- Submissions

Full Text
Modern Research in Dentistry
Bone-Borne versus Tooth-Borne Rapid Palatal Expansion (RPE) Treatment in Mixed Dentition; Literature Review
Sondus Ahmad Alkadri*, Maria Cristina Pollmann and Eugénio Martins
Department of Orthodontics, Faculty of Dental Medicine, University of Porto, Porto, Portugal
*Corresponding author: Sondus Ahmad Alkadri, Department of Orthodontics, Faculty of Dental Medicine, University of Porto, Porto, Portugal
Submission: February 24, 2018;Published: May 07, 2018

ISSN:2637-7764Volume2 Issue3
Abstract
Introduction: Bone-anchored maxillary expanders have been invented to provide extreme pure skeletal expansion. There are studies that address the clinical effectiveness and outcomes of bone-borne maxillary expansion; mostly on adults or with surgical assistance.
Objective: To review publications studied the effectiveness of Bone-Borne Maxillary Expander (BBME) compared with tooth-borne maxillary expander (TBME) in mixed dentition subjects.
Search strategy: Literature review dated from 2006 to June 2016 on PubMed and B-on databases was conducted. Relevant data were extracted, grouped and analyzed concerning: total amount of expansion, skeletal vs. dental expansion, side effects, and long-term stability of TBME and BBME. 16 articles were selected: 11 studies addressed TBME, one study was a comparison between TBME and BBME, and 4 studies addressed BBME.
Discussion: Amounts of skeletal expansion and dental expansion varied between TBME and BBME; it also varied within TBME itself in different studies. Inter-coronal widths of maxillary molars in TBME were significantly greater than their counterparts in BBME. Generally, TBME showed a reduction in alveolar bone thickness on the buccal aspect of the anchorage teeth. Buccal tipping in TBME studies was small or high up to 19 degrees, in BBME group it was clinically trivial.
Conclusion: Current available reviewed studies led to inconsistent conclusions regarding the superiority of BBME over TBME in mixed dentition patients. They were mostly done on subjects above 12 years old. Although theoretically and logically this claim may seem valid, no evidence-based conclusion could be made. Future investigations on mixed dentition patients are highly recommended.
Keywords: Rapid palatal expansion; Mixed dentition; Tooth-borne; Bone-borne; Skeletal anchored
Abbreviations: RPE: Rapid Palatal Expanders; CPCT: Cone Beam Computed Tomography; CT: Computed Tomography; LDCT: Low Dose Computer Tomography; FEM: Finite Element Model
Introduction
Maxillary Constriction (MC) is a deficiency of the maxillary bone in the transverse plane which is found in a large percentage of orthodontic patients; usually, associated with other types of malocclusion such as Class III and II [1-3]. Therefore, MC is considered one of the major problems in orthodontic practice. There are many clinical methods to correct MC, and choosing the most suitable method depends on the patient’s age and the main cause of the problem.
The orthopedic maxillary expansion is considered one of the most popular and conservative methods [4]. Maxillary expansion has been accomplished after developing its concept with a wide diversity of fixed expansion appliances; from simple wire configurations to more complicated designs that include jackscrews connected to orthodontic bands or acrylic elements, and to the most recent designs that use mini-implants inserted directly in the palatal bone, however, benefits and risks are key in choosing the type of expansion appliance. Evidence-based dentistry nowadays is a high priority in clinical practice. Evidence-based information is used in the decision-making process of treatment planning whenever it is available to the clinician [5].
The conventional Tooth-borne Rapid Maxillary Expander (TBME) has been used for a long time to correct the maxillary transverse deficiency. Although an acceptable expansion can be achieved, TBME has undesirable side effects as a result of using teeth for anchoring the appliance. Tipping of the posterior teeth, buccal root resorption, buccal cortex dehiscence or fenestration, limited skeletal expansion, relapse or instability of the expansion are some of the post-treatment complications that might occur after treatment with TBME [6,7].
Recently, after the innovation of Temporary Anchorage Devices (TADs), new anchorage techniques took place. Skeletal anchorage used mini-implants and palatal screws as anchoring tools for maxillary expansion. Forces from an activated screw can be oriented directly to the palatal bone instead of being transmitted through anchoring teeth. This can be clinically achieved through placement of mini screws on the palatal vault providing temporary skeletal anchorage for maxillary expansion. Bone-anchored maxillary expanders have been invented in order to provide extreme pure skeletal expansion without dento-alveolar detriment. In fact, there are studies that addressed the clinical effectiveness and outcomes of bone-borne maxillary expansion, but they were done mostly on adults in surgical assistance cases. Unfortunately, few clinical published studies have compared the effectiveness of tooth-borne and bone-borne maxillary expansion in mixed dentition subjects (under 12 years old). Other studies [8-11] addressed bone-borne expanders in subjects much older than 12 years old, teenagers. Therefore, there should be more extensive clinical studies before considering bone-borne expansion a more effective method for maxillary expansion than tooth-borne expansion.
The primary purposes of this paper were first to provide orthodontists with up-to-date research outcomes which compare the effectiveness and side effects of bone-borne rapid maxillary expansion with tooth-borne rapid maxillary expansion in mixed dentition patients, and second to highlight the importance of carrying out further clinical studies in order to have conclusive outcomes.
The present narrative review was undertaken to answer the following questions:
a) Is bone-borne anchored rapid maxillary expansion more effective in the treatment of mixed dentition patients than tooth-borne?
b) Does BBME induce more skeletal expansion than dentoalveolar expansion?
c) Does BBME eliminate the dental and periodontal complications reported after using TBME?
d) Which expander of TBME and BBME has long-term stability and less relapse?
Search Strategy
The research was made from international studies found on PubMed and B-on platforms. The used keywords were: “Rapid Palatal Expansion”, “Mixed dentition”, “Tooth-borne”, “Boneborne”, “Skeletal anchorage”. Using simple keywords leads to multiple results, and therefore, combinations of keywords were used. To identify possible articles, the initial articles’ selection was performed by title and abstract according to the following inclusive criteria:
• Published in English
• Published between 2006 and July 2016
• Samples of mixed dentition patients (until age 12 years old) or Finite Elements modules
Articles were excluded whenever they had one of the following:
• RPE treatment with a combination of other orthodontic appliances
• Surgically assisted RPEs
• Late permanent dentition subjects (above 12 years old)
• Patients with unilateral or bilateral cleft lip, anomalies, syndromes or disorders
• Systematic reviews, case reports, opinion articles, theses
When the abstract did not provide enough information to make a decision, the article was completely analyzed.
Results
Table 1

525 articles were retrieved from database searching: PubMed platform yielded 104 publications and B-on platform yielded 421. Based on the title, the initial selection phase yielded 39 articles, and 8 duplicated articles were eliminated. The researcher obtained the full-text versions for the second phase evaluation of the remaining 31 articles. 15 articles were excluded for reasons listed in Table 1 [9-23]. Articles that used any type of tissue-tooth-borne expanders. i.e. (Haas expander) were excluded since the present study aimed to evaluate two types of anchorage, tooth-borne and bone-borne. Otherwise, we would have had to create a third group for the tissue-tooth-borne type. As a result of articles scanning, almost 16 articles met the eligibility criteria, and they were selected for this dissertation, (Table 2) [6,7,24-37]. From the selected articles, the needed data referring to sample size and age, type of appliance, the total amount of expansion, retention period and follow-up, skeletal and dentoalveolar expansion and Buccal tipping, side effects and relapse was extracted as shown in Table 3 [24,25,26-33]. The table was constructed from articles which addressed the variables mentioned above.
Table 2: Included studies.
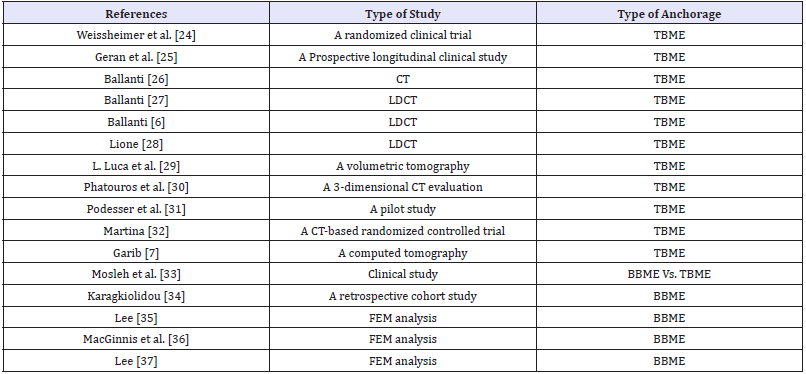
Table 3: Included studies.
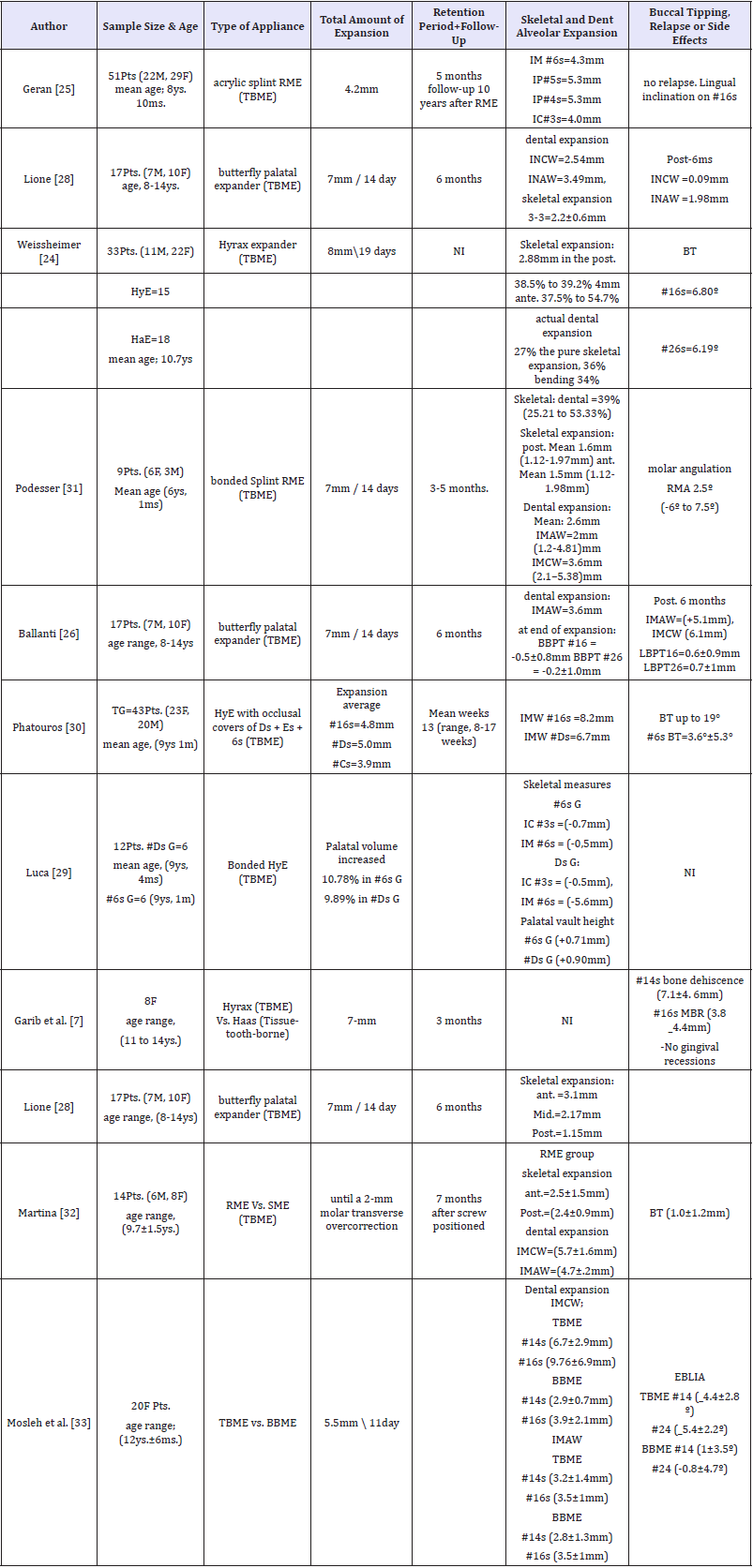
INAW: Inter-Incisor Apex Width; INCW: Inter-Incisor Crown Width; IMCW: Inter-Molar Crown Width; IMAW: Inter-Molar Apex Width;BT: Buccal Tipping; RMA: Right Molar Angulation; LMA: Left Molar Angulation; BBPT: Buccal Bone Plate Thickness; BBPT: Palatal Bone Plate Thickness; EBLIA: External Buccopalatal Inclination Angle; IM: Inter-Molar; IP: Inter-Premolar; IC: Inter-Canine; #3s: Permanent Canines; #4s: First Premolars; #5s: Second Premolars; #6s: First Molars, #16: Right First Permanent Molar; #26: Left First Permanent Molar; #14: Right First Premolar; #24: Left First Premolar; #Cs: Deciduous Canines; #Ds: First Deciduous Molars; #Es: Second Deciduous Molars; NI: Indicated Mentioned; Post. R: Posterior Region; Ant. R: Anterior Region; Mid: Middle Region; Post-6ms: Post 6 Months; Hye: Hyrax Expander; Hae: Haas Expander; G: Group; Ys: Years; Ms: Months; Pts: Patients; M: Male; F: Female; TBME: Tooth- Borne Maxillary Expander; BBME: Bone-Borne Maxillary Expansion; Mm: Millimeter
Discussion
Total amount of expansion
At the end of the active phase of TBME, all studies showed significant increments in the transversal width of the maxilla. However, the total amount of expansion was different across these studies due to the type of appliance, duration of treatment, and rate of screw activations. The range of the total amount of expansion was from 4.2mm [25] to 8mm [24].
Phatouros [30] used a 3-dimensional CT to evaluate the morphological dentoalveolar effects of the palate after treatment with bonded TBME on 43 subjects, with a mean age of 9.1 years and compared the results with a control group. He recorded a total expansion with 6.7mm between primary molars and 8.2mm between first permanent molars.
Mosleh et al. [33] used the CBCT to compare the transverse changes during maxillary expansion with TBME and BBME on 20 girls aged 12±6 years. She used the traditional Hyrax Expander anchored on the maxillary first premolars and first permanent molars as a TBME. For Bone-anchorage, she used a bone-borne rapid maxillary hyrax expander (BBRPE) which consisted of a traditional hyrax expander anchored on the maxillary first molars and 4 mini screws inserted palatally to the posterior teeth. Although Mosleh [33] used a 7mm jackscrew; the total possible activation was only 5.5mm during a period of 11 days since 1.5mm screw expansion was disbursed during the appliance construction due to insertion reasons. Therefore, the same total amount of expansion was applied for both expanders.
Dento-alveolar versus skeletal expansion
Generally, the expansion pattern described as triangular in most of the studies which used with TBME, since the sutural opening was greater anteriorly than posteriorly [24,28,31].
Using CBCT, Weissheimer et al. [24] reported that skeletal expansion gained by Hyrax Expander accounted for 37.5% to 54.7% in the anterior region, and 38.5% to 39.2% of the total expansion in the posterior region. Besides, the sutural expansion in Lion’s study accounted for 43% and 16% of the total expansion (7mm) in anterior and posterior regions, respectively [28]. Nevertheless, other studies observed a parallel pattern; the skeletal displacement was homogenous along the palatal suture [27,32].
Weissheimer et al. [24] and Podesser et al. [31] have reported that TBMEs produce a greater amount of expansion at the alveolar level than the sutural level. Nevertheless, Weissheimer et al. [24] stated that the pure skeletal effect was greater than the real dental one.
Luca [29] used CBCT to evaluate skeletal and dentoalveolar effects of TBME anchored either on deciduous or permanent teeth. He concluded that RPE anchored on the deciduous teeth produces greater intermolar skeletal transverse variations, whereas RPE anchored on the permanent teeth leads to greater intermolar dental variations.
Among the revised articles, the skeletal expansion amount produced by TBME varied throughout the palatal suture. In general, greater amounts have been recorded in the anterior region compared with the posterior ones [24, 28, 31]. The amounts of the mean of palatal suture expansion in the anterior region ranged between 1.5mm [31] and 4mm [24], while in the posterior region it ranged between 1.1mm [31] and 2.88mm [24].
The skeletal and dental effects of expansion can be measured by the net change in inter-coronal width. Generally, with TBME, the expansion extent at crowns level was superior to that at sutural level [6,31-33]. However, intermolar width showed a wide variety across the studied articles. Mosleh et al. [33] recorded the highest width change (9.7±2.1mm), while the lowest width was (3.6mm) recorded by Podesser [30] and Luca [29]. Likewise, the highest inter-premolar width was in the first premolar area with the amount of (6.7±2.9mm) as recorded by Mosleh [33]. The lowest width was 5.3mm as recorded by Geran [25].
Mosleh et al. [33] reported a statistically significant increment in the skeletal palatal dimensions in the TBME group. However, the average changes between both groups (TBME and BBME) was not statistically significant. Meanwhile, comparing the inter-coronal widths of the maxillary permanent molars and first premolars, the TBME group resulted in significantly greater widths compared with the BBME group. However, the difference in inter-apical widths between both groups was not significant [33].
Lee [37] compared the skeletal displacement of craniofacial structures resulting from maxillary expansion with TBME (traditional Hyrax) and BBMEs with or without surgical assistance. He observed that at mid-palatal suture both TBME and non-surgical type of BBME produced greater expansion in the anterior region than in the posterior one, whereas at the dental level, they showed more expansion on the posterior teeth than anterior ones. In fact, he used an adult skull model (fused palatal suture) in the finite element analysis [37].
Lee [35] also used FEM to compare the effects of different types of BBMEs with micro-implants. Two types of pure bone-borne expanders were used. In type 1, micro-implants were placed 3mm lateral to the mid-palatal suture, but in type 2 they were placed at the palatal slopes. Meanwhile, type 3 was hybrid hyrax expander (BBHyE), while type 4 was a surgically assisted tooth-borne hyrax expander. Among bone-borne expanders, Type 2 showed the least total alveolar movements across all teeth and buccal inclination, it also produced parallel mid-palatal expansion. He recommended using BBME with TADs placed in the palatal slopes for efficient treatment outcomes [35]. Nevertheless, the study of Karagkiolidou et al. [34] showed an excellent survival percentage accounted for 98% when the miniscrews of RPE appliance were placed in the paramedian anterior palate. A High survival rate supports AlSamak’s [38] study results that showed the paramedian area as the best site for TAD’s placement in the palate.
Adverse Effects (AEs)
The traditional TBME transmits the forces from the screw to the anchorage teeth through the arms of the appliance which usually leads to undesirable critical concerns. One of these concerns is related to the periodontium since these forces produce compression and tension forces on the periodontal ligament of the supporting teeth. As a result, alveolar bone resorption, dental tipping, gingival recessions, and/or reduction in the buccal cortical plate of the anchoring teeth might clinically occur [39-41]. These consequences or ‘‘Adverse Effects’’ (AEs) of heavy forces on sutures, anchoring teeth, and periodontium structures have been investigated by some authors such as Ballanti [6], Garib [7], Lagravere [10], Gunyuz Toklu [11]. The bone-borne expander has been used in order to maximize the orthopedic effects and limit the post-treatment concerns caused by teeth anchorage.
Many authors [6,7,26] reported a reduction in the thickness of the alveolar bone on the buccal bone plate of the anchoring teeth. Ballanti [6,26] used CT to assess the periodontal effects of TBME on dento-alveolar structures immediately at the end of the active expansion and after a retention period of 6 months. He reported a significant reduction in the thickness of buccal bone of the anchoring teeth ranging from 0.2 to 0.5mm. On the other hand, from the palatal point of view, he reported an increase in the bone plate thickness in a range between 0.6 to 0.7mm resulting from bone apposition. Neither attachment loss, bone dehiscence, root resorption, nor fenestrations were observed. At the end of the observation, he concluded that a 6-month retention period was enough for the recovery of the buccal and lingual bone plates thickness [6,26].
Likewise, Garib et al. [7] evaluated the periodontal effects after RME with tooth-borne (Hyrax Expander) in contrast to toothtissue- borne (Haas Expander) expanders by means of CT scanning. At the periodontal level, Hyrax group showed a higher reduction in alveolar bone thickness on the buccal aspect of the banded teeth, corresponding to 0.6 - 0.9mm. In contrast, the lingual bone plate thickness increased with a mean of 0.8 to 1.3mm. In addition, Garib et al. [7] recorded the greatest amount of bone dehiscence among the anchoring teeth, especially at the first premolars (4.6-7.1mm), and at the mesiobuccal aspect of the first molars (3.8-4.4mm) [7].
According to Weissheimer [24], Podesser [31], Ballanti [26], Luca [29], Phatouros [30] and Mosleh [33] studies, there was a significant buccal tipping observed on the anchoring teeth with TBME. Phatouros et al. [30] observed more buccal tipping with RPE anchored on deciduous teeth than on permanent teeth. This buccal tipping is owed principally to the alveolar process bending as Kartalian et al. [42] explained. There was noticeable variability in the buccal tipping degrees with TBMEs regardless of the expander’s type. Some authors reported neglectable buccal tipping of approximately 1 degree [32] or none, others reported large amounts up to 19 degrees [30].
In the comparison study of Mosleh [33] between TBME versus BBME, the TBME group expressed the greatest extent of molar rolling, whereas the buccal rolling in BBME group was clinically trivial. Likewise, MacGinnis, [36] used Finite Element Method (FEM) to assess the effects of BBRPE in comparison with the effects of traditional Hyrax Expander. The BBRPE group expressed lower rotational movement and less teeth tipping by preventing alveolar bone bending in contrast with the Hyrax group. MacGinnis [36] suggested the usage of BBRPE as a beneficial expander in young patients.
Relapse and long-term stability
The transverse dimension of the mid-palatal suture was the same before treatment and after a 6-month retention period [28]. This proves that keeping the RPE appliance in situ as a passive retainer is recommended to permit the interdigitation of palatal shelves [43].
In a prospective clinical trial, Geran et al. [25] used the dental casts of the maxillary and mandibular arches to compare the long-term stability of dental arch changes after treatment with TBME (Splint acrylic expander) in early mixed dentition patients; followed by a comprehensive orthodontic treatment in permanent dentition. Regarding the long-term changes, Geran [25] reported a significantly greater decrease in the maxillary first premolars width in the treatment group, while he recorded a significantly smaller decrease in the maxillary arch perimeter and width in the treatment group, in comparison with the control group. In the overall observation period, he recorded a 3.8mm long-term increase in the maxillary arch perimeter of the treated patients over that of the control group [25].
However, Current available reviewed studies and clinical trials led to different inconsistent conclusions regarding the claim of the superiority and effectiveness of bone-borne over tooth-borne maxillary expansion on mixed dentition patients. These studies were mostly performed on adolescents or adults with surgical assistance. Although theoretically and logically this claim may seem valid, no evidence-based conclusion could be made. Thus, future investigations on mixed dentition patients are highly recommended.
Conclusion
The present literature review showed that:
a) Both types of RPE used in mixed dentition patients are able to produce transverse skeletal effects by opening the mid-palatal suture regardless of the used anchorage method. However, the amount of skeletal expansion versus dental one varied between both RPEs, TBME and BBME, and also within TBME itself in different studies.
b) Both types had a significant increase in intermolar and inter-premolar widths; though they were greater in TBME
c) Buccal tipping and alveolar bending occurred with both types of expanders; however, in TBME occurred to significantly higher degrees.
d) Reduction of buccal alveolar bone thickness was significant in most studies which used TBME. Indeed, palatal bone apposition was observed.
e) A 6-month retention period is recommended to permit palatal suture healing, minimize relapse and provide long-term stability.
References
- Baccetti T, Franchi L, McNamara JA, Tollaro I (1997) Early dentofacial features of Class II malocclusion: a longitudinal study from the deciduous through the mixed dentition. Am J Orthod Dentofacial Orthop 111(5): 502-509.
- Baccetti T, McGill JS, Franchi L, McNamara JA, Tollaro I (1998) Skeletal effects of early treatment of Class III malocclusion with maxillary expansion and face-mask therapy. Am J Orthod Dentofacial Orthop 113(3): 333-343.
- Baccetti T, Franchi L, McNamara JA (2000) Treatment and posttreatment craniofacial changes after rapid maxillary expansion and facemask therapy. Am J Orthod Dentofacial Orthop 118(4): 404-413.
- Don Joondeph DM (2016) The Power Chain.
- Bennett S, Tooth L, McKenna K, Rodger S, Strong J, et al. (2003) Perceptions of evidence‐ based practice: A survey of Australian occupational therapists. Australian Occupational Therapy Journal 50(1): 13-22.
- Ballanti F, Lione R, Viarani S, Fanucci E, Cozza P (2008) Post-retention effects of rapid maxillary expansion on nasal cavity and on periodontal structures. Oral Implantol (Rome) 1(3-4): 95-103.
- Garib DG, Henriques JF, Janson G, de Freitas MR, Fernandes AY (2006) Periodontal effects of rapid maxillary expansion with tooth-tissue-borne and tooth-borne expanders: a computed tomography evaluation. Am J Orthod Dentofacial Orthop 129(6): 749-758.
- Lagravere MO, Carey J, Heo G, Toogood RW, Major PW (2010) Transverse, vertical, and anteroposterior changes from bone-anchored maxillary expansion vs traditional rapid maxillary expansion: a randomized clinical trial. Am J Orthod Dentofacial Orthop 137(3): 304.e1-e12.
- Farhangfar A, Bogowicz P, Heo G, Lagravère MO (2012) Palatal bone resorption in bone-anchored maxillary expander treatment. Int Orthod 10(3): 274-288.
- Lagravere MO, Gamble J, Major PW, Heo G (2013) Transverse dental changes after tooth-borne and bone-borne maxillary expansion. Int Orthod 11(1): 21-34.
- Gunyuz Toklu M, Germec-Cakan D, Tozlu M (2015) Periodontal, dentoalveolar, and skeletal effects of tooth-borne and tooth-bone-borne expansion appliances. Am J Orthod Dentofacial Orthop 148(1): 97-109.
- Christie KF, Boucher N, Chung CH (2010) Effects of bonded rapid palatal expansion on the transverse dimensions of the maxilla: a cone-beam computed tomography study. Am J Orthod Dentofacial Orthop 137(4 Suppl): S79-S85.
- Mohan CN, Araujo EA, Oliver DR, Kim KB (2016) Long-term stability of rapid palatal expansion in the mixed dentition vs the permanent dentition. Am J Orthod Dentofacial Orthop 149(6): 856-862.
- Mutinelli S, Manfredi M, Guiducci A, Denotti G, Cozzani M (2015) Anchorage onto deciduous teeth: effectiveness of early rapid maxillary expansion in increasing dental arch dimension and improving anterior crowding. Prog Orthod 16: 22.
- Mummolo S, Marchetti E, Albani F, Campanella V, Pugliese F, et al. (2014) Comparison between rapid and slow palatal expansion: evaluation of selected periodontal indices. Head Face Med 10: 30.
- Mutinelli S, Cozzani M, Manfredi M, Bee M, Siciliani G (2008) Dental arch changes following rapid maxillary expansion. Eur J Orthod 30(5): 469- 476
- Habeeb M, Boucher N, Chung CH (2013) Effects of rapid palatal expansion on the sagittal and vertical dimensions of the maxilla: a study on cephalograms derived from cone-beam computed tomography. Am J Orthod Dentofacial Orthop 144(3): 398-403.
- Garib DG, Menezes MHO, Filho OGS, dos Santos PBD (2014) Immediate periodontal bone plate changes induced by rapid maxillary expansion in the early mixed dentition: CT findings. Dental Press J Orthod 19(3): 36-43.
- Gracco A, Malaguti A, Lombardo L, Mazzoli A, Raffaeli R (2010) Palatal volume following rapid maxillary expansion in mixed dentition. Angle Orthod 80(1): 153-159.
- Brunetto M, Andriani JDSP, Ribeiro GLU, Locks A, Correa M, et al. (2013) Three-dimensional assessment of buccal alveolar bone after rapid and slow maxillary expansion: A clinical trial study. Am J Orthod Dentofacial Orthop 143(5): 633-644.
- Wilmes B, Nienkemper M, Drescher D (2010) Application and effectiveness of a mini-implant- and tooth-borne rapid palatal expansion device: the hybrid hyrax. World J Orthod 11(4): 323-330.
- Ngan P, Wilmes B, Drescher D, Martin C, Weaver B, et al. (2015) Comparison of two maxillary protraction protocols: tooth-borne versus bone-anchored protraction facemask treatment. Prog Orthod 16: 26.
- Nienkemper M, Wilmes B, Franchi L, Drescher D (2015) Effectiveness of maxillary protraction using a hybrid hyrax-facemask combination: a controlled clinical study. Angle Orthod 85(5): 764-770.
- Weissheimer A, de Menezes LM, Mezomo M, Dias DM, de Lima EMS, et al. (2011) Immediate effects of rapid maxillary expansion with Haas-type and hyrax-type expanders: A randomized clinical trial. Am J Orthod Dentofacial Orthop 140(3): 366-376.
- Geran RG, McNamara JA, Baccetti T, Franchi L, Shapiro LM (2006) A prospective long-term study on the effects of rapid maxillary expansion in the early mixed dentition. Am J Orthod Dentofacial Orthop 129(5): 631- 640.
- Ballanti F, Lione R, Fanucci E, Franchi L, Baccetti T, et al. (2009) Immediate and post-retention effects of rapid maxillary expansion investigated by computed tomography in growing patients. Angle Orthod 79(1): 24- 29.
- Ballanti F, Lione R, Baccetti T, Franchi L, Cozza P (2010) Treatment and post treatment skeletal effects of rapid maxillary expansion investigated with low-dose computed tomography in growing subjects. Am J Orthod Dentofacial Orthop 138(3): 311-317.
- Lione R, Ballanti F, Franchi L, Baccetti T, Cozza P (2008) Treatment and post treatment skeletal effects of rapid maxillary expansion STUDIED with low-dose computed tomography in growing subjects. Am J Orthod Dentofacial Orthop 134(3): 389-392.
- Luca L, Enrico A, Angela A, Chiara DAA, Giuseppe S (2015) Rapid maxillary expansion on the permanent teeth versus the deciduous teeth: Comparison of skeletal and dentoalveolar effects by volumetric tomography. Journal of the World Federation of Orthodontists 4(1): 2-7.
- Phatouros A, Goonewardene MS (2008) Morphologic changes of the palate after rapid maxillary expansion: A 3-dimensional computed tomography evaluation. Am J Orthod Dentofacial Orthop 134(1): 117-124.
- Podesser B, Williams S, Crismani AG, Bantleon HP (2007) Evaluation of the effects of rapid maxillary expansion in growing children using computer tomography scanning: a pilot study. Eur J Orthod 29(1): 37-44.
- Martina R, Cioffi I, Farella M, Leone P, Manzo P, et al. (2012) Transverse changes determined by rapid and slow maxillary expansion - a low-dose CT-based randomized controlled trial. Orthod Craniofac Res 15(3): 159- 168.
- Mosleh MI, Kaddah MA, Abd ElSayed FA, ElSayed HS (2015) Comparison of transverse changes during maxillary expansion with 4-point boneborne and tooth-borne maxillary expanders. Am J Orthod Dentofacial Orthop 148(4): 599-607.
- Karagkiolidou A, Ludwig B, Pazera P, Gkantidis N, Pandis N, et al. (2013) Survival of palatal miniscrews used for orthodontic appliance anchorage: a retrospective cohort study. Am J Orthod Dentofacial Orthop 143(6): 767-772.
- Lee HK, Bayome M, Ahn CS, Kim SH, Kim KB, et al. (2014) Stress distribution and displacement by different bone-borne palatal expanders with micro-implants: a three-dimensional finite-element analysis. Eur J Orthod 36(5): 531-540.
- MacGinnis M, Chu H, Youssef G, Wu KW, Machado AW, et al. (2014) The effects of micro-implant assisted rapid palatal expansion (MARPE) on the nasomaxillary complex-a finite element method (FEM) analysis. Prog Orthod 15(1): 52.
- Lee SC, Park JH, Bayome M, Kim KB, Araujo EA, et al. (2014) Effect of bone-borne rapid maxillary expanders with and without surgical assistance on the craniofacial structures using finite element analysis. Am J Orthod Dentofacial Orthop 145(5): 638-648.
- AlSamak S, Gkantidis N, Bitsanis E, Christou P (2012) Assessment of potential orthodontic mini-implant insertion sites based on anatomical hard tissue parameters: a systematic review. Int J Oral Maxillofac Implants 27(4): 875-887.
- Haas AJ (1961) Rapid expansion of the maxillary dental arch and nasal cavity by opening the midpalatal suture. The Angle Orthodontist 31(2): 73-90.
- Starnbach H, Bayne D, Cleall J, Subtelny JD (1966) Facioskeletal and dental changes resulting from rapid maxillary expansion. Angle Orthod 36(2): 152-164.
- Davis WM, Kronman JH (1969) Anatomical changes induced by splitting of the midpalatal suture. Angle Orthod 39(2): 126-132.
- Kartalian A, Gohl E, Adamian M, Enciso R (2010) Cone-beam computerized tomography evaluation of the maxillary dentoskeletal complex after rapid palatal expansion. Am J Orthod Dentofacial Orthop 138(4): 486-492.
- Mew J (1983) Relapse following maxillary expansion. A study of twenty- five consecutive cases. Am J Orthod 83(1): 56-61.
© 2018 Sondus Ahmad Alkadri. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






