- Submissions

Full Text
Modern Research in Dentistry
Lip Changes Following Non-Extraction Orthodontic Treatment
Kaveh Baharvand Ahmadi1, Peter H Buschang2 and Sawsan Tabbaa3*
1Kaveh Baharvand Ahmadi, Orthodontics Private Practice, Texas, USA
2Peter H Buschang, Texas Director of Orthodontic Research. A&M University College of Dentistry, USA
3Sawsan Tabbaa, Director of Orthodontic Research, School of Orthodontics, Jacksonville University, USA
*Corresponding author:Sawsan Tabbaa, Associate Professor, Orthodontics Research Director, School of Orthodontics, Brooks Rehabilitation College of Health Sciences, Jacksonville University, 2800 University Blvd N. Jacksonville. Fl. 32211, USA
Submission: August 01, 2019;Published: August 08, 2019

ISSN:2637-7764Volume4 Issue3
Abstract
Introduction: The purpose of this study was to predict the lip changes in Class I adolescents and adults following non-extraction orthodontics treatment.
Methods: This longitudinal retrospective study evaluated the pre- and post-treatment lateral cephalograms of 40 adults and 72 adolescents with Angle Class I molar relationships and crowding in both arches. The horizontal and vertical changes of 15 landmarks, along with lip thickness and taper, were evaluated. The sample was randomly divided into two group; 76% of the subjects were used to develop the multivariate regression formulas; the remaining 24% served as a validation sample.
Result: Adolescent lips moved inferiorly and anteriorly during treatment; adult lips showed lesser inferior movement, little or no anterior movement and decreases in thickness. Males demonstrated significantly greater inferior and, mostly, greater anterior changes of lip position. The multivariate regressions explained 48-59% and 41-69% of the vertical and horizontal variation of the lip changes, respectively. When the prediction equations were applied to the validation sample, with correlations ranged from 0.60-0.84, indicating external validity.
Conclusion: The lip changes of Class I adolescents and adults treated with non-extraction orthodontic treatment can be predicted with fair to moderate accuracy. Adults’ lips became compressed and thinner, while the upper lip thickness of adolescents did not change or become slightly thicker.
Introduction
Esthetic ideals are continuously evolving in today’s age of global media and merging cultures. It has been estimated that 3 out of 4 patients come to orthodontists to improve facial attractiveness [1]. Lips are among the most important features that determine attractiveness [2]. For example, lip thickness has been shown to be critical in the perception of beauty, [3,4] with thicker lips being positively related to higher esthetic perceptions [5]. The public notices the lip changes more than nose or chin changes [6]. It is essential for orthodontists to differentiate between lip changes due to treatment and those due to growth. For untreated subjects between 6-18 years of age, upper lip length increases approximately 4mm, thickness increases 1-2mm and protrusion decreases only slightly (0.5mm); lower lip length (9-10mm) and thickness (2-3mm) both increase [7]. Adolescents’ lips become relatively more retrusive over time, substantially longer, and somewhat thicker [8,9]. In contrast, adults show different patterns of change. Untreated adult soft tissues change at much slower rates. Their lips continue to retrude and tend to flatten, especially at the older ages [10-12].
Relationships between the lips and the underlying dental structures were demonstrated as early as 1834.7 Soft tissue changes following the orthodontic treatment are usually considered secondary to tooth and skeletal alterations [13]. Some authors have reported simple linear relationships between hard tissue and soft tissue profile changes [14,15]. Ratios, which relate lip changes to the amount of incisor retraction, have been reported to range from 1:1.75 to 1:2.2 for the upper lip, and from 1:1.2 to 1:1.4 for the lower lip [16,17]. Importantly, ratios assume that lip movements can be predicted by a single hard tissue measure, which limits their ability to predict [18,19]. Moreover, ratios imply that the relationship between hard and soft tissue changes is linear, which is not necessarily the case [8,20,21]. Ratios also provide no information about their predictive accuracy. Ratios have been reported to bias soft tissue changes, due to the fact they do not account for the effects of the other independent variables on the measured dependent variable [21].
Predicting the changes of the lips during treatment requires information from more than one variable. The changes of the lips measured from the commonly used profile planes are often confounded by growth, so that the actual changes in lip position during treatment can differ not only in magnitude, but also in direction [22]. Treatment changes in both upper and lower lip positions have been explained by a multiple regression formulas using various hard and soft tissue variables, attaining correlations of up to 0.98 [23]. While multiple regressions provide more precise estimates of soft tissue changes than ratios or bivariate regression, and are less biased, it remains controversial whether they produce clinically meaningful predictions for upper lip movements [18]. The purpose of the present study was to predict changes in lip position during non-extraction orthodontic treatment in Class I patients. Previous studies have used mixed (including more than one Angle class) samples, which could be problematic because of the different mechanics utilized could produce a wide range of incisor movements [13,24,25]. Moreover, most of the literature focuses on the prediction of the lip response in extraction cases [8,13,21]. Lip response to the non-extraction treatment, in which lips can be compressed, might be expected to be different than lip response to extraction treatment, in which the lips are relaxed [26]. There has been only one study that used a multivariate approach to predict the lip changes of a limited sample of non-extraction adult patients [21].
Material and Methods
Selection criteria
This longitudinal retrospective study was based on 40 adults and 72 adolescents, with crowding of at least 1mm in both the maxilla and mandible who completed a comprehensive orthodontic treatment at Jacksonville University school of Orthodontics. This study was approved by the Research Ethics Committee of the Institutional Review Board (IRB) at Jacksonville University (IRB # 2016-30). Approximately 64.3% of subjects were female. The average ages of the adolescents and adults were 13.1±1.4 years and 27.4 ±1.7 year, respectively. Females older than 15 years and males older than 17 years were considered to be adults. To be included in the study, the subjects had to have:
A. Angle Class I molar relationships;
B. Radiographs with lips in relaxed position.
C. Non-extraction treatment;
They were excluded if they had:
A. Syndromes, craniofacial anomalies, or congenitally missing teeth;
B. Orthognathic or cosmetic facial surgery.
C. Treatment terminated prematurely due to poor compliance.
D. Poor quality pretreatment (T1) or post-treatment (T2) cephalograms.
Cephalometric procedures and measurements
All radiographs were taken on calibrated cephalostats, with patients biting on their back teeth. Magnification differences between cephalostats were corrected prior to data analysis using a ruler that was included on each of the cephalograms. Seven soft tissue and 11 hard tissue landmarks were digitized by the primary investigator on each cephalogram (Table 1) (Figure 1) using the Dolphin Imaging Software©. The primary investigator superimposed the T1 and T2 tracings using the structural method, as described for the cranial base [27]. The horizontal and vertical changes of the landmarks were evaluated relative to constructed horizontal and vertical reference planes [28-32]. The horizontal reference plane (HRP) was registered on sella (S) and oriented 7 degrees inferior to the sella-nasion (S-N). The vertical reference plane (VRP) is drawn from Sella, perpendicular to the HRP (Figure 1).
Figure 1:A) Hard and soft tissue landmarks and B) measurement of upper and lower lip thickness.

Table 1:Hard and soft tissue landmarks.

There were primary-outcome variables (dependent), including soft tissue A point, upper lip point, stomion superioris, lower lip point, soft tissue B point, and stomion inferioris. There were nine independent measures, including the anterior nasal spine, A point, prosthion, U1 convex, U1 tip, L1 tip, infradentale, B point and pogonion. Upper and lower lip thickness and taper were computed (Table 2) (Figure 1). Technical reliability was estimated based on duplicate tracings of 15 randomly selected cephalograms, digitized approximately 14 days apart. Systematic errors were not statistically significant. Method errors ranged from 0.15 to 0.49mm, with the vertical changes of A point showing the largest random errors.
Table 2:Upper and lower lip thickness and taper.

Statistical analysis
SPSS (SPSS Inc, Version 24, Chicago, Ill) was used for the statistical evaluations. Based on skewness and kurtosis, the distributions were all normal. T-tests were used to evaluate between-group differences. Single sample t-tests were used to determine whether positions of the measured landmarks had changed significantly during the treatment. Stepwise multiple regression analyses were performed to predict the treatment changes. The sample was randomly divided into two group; 76% of the subjects were used to develop the regression formulas and the remaining 24% served as a validation sample. The validation sample was used to ensure that the predictions could be applied to other patients.
Result
Adolescents vs adults
Table 3:Comparison of the Vertical changes of the soft and hard tissue changes (mm) in adolescence and adults treated with non-extraction treatment.
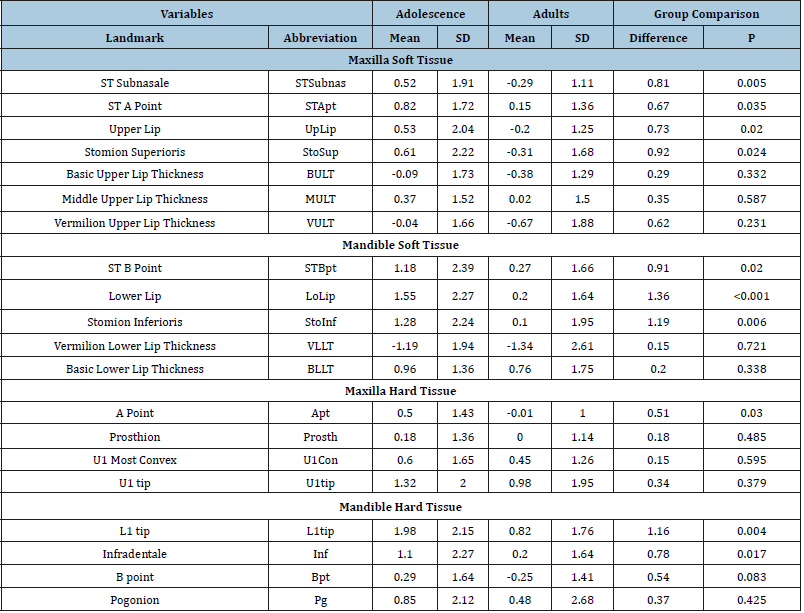
*Statistically significant changes (P<0.05) are shown in bold.
Table 4:Comparison of the horizontal changes of the soft and hard tissue changes (mm) in adolescence and adults treated with non-extraction treatment
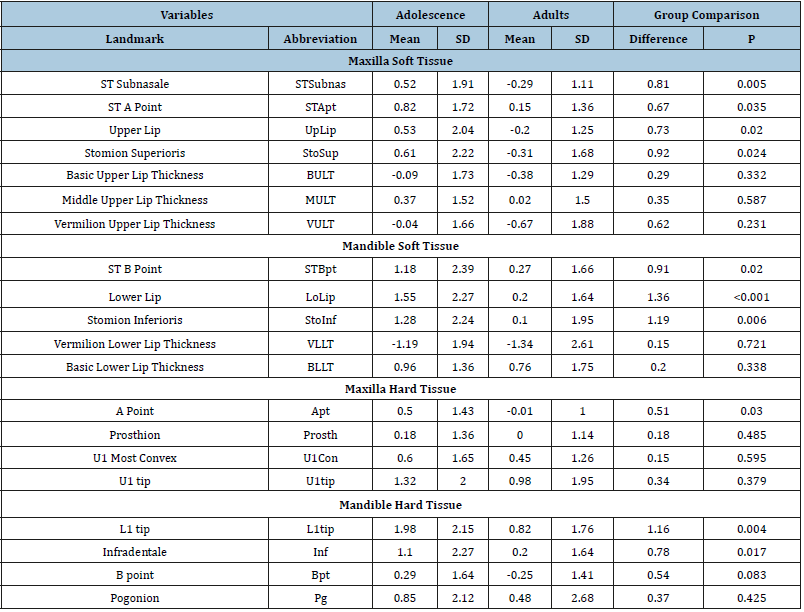
*Statistically significant changes (P<0.05) are shown in bold.
Adolescents showed statistically significant (p<.05) inferior movements of all landmarks (Table 3). Upper lip taper of adolescents did not change and lower lip taper decreased significantly. Four of the adult landmarks showed statistically significant inferior movements (Apt, L1tip, Bpt and Pg). Generally, the hard tissue landmarks showed greater inferior movements than the soft tissue landmarks. With the exception of Pg, LLTap and ULTap, all of the vertical landmarks showed statistically significant differences between adolescents and adults, with adolescents showing greater inferior movements than adults. All of the adolescent landmarks except Bpt and Prosth displayed statistically significant anterior movements (Table 4). Adolescents also showed significant increases in middle upper and lower lip thickness. There were significant increases in adults upper and lower lip thickness, and significant anterior movements of the upper and lower incisors. Ten of the measurements showed statistically significant betweengroup differences. The upper lip and Apt came forward significantly more in adolescents than adults. The lower lip, lower incisor and infradentale came forward significantly more in adolescents.
Male vs female
Table 5:Comparison of the Vertical changes of the soft and hard tissue changes (mm) in Males and Females treated with non-extraction treatment.
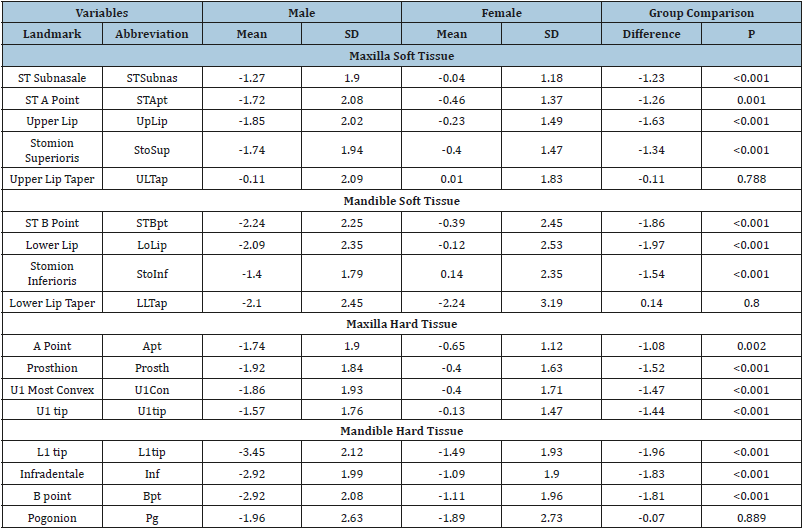
*Statistically significant changes (P<0.05) are shown in bold.
Table 6:Comparison of the horizontal changes of the soft and hard tissue changes (mm) in Males and Females treated with non-extraction treatment.
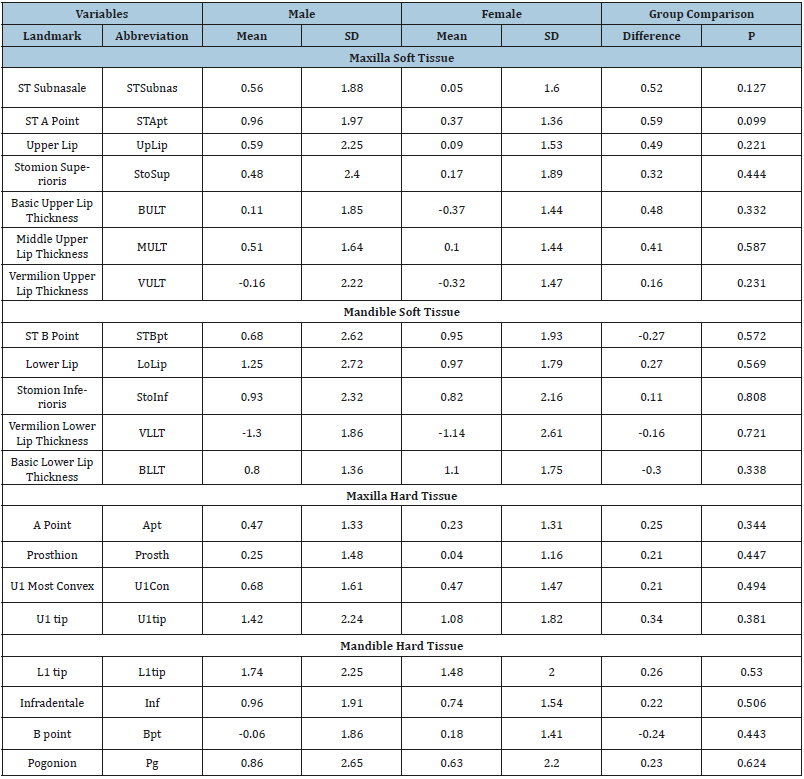
*Statistically significant changes (P<0.05) are shown in bold.
Males showed statistically significant vertical changes of all measurements (Table 5); 10 measures (mostly hard tissues) changed significantly in females. L1tip and STBpt showed the greatest inferior movements among the hard and soft tissues measures, respectively. With the exception of lip taper and Pg, all the vertical measures showed significant sex differences. Males underwent significantly more inferior movement than females. There were no significant sex differences for changes of lip taper. Except for 4 of the landmarks (UpLip, StoSup, Prosth and Bpt) males demonstrated significant anterior movements (Table 6). Females showed significant anterior movements of all landmarks except STSubnas, UpLip, Sto, SupProsth, and Bpt. Basic lower lip thick increased and vermilion thickness decreased. There were no sex differences in the horizontal changes that occurred.
Multivariate stepwise regression analyses and validation
Table 7:Stepwise multiple regression models for the upper and lower lip changes for hard and soft tissue variables.
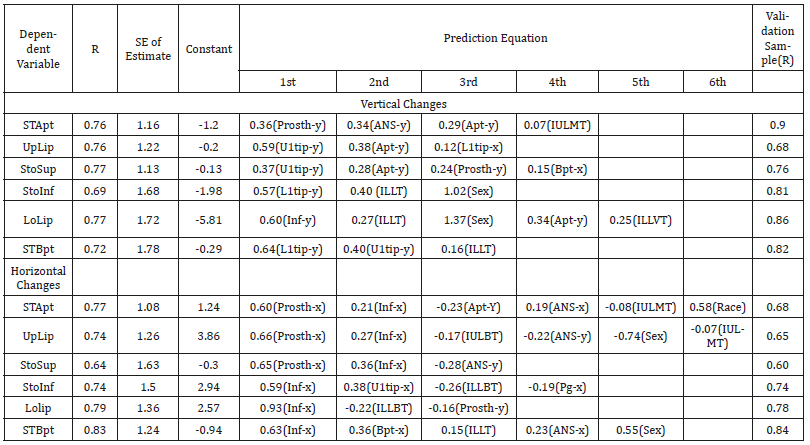
The multivariate stepwise regressions produced correlations explained 48-59% of the variations. The vertical changes of prosthion and ANS were the most important variables predicting the vertical changes of STApt, whereas the U1tip and Apt were the most important for predicting UpLip and StoSup (Table 7). The vertical changes of the lower lip were most closely associated with L1tip, ILLT and sex. When the regression equations were applied to the validation sample, the associations (ranging from 0.68- 0.90) between the actual and predicted changes were generally stronger than the original correlations. The regressions (Table 7) explained 41-69% of the variation in the horizontal changes of the lips that occurred during treatment. Three to six variables entered the predictive equations. The horizontal changes of prosthion and infradentale were the two measures most closely associated with horizontal upper lip changes, while the horizontal changes of infradentale was most closely related to horizontal lower lip changes. Similar relations were produced when the prediction equations were applied to the validation sample, with correlations ranging from 0.60-0.84.
Discussion
Incisors procline in the adult non-extraction cases treated for crowding. The present study showed forward movements of the upper and the lower incisor crowns. Forward tipping of the incisors in non-extraction treatment has been reported [33,34]. Proclination of the incisors in adults could have been the result of leveling and alignment. In addition, slightly more proclination of the upper than lower incisors was observed in the present than previous studies, possibly due to the MBT prescription (+17 degrees of torque for upper incisors, -6 degrees for lower incisors) that was used to treat the patients. Adult lip thickness decreases as a result of nonextraction treatments. Based on the present study, the lips did not move forward significantly, despite the forward movement of the underlying hard tissue. This shows that non-extraction treatment in adults compresses the lips slightly, decreasing upper and the lower vermilion thickness. Both decreases [34] and increases [35] of upper lip thickness have been reported after non-extraction treatment of white subjects. The increases were observed for a mixed sample of adults and adolescents, which could have been affected by growth.
Little or no growth was expected for the adults in the present study, and the changes can be attributed mainly to treatment. Unlike adults, adolescents undergo inferior growth movements of both the soft and hard tissues. The soft tissue changes followed the same direction as the underlying hard tissues: the lips became longer as the underlying hard tissue grew inferiorly. Inferior movements of adolescent lips have been reported in multiple growth studies [36- 38]. Based on the differences in the vertical soft tissue changes of adults and adolescents, growth must be considered as the major factor determining the inferior movements observed. During nonextraction treatment, most hard and soft tissue landmarks (except prosthion and B point) moved anteriorly in adolescents. Contrary to adults, who showed thinning of lips with treatment, the upper lip of adolescents did not change or became slightly thicker. Increases in lip thickness are expected in the untreated adolescents, especially in the mid-lip region [4,6]. Increases of the upper lip thickness and decreases of the lower lip vermilion thickness have been previously reported for adolescents treated nonextraction [39]. It appears that the normal thickening of the upper lip and the vermilion part of the lower lip that occurs in untreated adolescents is camouflaged by treatment.
The basic part of the lower lip exhibits both growth and treatment thickening effects. Males experienced more inferior movement of the hard and soft tissues than females. In the present study, the upper and the lower lips followed the underlying hard tissues, and moved more inferiorly in males than females. While upper lip length increased similarly in both sexes, lower lip increased only in males. Increases of the upper lip length in untreated males and females have been reported after 11 years of age [38]. Since the present sample consisted of both growing and non-growing patients, growth probably interacted with treatment to produce the lip response observed. There are no sex differences in the horizontal changes in lip position during non-extraction treatment. The present study showed no differences in the horizontal movements of the soft tissue landmarks, nor in the changes of the lip thickness that occurred. Subtelny [40] reported sex differences in untreated subjects, with males showing greater increases in lip thickness than females, especially at the vermilion borders [38,40]. Oliver reported greater increases in the upper lip thickness in the orthodontically treated growing males than females [41]. However, it was not clear if Oliver’s sample was treated with extractions or non-extraction. In the present study, the lips were growing and the incisors proclined. As previously explained, lips are compressed as the hard tissues are moved anteriorly, counteracting the effects of growth. While the stepwise multiple regressions in the present study provided more precise estimates than simple bivariate regression, the predictions were only fair to moderate. Previous studies also have reported better predictability using a regression model, as might be expected [18,20,23,25,34].
The regression models required at least three independent variables to explain the variability of the lip changes, substantiating the complexity of soft tissues changes that occur during treatment. The regression models in the present study explained 48-59% of the variability of the vertical changes of the lips. Changes in the positions of prosthion and the upper incisor tip were most closely related to the vertical changes of the upper lip. Similarly, infradentale and the tip of the lower incisor were most closely related to changes of lower lip position. Prosthion has previously been identified as an important hard tissue landmark related to the upper lip changes, [2,8,23] as has the tip of the upper incisor, [8,20] infradentale [8] and tip of the lower incisors [21,25]. While no other study has used multiple regression to predict vertical lip changes in non-extraction cases, a multivariate approach was used to explain 75% of the variability of the changes in the extraction cases [18]. This indicates that it may be more difficult to predict the vertical lip changes in non-extraction than extraction cases, perhaps due to variability in lip compression during treatment.
The multiple regressions in the present study predicted the horizontal lip changes moderately well, explaining 41-69% of the variation in the changes that occurred. Based on a smaller sample, Shirvani and coworkers reported substantially higher multiple correlations for non-extraction cases than the present study, perhaps due to their focus on adults [34]. Once again, changes in the positions of prosthion and infradentale were most closely associated with the horizontal changes of the overlying lips. The importance of prosthion and infradentale in determining horizontal lip changes during extraction treatment has been previously demonstrated [20,23,25,31]. It has also appears that the horizontal changes of the lower lip can be predicted with a higher level of accuracy in extraction than non-extraction cases [18,33].
Conclusion
Non-extraction orthodontic treatment of adults and adolescents is expected to affect the lip as the following:
A. The upper and the lower lips become thinner in adults.
B. Upper lip thickness of adolescents does not change or becomes slightly thicker; the lower lip became thinner at the vermilion border and thicker at its base.
C. Males showed more vertical, but similar horizontal, lip changes than females.
D. Treatment changes in upper and lower lip position can be predicted with fair to moderate levels of accuracy.
References
- Plaks V, Kong N, Werb Z (2015) The cancer stem cell niche: how essential is the niche in regulating stemness of tumor cells? Cell Stem Cell 16(3): 225-238.
- Melzer C, von der Ohe J, Lehnert H, Ungefroren H, Hass R (2017) Cancer stem cell niche models and contribution by mesenchymal stroma/stem cells. Mol Cancer 16(1): 28.
- Ouchi T, Morikawa S, Shibata S, Takahashi M, Yoshikawa M, et al. (2018) Recurrent spindle cell carcinoma shows features of mesenchymal stem cells. J Dent Res 97(7): 779-786.
- Gupta R, Singh S, Hedau S, Nigam S, Das BC, et al. (2007) Spindle cell carcinoma of head and neck: an immunohistochemical and molecular approach to its pathogenesis. J Clin Pathol 60(5): 472-475.
- Leventon GS, Evans HL (1981) Sarcomatoid squamous cell carcinoma of the mucous membranes of the head and neck: a clinicopathologic study of 20 cases. Cancer 48(4): 994-1003.
- Watson RF, Chernock RD, Zhang KH, Michel LS, Adkins DR, et al. (2015) Epidermal growth factor receptor expression in spindle cell carcinomas of the head and neck. Head Neck Pathol 9(3): 360-368.
© 2019 Sawsan Tabbaa. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






