- Submissions

Full Text
Modern Research in Dentistry
Posterior Root-End Resection with Palatal Approach
Juan G Robledo*, Karina I Krasnopolski and Pablo A Rodríguez
School of Dentistry, University of Buenos Aires, Argentina
*Corresponding author: Juan G Robledo, School of Dentistry, University of Buenos Aires, Argentina
Submission: December 20, 2021;Published: January 13, 2022

ISSN:2637-7764Volume7 Issue1
Abstract
Root-end resection is a reliable option for retention of valuable teeth with strategic function. However, when treatment is required on the posterior region, variations in regional and radicular anatomy should be rigorously considered. The aim of this case report is to show the apical root-resection procedure on a palatal root of first maxillary molar with palatal approach.
Introduction
Root-end resection has been defined as “The surgical removal of the apical portion
of a root and adherent soft tissues” [1] thus, is a reliable method of treatment for peri
radicular disease. However, if surgery is indicated in the posterior region, some drawbacks
such as limited access, visibility and anatomical structures induce decision to extraction or
intentional replantation of the tooth. On the palatal side, anatomic considerations should
be evaluated such as root shape, curvatures, location of foramina, fused roots, fenestrations
and even possibility of molars with double palatal root [2,3].
The greater palatine neurovascular bundle (GPB) can be damaged during osteotomy,
root resection or even if a posterior relieving incision is used. Bleeding or paresthesia
could be the result if those anatomical structures are injured. Cone Beam Computer
Tomography (CBCT) is useful for a clinician to anticipate those anatomical conditions and
project designs of surgical flap and osteotomy [4].
The height of palatal vault generally influences surgical procedures for palatal
approach. If its high, the access to the palatal root apices is more predictable. The palatal
root in maxillary molars (generally oval in shape) has a buccal curvature in the apical
third, prevention of root perforations or ledges should be carefully considered during nonsurgical
root canal treatment.
Thickness of palatal masticatory mucosa is also important, a computerized tomography
(CT) study revealed that males have thicker mucosa and thickness increase with age,
probably due to increment in fat tissue and gingival recession. The thinnest mucosa was
found in first molar area [5]. Palate is covered with masticatory mucosa, which is fibrous
and firmly attached, for this reason reflection of palatal flap is more exhausting. Triangular
flap with distal releasing incision is recommended for palatal approach, the thickness of
the bone around palatal roots is larger than over the buccal roots [2].
Irritants from root canal system produce reaction of the periarticular tissues. Peri
radicular curettage procedure is necessary for removing diseased or reactive tissue
from surface around the tooth. However, complete removing of inflamed tissue could be unfavorable since this granulation-like tissue will be integrated
to the new granulation tissue as part of the healing process [6].
Removal of irritants from root canal system (apical delta,
accessory canals) or iatrogenic conditions (ledge, perforations,
separated instruments) can be achieved through the apical
resection approach. The amount of root-end resection structure
will depend on the need to completely remove the origin of the
problem and create an apical seal.
Case Presentation
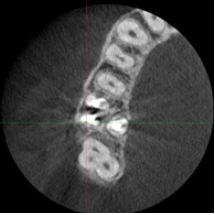
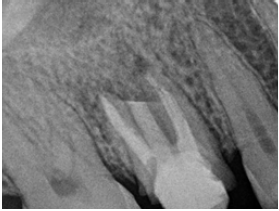
A healthy 34-year-old female presented to Endodontic Department at School of Dentistry, University of Buenos Aires with discomfort on the right palate area. Clinical examination revealed a full provisional crown on tooth #3 and sinus tract on the molar area of the palate (Figure 1). Radiographic examination and CBCT axial view showed previous nonsurgical root canal treatment and fiber post placed in the palatal root. A gutta-percha point size 20 .02 following the sinus tract was placed (Figure 2 & 3) Palatal root-end surgery was discussed and agreed with patient.
Figure 1: Provisional restoration and sinus tract on tooth #3.

Figure 2: Pre op. radiograph with a gutta-percha point size 20 .02 following the sinus tract.

Figure 3: CBCT axial view.
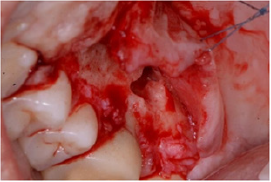
After presurgical rinse with 0.2% chlorhexidine, profound local anesthesia infiltration in both buccal and palatal sides of tooth #3 with 4% carticaine and 1:100.000 adrenaline (Anescart Forte, SIDUS, Buenos Aires, Argentina) was administered, the operating microscope (ZEISS OPMI pico, Carl Zeiss Meditec AG, Germany) was adjusted in order to use it throughout the surgical procedure. A palatal triangular flap was designed with 4mm vertical releasing incision to improve access and visibility. The tissue was tied to the contralateral side with 4-0 silk suture (4-0 ETHILON Nylon Suture, Ethicon Inc., J & J Company, NJ, USA) and the surgical site was exposed (Figure 4).
Figure 4: Surgical site with palatal approach.
Apical root resection was performed with Piezomed handpiece and B6 instrument (W&H Dentalwerk Bürmoos GmbH, Bürmoos, Austria). The cutting level was then evaluated with post op. digital radiograph (Figure 5).
Figure 5: Post op. radiograph.
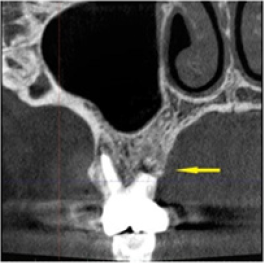
After six months recall, the tooth and the palatal mucosa area were asymptomatic and healthy. A full zirconia crown was cemented as final restoration. CBCT coronal view was evaluated showing palatal root end resection angulation and final restoration (Figure 6-8).
Figure 6: Six months after treatment the palatal surgical site was restored and a full zirconia crown was placed as final restoration.

Figure 7: Buccal view of maxillary first molar with full zirconia crown cemented.

Figure 8: CBCT coronal view showing cutting level angulation of the palatal root (yellow arrow).
Discussion
Limited access, inadequate visualization of root-ends and
flap reflection are obstacles when surgical palatal approach
is an option. Palatal roots are mostly straight, oval in shape
and without isthmus, in addition, they are more difficult to be
detected in periapical radiographs, due to the superposition of
the anatomical structures and zygomatic arch [7].
Limitations for palatal approach includes the chance
to damage the sinus membrane due to the proximity to the
maxillary sinus, provoking iatrogenic sinusitis or injury of the
GPB. The GPB travels in the pterygopalatine fossa, passes through
the pterygopalatine canal, and exits through the greater palatine
foramen which is located between the second and third molars
area [8,9].
Smith et al. [10] analyzed the relationship between the
greater palatine artery and root ends. Over 250 CBCT images
of teeth (126 maxillary first molars and 124 maxillary second
molars) they found that the position was 34% superior, 40%
adjacent, and 21% inferior [10]. In this clinical case report, GPB
location and size was carefully evaluated through CBCT.
Planning flap design could be a challenge since anatomical
variations and characteristics of the tissues it goes through
should be considered. Different factors such as teeth involved,
root shape, periodontal pockets, access visibility, bone covering
the target must be evaluated previously to any oral surgery
[11]. With root-end resection techniques is possible to remove
periapical lesion and decide bevel gradient. Use of magnification
is necessary for achieving small and conservative osteotomy
when is required. In addition, use of ultrasonics tips for root apex
resection is useful for reduce bevel angulation [12]. In this case
report, a bone surgery ultrasonic tip with saw shape was used for
achieving a deep and fine cutting on r esection tip.
Conclusion
Apical root-resection on palatal root of maxillary molars with palatal approach could be favorable in comparison with buccal approach. The greater palatine neurovascular bundle and other anatomic considerations should be carefully evaluated by clinician.
References
- American Association of Endodontists (2020) Glossary of endodontic terms. (10th edn), American Association of Endodontists, Chicago, Illinois, USA.
- Gutmann JL, Harrison JW (1985) Posterior endodontic surgery: anatomical considerations and clinical techniques. International Endodontic Journal 18(1): 8-34.
- Robledo JG, Rodriguez PA (2021) Anatomic variation in palatal root of maxillary second molar: Endodontic management. Open Journal of Stomatology 11(4): 159-165.
- Benjamin G, Ather A, Bueno MR, Estrela C, Diogenes A (2021) Preserving the neurovascular bundle in targeted endodontic microsurgery: A case series. Journal of endodontics 47(3): 509-519.
- Song JE, Um YJ, Kim CS, Choi SH, Cho KS, et al. (2008) Thickness of posterior palatal masticatory mucosa: the use of computerized tomography. Journal of periodontology 79(3): 406-412.
- Lin LM, Gaengler P, Langeland K (1996) Periradicular curettage. International Endodontic Journal 29(4): 220-227.
- Lee SH, Cho SY, Kim DH, Jung IY (2020) Clinical outcomes after apical surgery on the palatal root of the maxillary first molar using a palatal approach. Journal of Endodontics 46(4): 464-470.
- Fu JH, Hasso DG, Yeh CY, Leong DJ, Chan HL, et al. (2011) The accuracy of identifying the greater palatine neurovascular bundle: a cadaver study. Journal of Periodontology 82(7): 1000-1006.
- Rigolone M, Pasqualini D, Bianchi L, Berutti E, Bianchi SD (2003) Vestibular surgical access to the palatine root of the superior first molar: "low-dose cone-beam" CT analysis of the pathway and its anatomic variations. Journal of Endodontics 29(11): 773-775.
- Smith BG, Pratt AM, Anderson JA, Ray JJ (2021) Targeted endodontic microsurgery: Implications of the greater palatine artery. Journal of Endodontics 47(1): 19-27.
- Grandi C, Pacifici L (2009) The ratio in choosing access flap for surgical endodontics: a review. Oral Implantol 2(1): 37-52.
- Del Fabbro M, Corbella S, Sequeira Byron P, Tsesis I, Rosen E, et al. (2016) Endodontic procedures for retreatment of periapical lesions. Cochrane Database Syst Rev 10(10): CD005511.
© 2021 Juan G Robledo. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






