- Submissions

Full Text
Modern Applications in Pharmacy & Pharmacology
The Effects of Socioeconomic Status on Contracting Rheumatic Fever: Case Reports
Charlie Colquitt*, Irenee Ibrahim, Jamekia Grant, Jasmine LaVine, Mario Ghattes and Nkechi Ikediobi
Florida Agricultural and Mechanical University, USA
*Corresponding author:Charlie Colquitt, Associate Professor of Pharmacy Practice, Florida Agricultural and Mechanical University, Florida, USA
Submission: February 19, 2018;Published: May 24, 2018
ISSN 2637-7756Volume2 Issue1
Abstract
The effects of socioeconomic status may cause mitral valve replacement due to rheumatic fever. Environmental and financial factors in an underserved community such as access to healthcare, overcrowding, household income, and health literacy may predispose individuals and increase their risk of acquiring infections. Two patients were identified and then interviewed in the midtown community in Saint Petersburg, Florida who received mitral valve replacements as the result of rheumatic fever. This is the study of two case reports outlining the progression of rheumatic fever leading to mitral valve replacements.
keywords:Rheumatic fever; Socioeconomic status; Mitral valve replacement; Mitral valve regurgitation; Rheumatic heart disease
Introduction
Acute rheumatic fever (ARF) is a nonpurulent inflammation that occurs as a result of group A Streptococcus (GAS) pharyngitis that can manifest as carditis and valvulitis (50-70% of cases), arthritis (35-66%), central nervous system involvement: Sydenham chorea (10-30%), subcutaneous nodules (0-10%), or erythema marginatum (less than 6%) [1]. Some minor manifestations of ARF include fever, prolonged PR interval, arthralgia, and elevated acute phase reactants (C-reactive protein [CRP], erythrocyte sedimentation rate [ESR] [2]. This case will focus on ARF’s most prevalent manifestation of carditis also known as rheumatic heart disease (RHD). RHD refers to the involvement of the endocardium exhibiting as valvulitis, especially of the aortic and mitral valves, and usually presents within three weeks from the original infection. It is usually diagnosed by echocardiographic evidence of aortic or mitral regurgitation and auscultatory findings. Auscultatory findings include the Carey Coombs murmur, which is an indicatory of moderate to severe mitral regurgitation due to increased blood flow across the mitral valve during left ventricular filling, and it characterized by a short mid-diastolic murmur that is heard the loudest at the apex [3]. Cardiac valve damage from rheumatic fever can be chronic and progressive, and eventually lead to cardiac decompensation which requires immediate and intensive treatment such as mitral valve replacement.
The purpose of this case report is to study and analyze the socioeconomic effects that may cause a patient to seek a mitral valve replacement due to contracting rheumatic fever. According to the Centers for Disease Control and Prevention (CDC), the prevalence of ARF in the United States is extremely low with approximately 0.04-0.06 cases per 1,000 children [4]. The reason the prevalence is so low in America is because this disease is one of economic disadvantage and poverty; in addition, the diagnosis and treatment of GAS pharyngitis has tremendously improved in America and other industrialized countries since the mid-20th century [5]. Some risk factors of ARF include: age (6-20 years old), family history, scarlet fever, poor sanitation, strep throat, overcrowded living conditions, and lack of access to health care [6,7].
At the Community Health Centers of Pinellas, Inc., an ambulatory care clinic designed to provide affordable and quality primary healthcare services to Pinellas County underserved individuals, two patients have received mitral valve replacement due to ARF [8]. With the extremely low occurrence of ARF, this case report aims to investigate why two patients have presented with this condition by evaluating their socioeconomic risk factors in the Mid-town community located in St. Petersburg, Florida.
Patient case presentation
A mother and son pair is both patients at the Community Health Centers of Pinellas, Inc. The mother is a 59-year old African American female (height, 172.72cm; weight, 92.6kg) who received mitral replacement (with a #27mm St. Jude Mechanical Valve) in 2010 due to severe mitral regurgitation secondary to rheumatic fever, which she has had for years. The patient as an outpatient underwent a cardiac catheterization which demonstrated normal coronary arteries, ejection fraction greater than 50% with mitral vegetation. She then subsequently underwent a transesophageal echocardiogram (TEE) showing a dilated left atrium, and left ventricular cavity was dilated with overall normal systolic function. The anterior mitral leaflet was found on the significant prolapse with a possibility of ruptured cord and it was felt to be some involvement of prolapse in the posterior leaflet as well. The regurgitant jet was tilted out to the left atrium. She also presented with shortness of breath, heart failure, and chest wall pain. In addition to the severe mitral regurgitation, her medical history also included hypertension, hyperlipidemia, and rheumatoid arthritis. She reported no known drug allergies. Her family history is inconclusive because she was adopted. The patient reported that she smokes 2 packs a day for the past 30 years, and occasional drinks alcohol. She denied any illicit drug use. The patient claimed she was disabled from her rheumatoid arthritis. Her home medications and dosages at the time of surgery are as follows: Ecotrin 81mg twice daily, Folic Acid 1mg daily, Methotrexate 15mg weekly, Motrin 600mg every 8 hours as needed, Tylenol 650mg every 6 hours as needed, Nexium 40mg daily, Prinivil 5mg daily, and Zocor 20mg daily. All medications were taken orally. The patient was discharged on the following medications: Tylenol 650mg by mouth every 6 hours as needed for pain, Zocor 20mg by mouth at bedtime, Methotrexate 50mg by mouth weekly on Monday, Colace 100mg by mouth twice daily, Aspirin 81mg by mouth daily, Lortab 5/325mg 1-2 tablets by mouth every 4 hours as needed for moderate pain, Nexium 40mg by mouth daily, Folic Acid 1mg by mouth daily, and Coumadin 5mg by mouth daily or as directed.
The son is a 31-year old African American male (height, 177.8cm, weight, 103.6kg) who received mechanical mitral replacement in 2015 due to mitral regurgitation secondary to rheumatic fever. The patient was diagnosed with rheumatic fever at the age of 7 and developed significant mitral valve thickening with severe restriction and consequently severe mitral regurgitation. His symptomatology consisted of shortness of breath only with heavy exertion. His mitral regurgitation was discovered whenever he was hospitalized for his first seizure in early 2015. He was told that a CT scan of the head was negative, and a subsequent MRI of the brain also did not demonstrate any anatomic abnormalities. However, it was his physical exam revealed a loud murmur in the heart and a subsequent echocardiogram was performed which demonstrated severe mitral regurgitation with no evidence of mitral stenosis. Aortic valve was trileaflet and function normally. There was severe tricuspid regurgitation. Subsequent left and right heart catheterization were performed which demonstrated normal coronary arteries and a dilated left ventricle with normal systolic function. His doctor speculated that his seizure disorder is not in any way related to his cardiac abnormalities. His past medical history at the time of surgery included mitral valve regurgitation, rheumatic fever, seizure disorder, drug abusetetrahydrocannabinol (THC), and paroxysmal atrial fibrillation. He reported no known drug allergies. His family history from his mother’s side is as mentioned above, and history from his father’s side is unknown. The patient’s social history includes smoking 5 cigarettes per day for 7 months, drinking alcohol occasionally, and abusing THC. His home medications and dosages at the time of surgery are as follows: Lisinopril 5mg by mouth daily and Coreg 3.125mg by mouth twice a day with food. The patient was discharged on the following medications: Amiodarone 200mg by mouth daily, Coreg 12.5mg by mouth twice daily, Coumadin 5mg by mouth once a day every Tuesday, Thursday, Saturday, and Sunday, and Coumadin 7.5mg by mouth once a day every Monday, Wednesday, and Friday, and Keppra 750mg by mouth twice daily.
Discussion
The purpose of this case report is to analyze the socioeconomic effects that may contribute to patient contracting rheumatic fever which could ultimately lead to a mitral valve replacement. In the Midtown community of Saint Petersburg, Florida the population is primarily of low socioeconomic status. This community accounts for 10% of Saint Petersburg’s population but the poverty rate is close to 30% vs St. Petersburg’s city poverty rate of less than 10%. Both patients in our case report reside in the Midtown area and they were interviewed to assess socioeconomic contributory risk factors. The questionnaire and the patients’ responses are recorded in Table 1.
Table 1: Patient questionnaire.
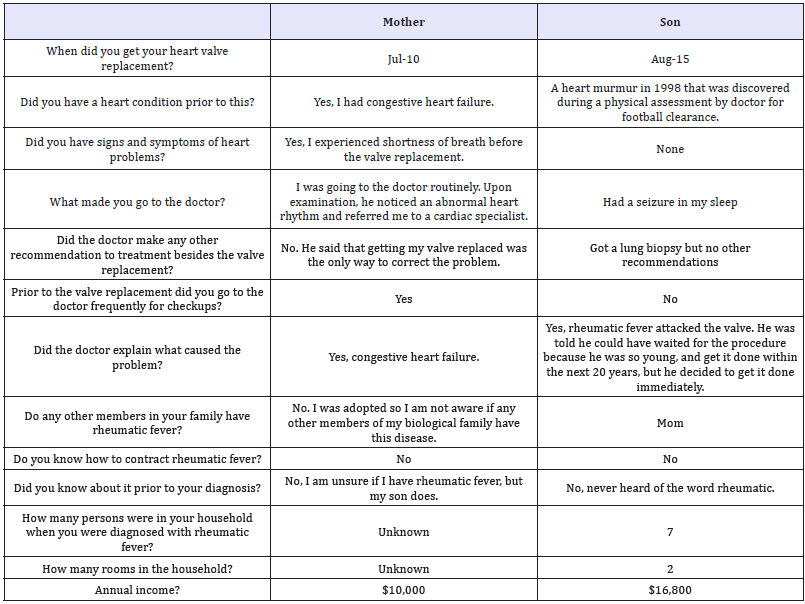
Conclusion
Based on the patients’ charts and responses from the questionnaire, they exhibit many of socioeconomic risk factors for developing ARF. Although the mother’s family history is unknown, the son had a direct relative who experienced heart complication due to ARF. When the son was first diagnosed with rheumatic fever, he was living in an overcrowded living space with 7 people sharing 2 bedrooms. However, since the mother is unsure when she contracted ARF (and her charts do not indicate it as well), it is unclear if she was also living in an overcrowded area at the time of diagnosis. Annual income at diagnosis was not assessed, but current annual income is useful when considering post-operative treatment. The mother falls under the individual poverty line of an annual income of $12,140. The son, at the time of surgery, did not have personal health insurance, and the doctor would not operate until he obtained it because of post-operative treatment costs. In addition, both patients live in the Midtown area of Pinellas County which is an underserved and has a substantially extreme poverty rate in comparison to the City of Saint Petersburg. Family history, overcrowded living conditions, health literacy and lack of access to health care all play a significant role in developing ARF, as witnessed by these patients.
References
- Gibofsky A, Steer A (2017) Acute rheumatic fever. In: TePas E (Ed.), Epidemiology and pathogenesis.
- Gibofsky A, Steer A (2017) Acute rheumatic fever. In: TePas E (Ed.), Clinical manifestations and diagnosis.
- Peters F, Zuhlke L (2018) Clinical manifestations and diagnosis of rheumatic heart disease. In: Yeon SB (Ed.).
- Beaudoin A, Edison L, Introcaso C, Goh L, Marrone J, et al. (2015) Acute rheumatic fever and rheumatic heart disease among children-American Samoa. MMWR Morb Mortal Wkly Rep 64(20): 555-558.
- Lee GM, Wessels MR (2006) Changing epidemiology of acute rheumatic fever in the United States. Clinical Infectious Diseases 42(4): 448-450.
- AARP (2017) Rheumatic fever risks
- Meadow R, Russell I (2017) Acute rheumatic fever.
- Community Health Centers of Pinellas. In: Mission (Ed.).
© 2018 Charlie Colquitt. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






