- Submissions

Full Text
Modern Research in Dentistry
Minimizing Prosthetic Intervention to Correct Occlusal Plane Discrepancy in a Complex Fixed- Removable Combination Case
Tzanakakis Emmanouil1* and Zoidis Panagiotis2
1Department of Operative Dentistry, National and Kapodistrian University of Athens, Dental School of Athens, Greece
2Division of Prosthodontics, Department of Restorative Dental Sciences, University of Florida College of Dentistry, Gainesville USA
*Corresponding author: Emmanouil- Georgios Tzanakakis, Perikleous 2, Cholargos 15561, Athens, Greece
Submission: December 22, 2020;Published: January 06, 2021
ISSN:2637-7764Volume6 Issue1
Abstract
Partial edentulism may be the cause of compromised mastication, articulation and changes in esthetic appearance. Although dental implants can provide a viable treatment option to conventional fixed and removable restorations, there are certain reasons that lead patients to reject implant treatment. The conventional prosthodontic approach combining fixed and removable prostheses is well documented and can result in reliable treatment solutions. Prosthetic intervention requires preparation of abutment teeth followed by appropriate prosthetic design in order to re-establish occlusal stability. Such combination full-arch prostheses should preserve health, esthetics and function. The aim of this case report is to present an alternative way to correct occlusal plane discrepancies through a full mouth rehabilitation in a step-by step procedure.
Keywords: Attachments;Combined fixed-removable restoration;Metal clasps;Occlusal plane;Removable dental prosthesis
Introduction
Partial edentulism, if not treated, may lead to complex esthetic and functional problems.
Moreover, patients often postpone their prosthetic treatment due to phsycological or financial
reasons. Most patients with severe edentulism are unaware of the difficulty and the time that
is needed for a proper treatment plan for their prosthetic rehabilitation [1]. Although dental
implants can provide additional support both for fixed and removable restorations, and offer
viable treatment options, some patients tend to reject implants as a treatment solution. The
basic reason would be the widespread misinformation that dental implants require more
complicated and time-consuming procedures. Additionally, the higher cost of the surgical
procedure and the possible post-operative complications make elderly patients reluctant to
implant placement [2].
Conventional prosthodontics involving combination of fixed and removable prostheses
are well documented and account for an acceptable and reliable treatment plan. Prosthodontic
approach requires preparation of abutment teeth and appropriate prosthetic design in order
to re-establish occlusal stability. The combination of fixed and removable prosthodontics is a
reasonable treatment plan when extended edentulous areas are present. The design of such
full-arch prosthesis should preserve health, esthetics, and function [3].
The removable dental prosthesis (RDP) design is a crucial factor for treatment planning.
The selection of major and minor connectors is based on the clinician’s experience and
knowledge. Visible parts of an RDP should first be acceptable by the patient. The dilemma
between clasp retainers and precision attachments is often a matter of controversy. Clasping
is well documented, requires less complicated laboratory procedures and is easier when it
comes to repairing [4,5]. Precision or semi-precision attachments are almost invisible in
anterior regions but increase stress to supporting abutment teeth. Moreover, extra coronal precision attachments work as cantilevers and increase the risk
of abutment failure [4,6]. Clinicians often use crown splinting to
distribute masticatory forces more favorably between abutment
teeth [7-10]. The cost of treatment planning attachments is usually
higher than that for conventional clasping and precise laboratory
procedures and techniques play a significant role for the longevity
of such restorations [11,12].
Occlusal rehabilitation has always been a challenge in
such combination cases. Thorough radiographic and intraoral
examination as well as study cast analysis are imperative to create a
viable treatment plan. Occlusal discrepancies can be evaluated and
corrected by means of a full mouth wax up on the diagnostic casts.
The final result should reestablish esthetics and function. The aim
of this case report is to present the full mouth rehabilitation of a
complicated clinical case in a step-by step procedure.
Case History
A 65-year-old male Caucasian patient presented with a
failing dentition. The patient had never before any prosthodontic
therapy. He reported previous traumatic experience from dental
therapy and claimed that the idea of visiting a dentist caused
psychological stress, explaining that he would only visit the dentist
as an emergency case. The only dental treatment he had received
in the past was the extraction of problematic teeth. Several initial
visits were spent to help the patient overcome his negative attitude
towards dental treatment.
His medical record was free, except he was a heavy smoker.
Dental examination revealed caries, moderate periodontitis,
and loss of posterior occlusal support. Periodontal examination
revealed gingival inflammation and pocket depths lower than
4mm. Significant recession areas were identified, and all teeth were
characterized with good prognosis. Osseous support averaged 50%
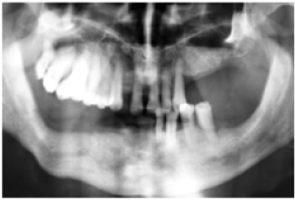
for both maxillary and mandibular teeth (Figure 1).
Figure 1: Initial Panoramic radiograph.
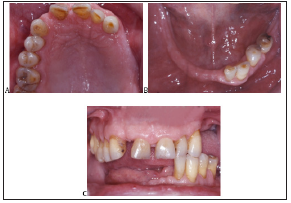
The loss of posterior support due to the absence of posterior teeth resulted in occlusal instability. Several teeth were missing in the maxillary left quadrant. The maxillary arch was characterized as Kennedy Class I according to the classification of the American College of Prosthodontics (Figure 2A). A significant long axis distal turn of the maxillary central incisors and severe abrasion of left lateral and canine teeth were also recorded. A significant occlusal plane discrepancy was present, defined by significant overeruption of right second bicuspid and first molar. The mandibular arch was characterized as a modified Kennedy Class I, with only four teeth present (Figure 2B). Caries were present on the left second bicuspid, as well as lingual inclination of left first and second bicuspid and incisal wear on the remaining teeth. The vertical dimension of occlusion (VDO) was slightly decreased (1-2mm) and maximum inter-cuspal position revealed only three occlusal contacts, resulting to occlusal trauma (Figure 2C).
Figure 2: Preoperative condition.
A. Maxilla.
B. Mandible.
C. Frontal view.
The patient was seeking a treatment plan to improve his
compromised chewing and speaking ability. Patient rejected the
implant option due to increased cost, and his inability to quit
smoking. The patient also wanted to avoid a clasp on the canine
that would compromise esthetics.
After clinical examination and diagnosis and taking under
consideration the above-mentioned restrictions, two different
treatment plans were proposed for the maxillary and mandibular
arch, combining fixed and removable restorations. In the maxilla,
the point of controversy was the occlusal plane correction. The
first treatment plan would include occlusal plane correction by
significantly reducing right maxillary abutment teeth in order to
restore with PFM crowns. This significant tooth reduction would
possibly require endodontic therapies. Maxillary anterior teeth
would be restored with a six-unit bridge. The fixed restoration
would combine with a unilateral removable partial denture.
A second and more conservative treatment plan was
implemented in order to correct this inverted occlusal plane.
Instead of reducing posteriorly, anterior teeth elongation (2-3mm)
was decided. Those teeth would be prepared regardless, in order
to fabricate the anterior bridge restoration that would combine with the RDP. Concerning this RDP, an extra-coronal semi-precision
attachment (ERA; Sterngold Co) was proposed distally to the left
canine to improve esthetics [13-15].
In the mandible, the left lateral incisor was planned for
extraction due to poor prognosis. The treatment plan included
three splinted metal ceramic crowns for the remaining mandibular
teeth (left canine and bicuspids) and a RPD. A simple conventional
bilateral clasp design was proposed for the RPD since there were no
esthetic demands [16-18].
Figure 3: Diagnostic wax-up to verify treatment plan.
A. Frontal view.
B. B, C Lateral views.
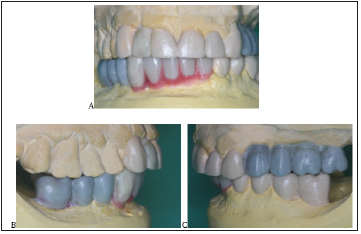
A detailed wax-up was performed to justify that this second,
conservative approach would be a viable solution (Figures 3A,B,C).
Conservative periodontal treatment, followed by the preparation
of all maxillary and mandibular abutment teeth was performed.
Provisional restorations were fabricated chairside according to
the wax up and an interim RDP was delivered to ensure proper
posterior support. Provisional restorations were trial tested for
three months to ensure esthetic and functional requirements as
well as patient’s compliance with oral hygiene instructions.
Final impressions were performed using the double mix
technique. Occlusal records included face-bow registration and
precise centric relation registration. Metal frameworks try-in,
verified complete marginal covering and passive fit. Bisque try in,
allowed for esthetic adjustments. Definitive RDP impressions were
performed using custom trays and polyether impression material.
RPDs were also examined for accurate fit. A final try-in stage
following RDP processing, allowed for a final occlusal adjustment
of both fixed and removable restorations.
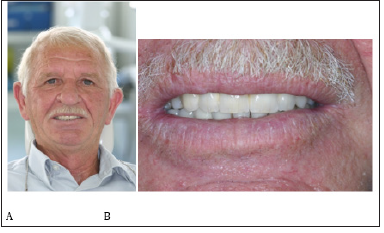
The final cementation of the maxillary fixed restorations was
performed using conventional Glass-Ionomer cement (Riva, SDI Co,
USA). In the mandible, an adhesive protocol was selected and a resin
cement (Panavia F2.0; Kuraray Co) was used, due to limited number
of abutments and increased expected torque values. The final
result fulfilled patient’s expectations and demands, significantly
improving his smile (Figures 4-6).
Figure 4: Definitive restorations.
A. Frontal view.
B. B, C Lateral views.

Figure 5: Extraoral preoperative condition.
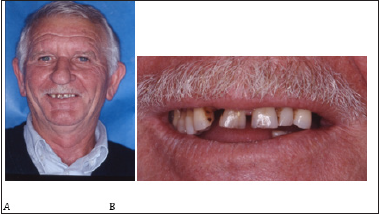
Figure 6:Extraoral post-operative condition.
Discussion
In this case report, an alternative, conservative approach for the correction of maxillary occlusal plane discrepancy was implemented, without compromising long-term prosthetic prognosis.
Over eruption is a common problem encountered when
opposing teeth are not present for extended periods of time [1]. The
basic guideline for prosthodontic treatment in these complicated
cases is to correct occlusal disharmony by decreasing this occlusal
plane angulation [15].
The selected conservative prosthetic protocol followed in this
case, offered certain clinical advantages. First, the treatment plan
was less invasive and required minimum reduction of dental tissue.
Fewer teeth were prepared and right maxillary teeth were left intact.
As a result, no root canal treatment and no surgical procedures
(crown lengthening for maxillary right teeth) were performed.
Minimizing the number of metal ceramic crowns, the number of
root canals and surgical procedures, significantly reduced the final
cost for the patient [18]. The standard occlusal plane correction
protocol would involve both surgical and endodontic procedures as
well as more PFM crowns, therefore it would be more expensive.
There was a need for minimal increase in vertical dimension of
occlusion(1-2mm) for enhanced aesthetics. Temporary all acrylic
RPDs were used for a trial period of three months to ensure esthetics
and function. Posterior support was restored and neuromuscular
adaption to removable appliances was also confirmed.
Splinting remaining anterior teeth into a six-unit FDP, ensured
adequate support for missing right lateral incisor, minimizing the
possibility of flare up and provided better stress distribution for
RDP support. An alternative design of two 3-unit separate FDPs
(centrals to canines) was not advocated since it would not provide
protection against anterior teeth flare-out.
Patients with multiple missing teeth regain their self-confidence
when the final prosthetic restoration is esthetically acceptable
[15]. The use of an ERA semi-precision attachment offered an
aesthetic result without the unacceptable metal display of a
conventional clasp design RPD [12,16,17]. A unilaterally positioned
ERA attachment functions as a rigid connector since its vertical
resiliency was restricted by the major connector (palatal zone) and
the occlusal rests on maxillary molars. A Swing lock design was not
proposed as alternative treatment option due to reduced available
vestibular depth, the presence of extended frenum attachment and
the anticipated high torque values [14].
Other possible alternative treatment plans would involve
either the use of dental implants or the fabrication of an RPD with
conventional metal clasps. Implant supported FDPs were rejected
due to cost and conventional RDPs due to esthetics. The patient
wanted to avoid a metal clasp on the canine that would be visible
at smile, and the all-acrylic interim RDP did not satisfy his aesthetic
demands [15].
The prosthetic complications in this case report were a clasp
failure for the mandibular RDP and an acrylic tooth detachment
(left central incisor) over five years of observation time. The patient
followed a strict maintenance protocol every six months for five
years, which included conservative periodontal treatment, light
occlusal adjustments, replacement of the male ERA attachment and
evaluating the need for denture base relines.
References
- Craddock HL, Youngson CC, Manogue M, Blance A (2007) Occlusal changes following posterior tooth loss in adults. Part 1: a study of clinical parameters associated with the extent and type of supraeruption in unopposed posterior teeth. J Prosthodont 16: 485-494.
- Zitzmann NU, Scherrer SS, Weiger R, Lang NP, Walter C (2011) Preferences of dental care providers in maintaining compromised teeth in relation to their professional status: implants instead of periodontally involved maxillary molars? Clin Oral Implants Res 22(2): 143-150.
- D’Souza D, Dua P (2011) Rehabilitation strategies for partially edentulous prosthodontic principles and current trends. Med J Armed Forces India 67(3): 296-298.
- Ben-Ur Z, Shifman A, Aviv I, Gorfil C (1999) Further aspects of design for distal extension removable partial dentures based on the Kennedy classification. J Oral Rehabil 26(2): 165-169.
- Campbell SD, Cooper L, Craddock H, Hyde TP, Nattress B, et al. (2017) Removable partial dentures: The clinical need for innovation. J Prosthet Dent 118(3): 273-280.
- Aviv I, Ben-Ur Z, Cardash HS (1989) An analysis of rotational movement of asymmetrical distal-extension removable partial dentures. J Prosthet Dent 61(2): 211-214.
- Altay OT, Tsolka P, Preiskel HW (1990) Abutment teeth with extracoronal attachments: the effects of splinting on tooth movement. Int J Prosthodont 3(5): 441-448.
- Burns DR, Unger JW (1994) The construction of crowns for removable partial denture abutment teeth. Quintessence Int 25(7): 471-475.
- Charkawi HG, Wakad MT (1996) Effect of splinting on load distribution of extracoronal attachment with distal extension prosthesis in vitro. J Prosthet Dent 76(3): 315-320.
- Itoh H, Caputo AA, Wylie R, Berg T (1998) Effects of periodontal support and fixed splinting on load transfer by removable partial dentures. J Prosthet Dent 79(4): 465-471.
- Ma PS, Brudvik JS (2008) Managing the maxillary partially edentulous patient with extensive anterior tooth loss and advanced periodontal disease using a removable partial denture: a clinical report. J Prosthet Dent 100(4): 259-263.
- Wang H, Zhang Y, Yao D, Chen J, et al (2011) Effects of rigid and nonrigid extracoronal attachments on supporting tissues in extension base partial removable dental prostheses: A nonlinear finite element study. J Prosthet Dent 105(5): 338-346.
- Berg T, Caputo AA (1992) Load transfer by a maxillary distal-extension removable partial denture with cap and ring extracoronal attachments. J Prosthet Dent 68(5): 784-789.
- Brudvik JS (1999) Advanced removable partial dentures. Quintessence, Chicago, USA pp. 107-110.
- Beaumont AJ (2002) An overview of esthetics with removable partial dentures. Quintessence Int 33(10): 747-755.
- Krol AJ (1973) Clasp design for extension-base removable partial dentures. J Prosthet Dent 29(4): 408-415.
- Donovan TE, Cho GC (2003) Esthetic considerations with removable partial dentures. J Calif Dent Assoc 31(7): 551-557.
- Wagner B, Kern M (2000) Clinical evaluation of removable partial dentures 10 years after insertion: success rates, hygienic problems, and technical failures. Clin Oral Investig 4(2): 74-80.
© 2021 Tzanakakis Emmanouil. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






