- Submissions

Full Text
Modern Research in Dentistry
Digital Bite Registration of Habitual Occlusion with Specific Skeletal Intraoral Scan Bodies for the Fabrication of a Fixed Full-Arch Prosthesis on Immediate Loading Dental Implants with Full Digital Workflow: Two Case Reports
Marco Serri1*, Andrea Papa2 and Marcello Melis3
1Director, Studio Serri Odontoiatria e Salute, Quartu Sant’Elena (CA), Italy
2Research & Development Manager and Digital Dentistry Manager, LaStruttura S.p.A., Cassano Magnago (VA), Italy
3Private Practice, Cagliari, Italy
*Corresponding author: Marco Serri, Via Monsignor Angioni 64, Quartu Sant’Elena (CA), Italy
Submission: November 11, 2021;Published: December 02, 2021

ISSN:2637-7764Volume7 Issue1
Abstract
Aim: A fixed full-arch prosthesis on immediate loading dental implants, designed in a complete digital
workflow, requires the impressions of both dental arches, the exact position of the dental implants
and the registration of the maxillo-mandibular relationship. In case of surgical interventions requiring
significant modifications of the bone crest or the removal of all the teeth, with alteration and/or swelling
of the soft tissues, it is difficult to have accurate and stable landmarks to match the pre-surgical and the
post-surgical digital impressions. Therefore, the purpose of this study was to introduce a reliable method
to overcome such problem and realize a fixed full-arch prosthesis on immediate loading dental implants
by the use of a complete digital workflow.
Materials and methods: Prior to the surgical procedure and the digital impressions, two unique skeletal
scan bodies, each one combined with a mini-implant, are positioned distally in the dental arch (one left and
one right) where the dental implants are placed, to provide distinctive landmarks that remain unchanged
after surgery. Such procedure allows a perfect matching between the pre-surgical and post-surgical scans,
maintaining the information of the patient’s habitual occlusion in maximum intercuspation.
Result: The use of the skeletal scan bodies enables the oral surgeon to add the data of the patient’s
maxillo-mandibular relationship to the digital work flow.
Conclusion: The present protocol allows to achieve the position of the implants and the patient’s maxillomandibular
relationship in maximum intercuspation in the three dimensions with a single digital scan.
Keywords: Digital impression; Digital workflow; Full-arch prosthesis; Immediate loading; Habitual occlusion; CAD/CAM; Implant scan body; Skeletal scan body
Introduction
In dentistry, several scientific articles show an increasing interest in the digital protocols
[1-4]. They are gradually replacing the traditional analogical laboratory procedures,
demonstrating not only the same efficiency, but also higher precision and accuracy [5-
7]. The workflow used to create a fixed full-arch prosthesis on immediate loading dental
implants using CAD/CAM technology is based on the following 7 steps:
1. preliminary intraoral scan;
2. cone beam computed tomography (CBCT) with radiologic template or with
intraoral radiopaque landmarks;
3. prosthesis guided surgical planning.
4. surgical guide fabrication [8,9].
5. static-guided or computer-guided dynamic surgery
[10,11].
6. intraoral scan with scan bodies after the surgery [12]
7. delivery of the CAD/CAM prosthesis [13].
All mentioned steps need to be followed accurately to avoid
deviations or mistakes that can negatively affect the succeeding
steps [14-16].
Prosthesis guided surgery is followed by the immediate
delivery of a previously designed prosthesis, which is adapted
to become passive on the implants’ abutments. This is usually
needed because the fixtures cannot be perfectly placed in
the bone as planned [17,18]. This step interrupts the digital
workflow, extends the working time, and interferes with the
surgical procedure, decreasing cleanliness and fluency. However,
if the prosthesis is realized after surgery, the procedure starts
with a pre-surgical scan of the dental arches and the maxillomandibular
relationship in maximum intercuspation. Following
surgery, the digital impression of the gingiva and the implants
scan bodies must be obtained. The scan will also include
unchanged anatomic landmarks that were already present in the
pre-surgical scan, together with the recording of the patient’s
habitual occlusion. After surgery, it is very difficult to identify
many anatomic landmarks, because they could be missing,
in case of tooth extraction or because the total prosthesis is
removed due to gingival edema, and because the soft tissues can
be completely altered by the procedure. This makes matching
the pre-surgical and the post-surgical digital impressions very
difficult. In addition, it is necessary to add the recording of the
patients’ habitual occlusion in the digital workflow. Therefore,
after scanning the dental arch with the healing abutments, a waxbite
registration of the maxillo-mandibular relationship is needed
as a reference point that can be used to design and prepare the
temporary prosthesis. Such relationship will be re-evaluated at
the moment of the fabrication of the definitive prosthesis [19].
This analogical step not only interrupts the digital workflow,
but also requires the delivery of the wax registration to the dental
laboratory, in order to produce stereolithographic models of the
dental arches to be positioned in the correct maxilla-mandibular
relationship interposing the wax registration. These models are
then scanned by the laboratory technician. This analogical step
introduces a possible margin of error at different stages. First
of all, the clinical procedure is operator dependent [20,21].
Secondly, the repositioning of the wax registration on the cast
models occluding with the opposing arch is also subject to error
[20,21].
After this step, it is possible to proceed with the digital
workflow by registering the maxillo-mandibular relationship
with the laboratory digital scanner. Based on such record, the
technician produces a temporary full-arch prosthesis applying
the CAD/CAM technique. The purpose of the temporary fixed fullarch
prosthesis is twofold: to allow implants osteointegration (if
the prosthesis is passive and well occlusally balanced), and to
deliver aesthetics and function to the patient. Once the implants
are integrated and both hard and soft tissue are healed and
stable, a new definitive prosthesis is fabricated.
Because of this assumption, the aim of this study was to
introduce a reliable method to digitally record the patients’
maximal intercuspation without interrupting the digital
workflow and minimize the margin of error.
Material and Methods
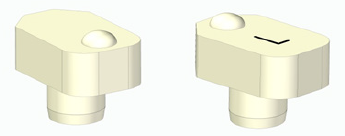
Specific skeletal scan bodies have been designed and fabricated (designed by Dr. Marco Serri, manufactured by Biotec S.r.l., Povolaro di Dueville, Italy). They are unique for each side, to be positioned on the right and left side of the distal parts of the dental arch where the implants are placed. They have an irregular parallelepiped shape with rounded edges on one side, and three facets oriented at a 45° angle on the other side, made of polyether-ether-ketone (PEEK), a biocompatible material. The two contralateral skeletal scan bodies differ in the occlusal surface, due to the opposite location of a hemisphere and the presence of the letter L on the left skeletal scan body. This specific shape, combined with the specific side of positioning, prevents the scanner from detecting the external surfaces of the skeletal scan bodies as identical (Figure 1). For the same reason, also the titanium implant scan bodies (LaStruttura S.p.A., Cassano Magnago, Italy) have a distinct design on their occlusal surface, in order to overcome this problem created by the software.
Figure 1: Skeletal scan bodies.
Case Reports
Two case reports of a fixed full-arch prosthetic rehabilitation on immediate loading dental implants with the use of skeletal scan bodies are presented.
Case 1
In the first case, the prosthetic rehabilitation on dental
implants in the upper arch of an edentulous male patient wearing
a total removable prosthesis is described.
The first step consists in the creation of two holes in the
removable prosthesis in the area of the maxillary second molars,
to allow the housing of the skeletal scan bodies. In each of these
sites, one mini-implant (Biotec S.r.l., Povolaro di Dueville, Italy)
combined with the skeletal scan body is placed (Figures 2 & 3).
At this time, before surgery, four intraoral scans with the skeletal scan body in place were taken: a scan of the maxillary edentulous
mucosa, a scan maxillary arch with the removable prosthesis
in place, a scan of the mandible, a scan of the patient’s habitual
occlusion in maximum intercuspation (Figure 4).
Figure 2A: One mini-implant positioned in the left side of the maxillary arch.
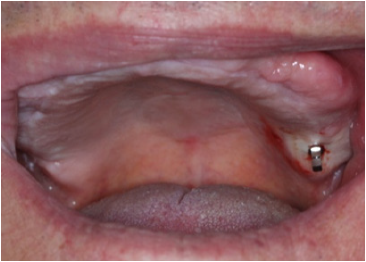
Figure 2B: The two skeletal scan bodies positioned on the maxillary arch.
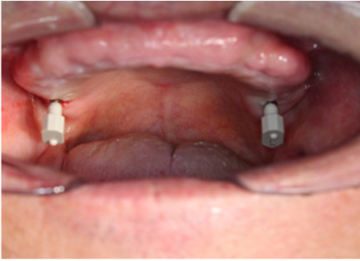
Figure 3: Skeletal scan bodies with the removable prosthesis in place.

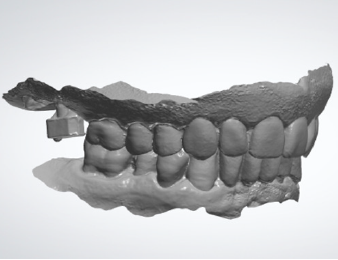
Figure 4A: Digital impression of the maxillary arch with the removable prosthesis in place and the scan bodies.
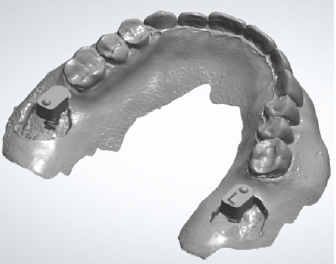
Figure 4B: Digital impression of the antagonist arch.

Figure 4C: Digital impression of the maxillomandibular relationship of patients’ habitual occlusion in maximum intercuspation.
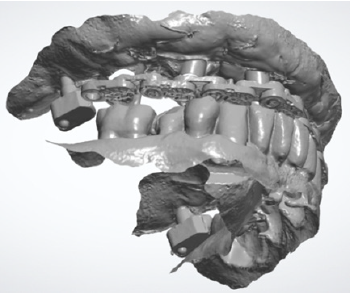
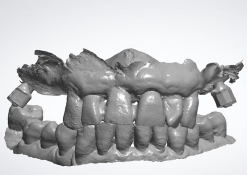
After concluding the surgical phase, the implant scan bodies were connected to the implants and merged together with the universal scan template (Designed by Dr Andrea Papa, produced by LaStruttura S.p.A., Cassano Magnago, Italy), in order to ease the scanning procedure in case of altered or bleeding mucosa (Figure 5). The scan started from the skeletal scan bodies to allow the software to correlate the pre-surgucal and post-surgical scans obtaining a perfect relation with the opposing arch (Figure 6).
Figure 5: Post-surgical digital impression including the skeletal scan bodies, the implant scan bodies and the universal scan template.

Figure 6: Maxillo-mandibular relationship in patient’s habitual occlusion in maximum intercuspation obtained matching the pre-surgical and post-surgical digital scans.
In the resulting post-surgical intermaxillary space, a fixed full-arch temporary prosthesis was digitally designed and manufactured in a complete digital workflow (CAD/CAM) with the occlusal plane parallel to the Camper’s plane and the bipupillary plane, it was then screwed on the implants (Figures 7-12). The definitive prosthesis will be fabricated once the implants are integrated and both hard and soft tissue are healed and stable.
Figure 7: Frontal and sagittal view of the design of the temporary maxillary full-arch prosthesis.
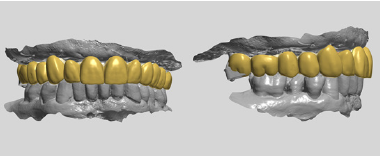
Figure 8A: Maxillary arch immediately after surgery before positioning the temporary full-arch prosthesis.

Figure 8B: Temporary maxillary full-arch prosthesis.

Figure 8C: Temporary maxillary full-arch prosthesis screwed on the implants immediately after surgery.

Figure 9: Control of the correct relationship between the prosthesis’ occlusal plane and Camper’s plane. Right side.

Figure 10: Control of the correct relationship between the prosthesis occlusal plane and the bipupillary plane.
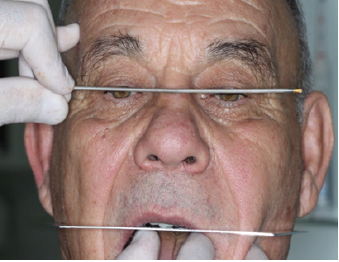
Figure 11: Final aesthetic result.

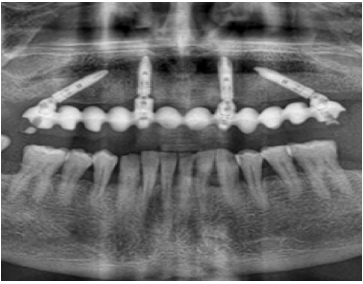
Figure 12: Post-surgical panoramic X-ray.

Management of dental and periodontal pathologies affecting the mandible will not be described in this article.
Case 2
The second case shows the prosthetic rehabilitation of
a male patient suffering from periodontal disease, with five
periodontally compromised anterior teeth in need of extraction.
This case was elaborated in complete digital workflow. A static
guide was designed and manufactured based on cone beam
computed tomography (CBCT) images and intraoral digital scans,
in order to carry out a prosthesis guided surgery.
Before surgery, two mini-implants combined with the
associated skeletal scan bodies were placed in the distal sectors
of the maxilla. Three intraoral digital scans with the skeletal
scan bodies in place were taken: a scan of the maxillary arch, a
scan of the mandible, a scan of the patient’s habitual occlusion in
maximum intercuspation (Figures 13A & 13B).
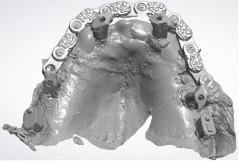
Figure 13A: Digital impression of the maxillary arch and the scan bodies in place.
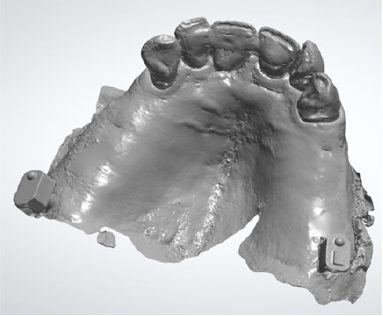
Figure 13B: Digital impression of the maxillomandibular relationship of patients’ habitual occlusion in maximum intercuspation.
At the end of the surgical session, the position of the implants was defined by the use of specific scan bodies connected to each other through the use of the universal scan template. Then, the post-surgical digital scan was carried out, including the entire maxilla, the skeletal scan bodies, the implant scan bodies and the universal scan template (Figure 14).
Figure 14: Post-surgical digital scan including the entire maxilla, the skeletal scan bodies, the implant scan bodies and the universal scan template.
As seen in the previous case, in the resulting post-surgical intermaxillary space, a fixed full-arch temporary prosthesis was digitally designed and manufactured in a complete digital workflow (CAD/CAM) with the occlusal plane parallel to the Camper’s plane and the bipupillary plane, it was then screwed on the implants (Figures 15-22). The definitive prosthesis will be fabricated once the implants are integrated and both hard and soft tissue are healed and stable.
Figure 15: Maxillo-mandibular relationship in patient’s habitual occlusion in maximum intercuspation obtained matching the pre-surgical and post-surgical digital scans.
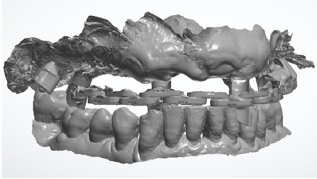
Figure 16: Design of the temporary maxillary full-arch prosthesis. Fontal view.
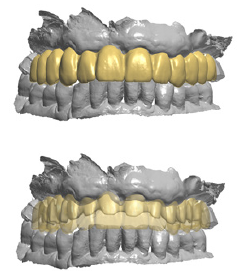
Figure 17: Design of the temporary maxillary full-arch prosthesis. Occlusal view.
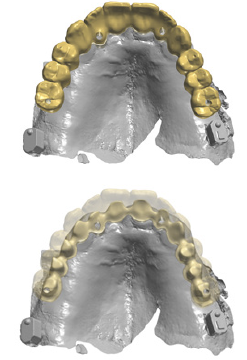
Figure 18: Temporary maxillary full-arch prosthesis screwed on the implants immediately after surgery.

Figure 19A: Control of the correct relationship between the prosthesis’ occlusal plane and Camper’s plane. Right side.
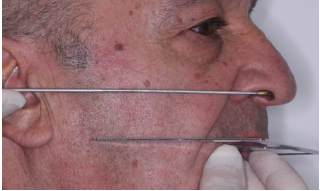
Figure 19B: Control of the correct relationship between the prosthesis’ occlusal plane and Camper’s plane. Left side.
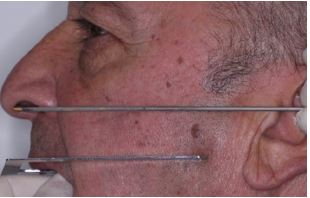
Figure 20: Control of the correct relationship between the prosthesis occlusal plane and the bipupillary plane.

Figure 21: Final aesthetic result.

Figure 22: Post-surgical panoramic X-ray.
Discussion
In the present study, a protocol is proposed to allow the
fabrication of a fixed full-arch prosthesis on immediate loading
dental implants with full CAD/CAM digital workflow, without
interrupting the digital work-flow, and minimizing the margin
of error. A standardized method to perfectly reproduce the presurgical
patient’s habitual occlusion in maximum intercuspation
has been introduced. The use of specific skeletal and implant scan
bodies with a peculiar morphology provides an unique position in
the space and guarantees the unique superimposition of the presurgical
and post-surgical scans. In the cases where the clinician
cannot superimpose the pre-surgical and the post-surgical digital
impressions with his own intra oral scanner (IOS), the laboratory
technicians can benefit from a specific software to match the two
digital scans by the use of the landmarks given by the skeletal
scan bodies.
In some cases, to avoid to interrupt the digital workflow, we
can use the presence of remaining teeth, when their presence does
not hinder the surgical procedure and the fabrication of the dental
prosthesis. They can be extracted afterwards if needed. Natural
teeth can surely represent anatomic landmarks unchanged after
surgery, therefore they can be employed to allow matching of the
pre-surgical and post-surgical digital impressions. However, this
technique is suitable in a limited number of cases. Conversely,
the positioning of the skeletal scan bodies overcomes such limits,
because it can also be utilized in edentulous patients were all the
reference points are missed. Since the main advantage of such
protocol is the reproduction of the patient’s habitual occlusion,
it is most appropriate when treating patients whose habitual
occlusion in maximum intercuspation is deemed correct, with the
occlusal plane parallel to the Camper’s plane and the bipupillary
plane. In fact, if we need to treat edentulous subjects or patients
with improper dental occlusion, it would not be appropriate to
reproduce patient’s habitual occlusion in the new prosthesis.
Nonetheless, the same method could be used after restoring
correct dental occlusion by the use of a temporary full-denture (in edentulous patients) or a dental appliance (in patients with
improper dental occlusion).
Conclusion
The protocol described in the present study allows the fabrication of a fixed full-arch prosthesis on immediate loading dental implants with full CAD/CAM digital workflow, perfectly reproducing the pre-surgical patient’s habitual occlusion in maximum intercuspation. This can be achieved by the use of unique skeletal scan bodies.
References
- Kihara H, Hatakeyama W, Komine F, Takafuji K, Takahashi T, et al. (2020) Accuracy and practicality of intraoral scanner in dentistry: A literature review. J Prosthodont Res 64(2): 109-113.
- Zhongpeng Y, Tianmin X, Ruoping J (2019) Deviations in palatal region between indirect and direct digital models: an in vivo BMC Oral Health 19(1): 66.
- Monaco C, Ragazzini N, Scheda L, Evangelisti E (2018) A fully digital approach to replicate functional and aesthetic parameters in implant-supported full-arch rehabilitation. J Prosthodont Res 62(3): 383-385.
- Takeuchi Y, Koizumi H, Furuchi M, Sato Y, Ohkubo C, et al. (2018) Use of digital impression systems with intraoral scanners for fabricating restorations and fixed dental prostheses. J Oral Sci 60(1): 1-7.
- Ender A, Zimmermann M, Mehl A (2019) Accuracy of complete- and partial-arch impressions of actual intraoral scanning systems in vitro. Int J Comput Dent 22(1): 11-19.
- Mangano F, Lerner H, Margiani B, Solop I, Latuta N, et al. (2020) Congruence between meshes and library files of implant scanbodies: an in vitro study comparing five intraoral scanners. J Clin Med 9(7): 2174.
- Ender A, Mehl A (2011) Full arch scans: conventional versus digital impressions: an in-vitro Int J Comput Dent 14(1): 11-21.
- D'haese J, Ackhurst J, Wismeijer D, De Bruyn H, Tahmaseb A (2017) Current state of the art of computer-guided implant surgery. Periodontol 2000 73(1): 121-133.
- Tatakis DN, Chien HH, Parashis AO (2019) Guided implant surgery risks and their prevention. Periodontol 2000 81(1): 194-208.
- Mandelaris GA, Stefanelli LV, DeGroot BS (2018) Dynamic navigation for surgical implant placement: overview of technology, key concepts, and a case report. Compend Contin Educ Dent 39(9): 614-621.
- Stefanelli LV, Mandelaris GA, DeGroot BS, Gambarini G, De Angelis F, et al. (2020) Accuracy of a novel trace-registration method for dynamic navigation surgery. Int J Periodontics Restorative Dent 40(3): 427-435.
- Gimenez Gonzalez B, Hassan B, Özcan M, Pradíes G (2017) An in vitro study of factors influencing the performance of digital intraoral impressions operating on active wavefront sampling technology with multiple implants in the edentulous maxilla. J Prosthodont 26(8): 650-655.
- Davidowitz G, Kotick PG (2011) The use of CAD/CAM in dentistry. Dental Clin North Am 55(3): 559-570.
- Rutkūna V, Gečiauskait A, Jegelevičiu D, Vaitiekūnas M (2017) Accuracy of digital implant impressions with intraoral scanners. A systematic review. Eur J Oral Implantol 10 Suppl 1: 101-120.
- Schmidt A, Klussmann L, Wöstmann B, Schlenz MA (2020) Accuracy of digital and conventional full-arch impressions in patients. An update. J Clin Med 9(3):688.
- Papadiochou S, Pissiotis AL (2018) Marginal adaptation and CAD-CAM technology: A systematic review of restorative material and fabrication techniques. J Prosthet Dent 119(4): 545-551.
- Unsal GS, Turkyilmaz I, Lakhia S (2020) Advantages and limitations of implant surgery with CAD/CAM surgical guides: A literature review. J Clin Exp Dent 12(4): e409-e417.
- Turkyilmaz I (2019) Keys to achieving successful restoratively-driven implant placement with CAD/CAM surgical guide: A technical note. J Stomatol Oral Maxillofac Surg 120(5): 462-466.
- Preti G (1985) Determination of the prosthetic space in the edentulous patient. Minerva Stomatol 34(1): 13-16.
- Squier RS (2004) Jaw relation records for fixed prosthodontics. Dent Clin North Am 48(2): 471-486.
- Eriksson A, Ockert Eriksson G, Lockowandt P, Eriksson O (2002) Clinical factors and clinical variation influencing the reproducibility of interocclusal recording methods. Br Dent J 192(7): 395-400.
© 2021 Marco Serri. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






