site has previously been achieved in two days using laser assisted blood coagulation (LBC) [7].
Materials and Methods
The laser parameters and procedures did not necessitate the use of local anaesthetic.
Pain relief and improving mouth opening
810nm diode laser was the chosen wavelength. The parameters were set at 20W, 15kHz, 10𝜇s using non-initiated 600𝜇m fiber. The fibre was moving at a distance from the ulcerated site defocusing the beam between 1 and 2cm spot size. Irradiation was stopped when patient felt warmth. The site was allowed to cool, and the patient reported pain relief effect compared to initial pain. This step was repeated a number of times. Total irradiation time was 16 seconds.
Bone graft decontamination
The top layer of the graft material was excavated followed by decontamination of the existing bone graft with a 2940nm Er: YAG laser. The parameters were set at 100𝜇s, 70mJ, 20Hz at an average power of 1.4W. The irradiation technique was carried out using a 400𝜇m tapered sapphire tip in a scanning motion with water spray. The area was irradiated a few times in different directions and at different angles to ensure complete irradiation coverage of the surface.
Re-establishing blood clot to promote soft tissue healing
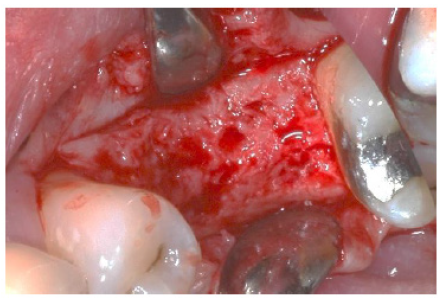
Using the above parameters and techniques, the soft tissue in and around the socket was ablated and de-epithelialized, and bleeding was induced by Er: YAG laser. An 810nm diode laser was used for coagulation & stabilization of the blood clot. Parameters were set at 20W, 20kHz, 16𝜇s. A 600𝜇m non-initiated fiber was placed at a distance of 2mm from the bleeding socket. Fixed spot irradiation for about 0.5 s produced a color change of the clot from red to pink. The technique was repeated to cover the full area. Some over-irradiated areas showed a blackened in color (Figure 4).
Figure 4: Coagulated socket by LBC technique.

Post-operative management
The patient was instructed NOT to disturb the clot with brushing, toothpaste or antiseptic mouthwash. A warm gentle saline mouth rinse was recommended. A healthy diet without spicy foods was advised. Antibiotics and analgesics were not prescribed.
Result and Discussion
Pain relief at corner of the mouth
The patient’s self-reported pain level decreased from 10 before irradiation to 2 after repeated irradiation. Mouth opening was normal, and some discomfort on full mouth opening was acceptable. Although the output power was 20W, average power was 3W. The pulse energy was 0.2mJ with energy density of the defocused beam ranging from 0.157 and 0.64mJ/cm2. Therefore, the high frequency was set at 15kHz, which is warranted to yield an average power of 3W.
Re-establishing blood clot to promote soft tissue healing
The patient was reviewed after three days. The bone graft in the socket was covered with fibrin. There was bleeding on probing into the fibrin layer indicating vascular supply over the bone graft (Figure 5). Re-epithelialization across the centre of the socket buccal lingually took place on Day 17 (Figure 6). During Week 6, complete keratinization over the socket was observed (Figure 7). Peri-apical radiograph (Figure 8) and re-entry at 6 months post-op showed successful bone regeneration (Figure 9).
Figure 5:3 days post-op.

Figure 6: 17 days post-op.

Figure 7: 6 week post-op.

Figure 8: 6 months post-op radiograph.
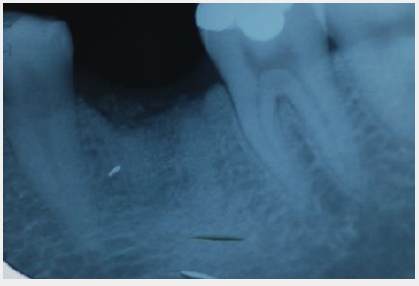
Figure 9: Re-entry at 6 months post-op.
Er: YAG laser is absorbed well by water. Although its average power is 1.4W, the output power is calculated to be 700W. A short pulse duration with water spray allowed soft tissue ablation with low thermal conduction. The outcome effect was bleeding. If Er: YAG laser was not available, scalpel would be required to induce bleeding under local or topical anaesthesia.
810nm wavelength is absorbed well by melanin and haemoglobin. A 30W, 16𝜇s, 20kHz setting have been shown to produce a subsurface coagulation effect in non-ablative gingival depigmentation [8,9]. As irradiation was directly onto the blood clot, the same parameters with lower output power at 20W was selected. The settings generate a 0.32 mJ pulse energy with a 10 mJ/ cm2 energy density. With a 0.5 s fixed spot irradiation dosage of 100 J/cm2, an immediate surface coagulation effect was achieved. LBC coagulation provided a gelatin-like surface layer of clot. The black area of the clot showed carbonization in a thin hard layer. However, the black material can be peeled off easily, leaving the gelatinous layer below. Nevertheless, the carbonised layer provided additional protection to the clot. Laser coagulated surface is more stable than a natural formed clot.
The conventional method to re-establish primary closure by flap surgery is widely accepted. To leave the grafted site to heal would be an alternative. The advantage of LBC technique allows for soft tissue proliferation within a few days protecting the graft. This is a minimal invasive with minimal discomfort technique. There was no need for anaesthesia or medication. In cases of primary closure difficulty by flap surgery, combining LBC may assist the clinical outcome. In this case report, the patient was very pleased with the immediate ulcer pain relief and improvement in mouth opening restrictions. Patient was more confident to continue implant surgery after trouble free socket healing.
Implant placement and reviews
Implant surgery was performed on the day of re-entry. Figure 10 shows a periapical radiograph of pre-impression coping fit for a screw type crown. Ten-year review showed healthy soft tissue margin around the implant (Figure 11). Periapical radiograph at 13- year review showed good bone quality and bone level comparable to initial placement (Figure 12).
Figure 10: Radiograph at impression coping.

Figure 11: Implant/Tissue margin at 10 years review.
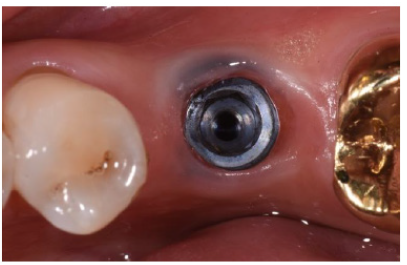
Figure 12: 13 years post-implant radiograph.

Conclusion
The laser-assisted blood coagulation technique was effective for promoting soft tissue healing on exposed bone grafted socket. It provided a good soft tissue seal for bone regeneration. LBC may be an alternative option or assistance to primary closure by flap surgery. More clinical cases are required to verify the reproducibility of this technique.
References
- Romagnoli E, Cafaro A (2017) PBM-theoretical and applied concepts of adjunctive use of LLLT/PBM within clinical dentistry. Lasers in Dentistry Current Concepts pp: 131-160.
- Kingsley JD, Demchak T, Mathis R (2014) Low-level laser therapy as a treatment for chronic pain. Front Physiol 5: 306.
- Chow R, Armati P, Laakso EL, Bjordal JM, Baxter GD (2011) Inhibitory effects of laser irradiation on peripheral mammalian nerves and relevance to analgesic effects: a systematic review. Photomed Laser Surg 29(6): 365-381.
- Kreisler M, Kohnen W, Marinello C, Götz H, Duschner H, et al. (2002) Bactericidal effect of the Er: YAG laser on dental implant surfaces: an in vitro J Periodontol 73(11): 1292-1298.
- Polak D, Shani Kdoshim S, Alias M, Shapira L, Stabholz A (2022) The in vitro efficacy of biofilm removal from titanium surfaces using Er:YAG laser: Comparison of treatment protocols and ablation parameters. J Periodontol 93(1): 100-109.
- Pereira AN, Eduardo CP, Matson E, Margues MM (2002) Effect of low-power laser irradiation on cell growth and procollagen synthesis of culture fibroblasts. Lasers Surg Med 31(4): 263-267.
- Luk K (2009) A novel technique of laser-assisted blood coagulation for tissue regeneration in implant dentistry. International Magazine of Laser Dentistry 1(3): 21.
- Luk K (2005) Clinical application of a digital pulsed diode laser in depigmentation therapy. Journal of Academy of Laser Dentistry 13(4): 18-21.
- Luk K (2009) Depigmentation of gingivae and lip with Digital Pulsed Diode Laser-an integral part of Cosmetic Dentistry. International Magazine of Laser Dentistry 1(2): 31-33.
© 2022 LUK Kenneth. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






