- Submissions

Full Text
Modern Research in Dentistry
Contemporary Implantology - Possibilities and Constraints
Mladen Vukovic*
Faculty of Dentistry University of Belgrade, Serbia
*Corresponding author: Mladen Vukovic, DMD, PhD student at the Faculty of Dentistry, University of Belgrade, Dr. Subotica 6, Street 11000 Belgrade, Serbia
Submission: April 20, 2018;Published: May 04, 2018

ISSN:2637-7764Volume2 Issue3
Mini Review
Every human being, sooner or later, faces tooth loss. The reasons for this can be multiple - a disease of the tooth that begins with a caries lesion, so that, if no adequate treatment is done in time, the process spread to the dental chamber, capturing the pulp and its associated structures, and continued its spread further to the root of the tooth and periapical tissue. Tooth loss can also lead to the disease of soft tissue structures - dental meat initially manifesting inflammation - gingivitis, so that, in case of lack of adequate therapy, the inflammatory process spreads to bone structures and ultimately leads to loss of teeth. Parodontopathy is a disease that in the advanced stage, in stages 3 and 4, leads to oscilation and loss of teeth.
Loss of teeth leads to functional, aesthetic and psychological problems. Functional deficiency manifested in the loss of basic functions of the stomatognathic system - chewing, swallowing, speech and breathing. In addition, due to the loss of teeth inevitably leads to resorption of the alveolar ridge and shrink basal bone. About 88% of patients with partial number of teeth or totally toothless have problems with chewing and speaking. Aesthetic defects are manifested by reducing the height of the face, reducing the labio-mental angle, deepening the wrinkles on the face, the rotation of the chin ahead (which contributes progeny appearance), lowering the corners of the mouth, loss of muscle tone mimic muscles (leading to thinning edge vermilion), deepening of nasolabial grooves, the larger the angle Filtrum-columella, increasing the length of the upper lip (increases the visibility of the teeth when smiling), and lowering the attachment of the buccal and chin muscle, which contributes to the so-called “ Relaxed facial appearance”. Psychological consequences represent a range of different psychological disorders that can cause various forms of neurotic changes [1].
Loss of teeth, various forms of partial or total edentulism can be offset by various forms of prosthetic restorations, fixed or mobile. All these restorations have their advantages and disadvantages, as well as strict indications when they should be applied. A significant shift in the management of partial and total loss of teeth was the use of implants that are allow making prosthetic restorations in those cases where the resorption of the alveolar ridge is so advanced that it did not allow the creation of high-quality dentures, or when the tooth loss is expressed, with a large interdental spaces, as aggravating factor for the development of fixed restorations -crowns and bridges. Advantages of prosthetic implants are multiple -prevention of further bone resorption, establishing and maintaining the intermaxillary relationship, improvement in function of the masticatory apparatus and facial expressions (muscle tone), an aesthetic effect - it looks like the teeth to spring out of the alveoli, speech enhancement, occlusion, stability and retention of mobile prosthetic restorations, the release of the needs of neighboring teeth grinding, improving overall psychological state, etc [2].
There are a number of different implant systems on the market, of which the most famous are: Nobel Biocare, Straumann, Biohorizons, Bredent, ITI, Izomed, etc. Regardless of the implant system, the following principles should be respected for implantation: indications and contraindications, biocompatibility, osseointegration, implant loading protocol, and evaluation of implant performance.
Indications for implantation are: loss of one or more teeth or total toothless, which practically means any dental deficiency. Indications include the lack of a part of the jawbone (retention of the opturator –post-resection dentures) and the lack of a part of the face (retention of facial dentures). Contraindications may be general and local, absolute and relative. Among the general contraindications include all systemic diseases (diabetes, vitamin D dependent rahitis, osteoporosis, autoimmune diseases, AIDS, malignant diseases, etc.) but also bad habits such as alcoholism, drug addiction, passionate smoking as well. It is mainly about relative contraindications if the disease is in the initial stages and under control while absolute contraindications, for example, fresh myocardial infarction, certain severe kidney and liver diseases, terminal stages of malignancies, air therapy or ongoing hemiotherapy. Local contraindications include tumors, infections, poor oral hygiene, para functions, restricted mouth opening, adverse inter-jaws relations, adverse anatomical relationships, etc. It’s a matter of relative contraindications while absolute contraindications are malignant tumors at the site intended for implantation, acute infections or significantly restricted mouth opening. Biocompatibility implies that the material from which the implants were built is in a harmony with the biological functions of living tissues as well as biologically inert. That mean interaction with living tissues is minimal and that the action of tissue fluids does not cause any change. Plasma titanium has been imposed as the material for the selection of modern implants which, in the highest percentage, satisfies the listed requirements [3]. Oseointegration implies direct structural and functional contact between the organized bone and the surface of the loaded implant. Implant loading protocol according to modern concepts can imply immediate, early and late loading. Immediate (immeasurable) burden implies setting temporary or final dental compensations within the first 48 hours after implantation. In relation to occlusion dental compensation may be out of service with antagonists or in full functional occlusion [4,5]. Early burden is the setting of dental compensation in a functional contact between 48 hours and three months after implantation. Late (conventional) burden implies the setting of dental compensation between three and six months after the implant is implanted whether it is a single phase protocol (the implant is mounted so that the soft tissue is adapted around its neck and it is in oral cavity with one part) or biphasic protocol (the implant is embedded so that it is completely covered with mucoperisotal cutting, its “release” to set “abatment” and load with dental compensation is the second phase) [6] (Figure 1-3).
Figure 1:
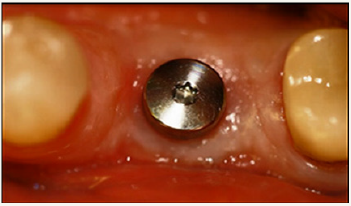
Figure 2:

Figure 3:

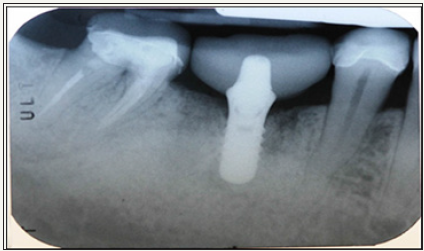
Assessment of the success of implants includes several criteria such as functional (vocabulary, speech), psychological (lack of pain, aesthetic result) and physiological. These criteria include the stability of the implants after removal of dental compensation, absence of radioluscence around the implant on the radiograph (Figure 4), vertical bone loss that is less than 2mm per year (after the first 12 months), absence of pain, infection, paraesthesia [7]. Treatment with implants is considered successful if 85% of implants after 5 years, or 80% after 10 years, meets the above criteria. The greatest challenges in modern implantology are implantation in difficult anatomical conditions and implantation in the arable area. Anatomical conditions that make it difficult to install common syringe implants represent a lack of alveolar bone (horizontal, vertical and combined) and reduced alveolar bone density. Modern implantology offers the following surgical procedures for solving anatomically difficult conditions: free autologous bone transplants alone or in combination with bone marrow and resorption or nonresorption membranes, alveolar distraction osteogenesis and basal osseointegration (BOI) disc implantation principles [8-10].
Figure 4:
Zygomatic implants are also one of the solutions of anatomically difficult conditions and are most commonly applied to the expressed atrophy of the alveolar ridge in the upper jaw and lowered sinuses (sinus procidens), which is mainly due to early loss of teeth, when a long period of time passes to adequate prosthetic care. Implantation in the treated area is performed in people with oral cancer. The treatment of malignant tumors of the maxillofacial region requires a team approach of doctors of several specialties. Of course, the most important thing is to radically remove the tumor and prevent its spread, which, like the reconstruction of the removed tissue is in the domain of maxillofacial surgeon. No less important is the application of air therapy after surgery, and in some cases also polihemiotherapy, which within a specific oncological treatment is performed by a radiologist or an oncologist [11,12]. The success rate of the implants in the ventilated area depends on the places in which they are implanted, the radiation dose received and the use of the hyperbaric chamber. The percentage of rejection of implants from the area of the face and jaw is quite large (30-40%), but with the use of a hyperbaric chamber that revitalizes the bone, it can be significantly reduced. In any case, it is advisable to wait for the implant for at least four months from the applied air therapy.
In the end, to summarize, the use of oral and extra oral implants is a modern and safe method (selection method) of fixation of dental compensations and dentures. In order for implantation to be successful, the following principles must be respected: indications and contraindications, biocompatibility, osseointegration, implant loading protocol, and evaluation of the success of implants. The major challenges in implantology are implantation in difficult anatomical conditions and implantation in the irradiated area, but they are not absolute contraindications. By making the right choice or applying adequate implantation systems, successful implantation is possible under different conditions.
References
- Misch CE (2005) Rationale for dental implants. In: Misch CE (Ed.), Dental Implant Prosthetics. St. Louis: Mosby, USA, pp. 6, 11-13, 15.
- Adell R, Lekholm U, Rockler B, Brånemark PI (1981) A 15 year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg 10(6): 387-416.
- Kasemo B (1983) Biocompatibility of titanium implants: Surface science aspects. J Prosthet Dent 49(6): 832-837.
- Brånemark PI (1983) Osseointegration and its experimental background. J Prosthet Dent 50(3): 399-410.
- Brånemark PI, Zarb GA, Albrektsson T (1985) Tissue integrated prosthesis: osseointegration in clinical dentistry. Quintessence Publishing Co, Chicago, USA, p. 11.
- Ihde SKA, Konstantinović VS (2005) Comparison and definition of the pathological phenomena occurring after a tooth replacement and possible therapeutic stages implying basal and crestal implants. Implantodontie 14: 176-185.
- Horinchi K, Uchida H, Yamamoto K, Sugimura M (2000) Immediate loading of Brånemark system implant following placement in edentulous patients: A clinical report. Int J Oral Maxillofac Implants 15(6): 824-830.
- Chin M (1999) Distraction osteogenesis in maxillofacial surgery. In: Lynch SE, Genco RJ, Marx RE (Eds.), Tissue Engineering, applications in maxillofacial surgery and periodontics. Quintessence Publishing Co, Inc. Chicago, Berlin, London, England, pp. 147-160.
- Chin M, Toth BA (1996) Distraction osteogenesis in maxillofacial surgery using internal devices: a review of five cases. J Oral Maxillofac Surg 54(1): 45-53.
- Gaggl A, Schultes G, Karcher H (1999) Distraction implants: a new technique for alveolar ridge augmentation. J Oral Maxillofac Surg 27(4): 214-221.
- Bischorer R, Schmelzle R (1997) Verwendung des Fibulaspans bei der Kieferkammaugmentation. Oral and Maxillofacial Surgery 1(1-6): 276- 280.
- Beumer J, Zlotolow IM, Sharma AB (1998) Restoration of palate, tongue mandible, and facial defects. In: Silverman S (Ed.), Oral cancer. BC Decker Inc, Hamilton, London, England, pp. 103-112.
© 2018 Mladen Vukovic. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






