- Submissions

Full Text
Modern Approaches in Drug Designing
Comprehensive Pharmacology of Azithromycin Repurposing for COVID-19
Parthiba Ghosh1, Susmita Patra2, Susmita Roy1, Bipasha Mukherjee1, Pallab Kanti Haldar2 and Asis Bala1*
1Division of Pharmacology, Guru Nanak Institute of Pharmaceutical Science and Technology, 157/F Nilgunj Road, Panihati, Kolkata-700114, West Bengal, India
2Phytotherapy and Pharmacology Research Laboratory, Department of Pharmaceutical Technology, Jadavpur University, Kolkata – 700032, West Bengal, India
*Corresponding author: Asis Bala, Division of Pharmacology, West Bengal, India
Submission: July 30, 2021;Published: August 05, 2021
ISSN: 2576-9170 Volume3 Issue3
Abstract
The theory behind the madness of azithromycin for the treatment of COVID-19 is unclear as no significant evidences are available till date. The present study aimed to discuss about the comprehensive pharmacology of azithromycin and to explore the preclinical and clinical evidences repurposing for COVID-19. Here we reviewed briefly the current knowledge about COVID-19, considering the potential explanation for the repurpose of azithromycin for this pandemic disease condition and global crisis. Azithromycin alone or in combination with Hydroxychloroquine (HCQ) modulate the anti-inflammatory processes and decreases the susceptibility to secondary bacterial pneumonia. We highlighted potential approaches to address repurpose of azithromycin for COVID-19.
Keywords: Azithromycin; Comprehensive pharmacology; Repurposing for COVID-19; Immunomodulatory activity; Combination therapy for COVID-19
Introduction
Azithromycin is a well-known broad-spectrum antibiotic amongst the macrolide group,
primarily used for upper and lower respiratory tract infection [1]. Recently it is repositioned
for the treatment of covid-19 pandemic [1]. However, some circumstantial scientific reports
suggest that Azithromycin (AZ) in combination with hydroxychloroquine decrease the
viral load in Covid patients [2]. The open level non- randomized clinical trial carried out
by Gautret and co-workers stated that the patients treated with hydroxychloroquine and
azithromycin had 100% recovery rate after 5-6 days, compare to 57.1% of subjects treated
with hydroxychloroquine only, and 12.5% of untreated individuals [2]. There are some
controversies about the use of AZ in Coronavirus disease (COVID-19) [3-4]. This article
represents the research findings regarding the molecular pharmacology of AZ and how it is
correlated for the treatment of COVID-19.
The immunomodulatory and antiviral properties of AZ and other macrolides was
previously being established [5]. It is well known that coronavirus disease (COVID-19) is an
infectious disease caused by a newly discovered noble coronavirus [5]. Epithelial cells are the
primary target of this virus and Infection is mediated by cellular expression of Angiotensin-
Converting Enzyme 2 (ACE2), a carboxypeptidase that binds to the spike proteins of SARSCoV-
2; ACE2 is expressed by the epithelium of the mouth, tongue and upper airways, thus
enabling endocytosis of the virus [6]. Severity and mortality of COVID- 19 are associated with
host’s uncontrolled inflammatory response due to the hyper production of reactive oxygen
species and cytokines [7].
Macrolide antibiotics have promising activity against various respiratory viral disease
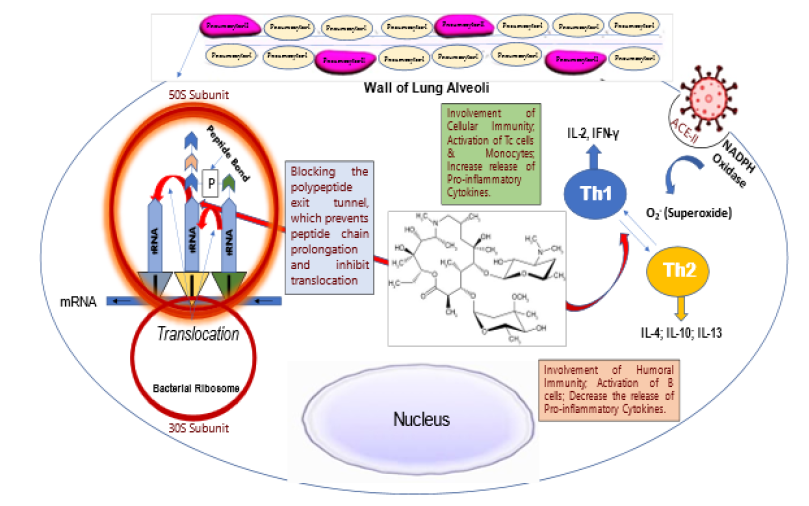
reported in different studies. Azithromycin significantly reduced inflammatory cytokines such as cytokines IL-6 and IL-8 and so far, increase the production of IFN
-gamma and IFN -gamma stimulated genes expression established
in Human bronchial epithelial cells in an in vitro condition [8]. AZ
favouring tissue repair after inflammation by shifting helper T cell
phenotype from type I to type II, reported by Murphy et al. [9] & [10].
Several studies have been reported about the anti-inflammatory
activities of AZ. AZ significantly reduced the production of proinflammatory
cytokines IL-12 and IL-6, increased production of
the anti-inflammatory cytokine IL-10 as shown in Figure 1; [11].
Preclinical research found that AZ attenuated the accumulation of
inflammatory cells in the lung tissue and significantly decreased
the aggregation of macrophages, lymphocytes and neutrophils [11].
Figure 1: The schematic representation of Azithromycin mechanism of action for inhibiting the viral translation and the possible way of explaining the immunomodulating role of Azithromycin.
CD147 is a transmembrane receptor glycoprotein, present
in host epithelial cell responsible for interaction with Covid-19
spike protein. Thus, it mediates the viral entry inside the host cell
[12]. CD147 also present in RBC and inflammatory cells used as
a receptor for parasite Plasmodium falciparum - protozoan that
causes Malaria in humans and also regulates cytokine secretion
and leukocytes chemotaxis. AZ interfere with the tight junction
formation between spike protein and CD147 and prevents virus
entry [13]. Previously it was reported that Az blocks the invasion
of Plasmodium falciparum in RBC. AZ reduces the expression
of CD147 reported by other studies. CD147 known as inducer of
extracellular matrix metalloproteinase, and CD147 functions as
an upstream stimulator of Matrix Metalloproteinases (MMP’s). AZ
exhibits reduced levels of MMP expression and activity, this may be
associated to a reduced expression of CD147 in cells [12-14].
COVID-19 considerably shows some higher mortality rate in
geriatric patients as it was reported that the highest mortality rate
was observed in patients aged ≥80 years. Patients aged >80 years
had 60% higher risk of dead compared to patients with age 70 to79
years [15]. It was also seen that patients aged eighty and older on
ventilators, the fatality rate was 90 percent [15,16]. This arise the
question is to whether there is any correlation between ageing
and COVID-19 infection. Cellular “senescence” defined as a state
in which cells cease dividing and undergo distinctive phenotypic
alterations, including profound chromatin and secretome
changes, and tumor-suppressor activation [17]. Senescence
occurs throughout the lifespan including during embryogenesis
and it plays very important role during development as well as
wound healing [17,18]. There are certain kinds of biomarkers like
CD26, ACE2 are express in senescent cell. Interestingly, these two
receptors are used by COVID-19 for entering into the cell. Senescent
cells produce large amounts of inflammatory cytokines, as a
result of the senescence-associated secretory phenotype (SASP),
including IL-6, increased protein synthesis, increased number of
lysosomes. Corona virus uses the machinery of this cell which find as ideal cell for their replication [18]. Azithromycin preferentially
targets senescent cells, removing approximately 97% of them with
great efficiency [19]. AZ also acts as an anti-inflammatory agent and
reduces SASP mediators such as IL-1 beta and IL-6. Interestingly Az
inhibits the replication of other viruses, such as Zika and Ebola [18-
21]. It can be predicted that senolytic agent can be useful for the
treatment of COVID-19. In clinical trial Az shows its efficacy against
Covid-19, combinely with Hydroxychloroquine may be due to its
senolytic activity. Although clinical trials are needed to establish
this hypothesis and repurposing efforts of Az against Covid-19
[21,22].
There are some in vitro evidence that AZ may prevent replication
of other viruses such as human influenza virus H1N1 and Zika virus.
AZ and hydroxychloroquine combinedly inhibit the replication of
SARS-CoVs 1 and 2 in in vitro, identified by Andreani et al. [23].
It was reported previously that AZ prevents the replication and
release of Rhinovirus (RV1B & RV16) [24,25].
Conclusion
The review briefly explained the current knowledge about COVID-19, considering the potential explanation for the repurpose of azithromycin. Azithromycin modulates the antiinflammatory processes by modulating the Th1 and Th2 cytokine level as mentioned schematically in Figure 1. and decreases the susceptibility to secondary bacterial pneumonia.
References
- Damle B, Vourvahis M, Wang E, Leaney J, Corrigan B (2020) Clinical pharmacology perspectives on the antiviral activity of azithromycin and use in COVID-19. Clin Pharmacol Ther 108(2): 201-211.
- Gautret P, Lagier JC, Parola P, Hoang VT, Meddeb L, et al. (2020) Hydroxychloroquine and azithromycin as a treatment of COVID-19: Results of an open-label non-randomized clinical trial. Int J Antimicrob Agents 56(1): 105949.
- Trindade GG, Caxito SMC, Xavier AREO, Xavier MAS, BrandÃo F (2020) COVID-19: Therapeutic approaches description and discussion. An Acad Bras Cienc 92(2): e20200466.
- Schögler A, Kopf BS, Edwards MR, Johnston SL, Casaulta C, et al. (2015) Novel antiviral properties of azithromycin in cystic fibrosis airway epithelial cells. Eur Respir J 45(2): 428-439.
- Bala A, Sengupta A, Matsabisa MG, Chabalala HP (2020) COVID-19: Pathophysiology; mechanism of transmission and possible molecular drug target for management. Curr Mol Pharmacol, PMID: 32867666.
- Schett G, Manger B, Simon D, Caporali R (2020) COVID-19 revisiting inflammatory pathways of arthritis. Nat Rev Rheumatol 16(8): 465-470.
- Huang C, Wang Y, Li X, Ren L, Zhao J, et al. (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395(10223): 497-506.
- Min JY, Jang YJ (2012) Macrolide therapy in respiratory viral infections. Mediators Inflamm, 649570.
- Pani A, Lauriola M, Romandini A, Scaglione F (2020) Macrolides and viral infections: focus on azithromycin in COVID-19 pathology. Int J Antimicrob Agents 56(2): 106053.
- Murphy BS, Sundareshan V, Cory TJ, Hayes D, Anstead MI, et al. (2008) Azithromycin alters macrophage phenotype. J Antimicrob Chemother 61(3): 554-560.
- Beigelman A, Mikols CL, Gunsten SP, Cannon CL, Brody SL, et al. (2010) Azithromycin attenuates airway inflammation in a mouse model of viral bronchiolitis. Respir Res 11(1): 90.
- Ulrich H, Pillat MM (2020) CD147 as a target for COVID-19 treatment: Suggested effects of azithromycin and stem cell engagement. Stem Cell Rev Rep 16(3): 434-440.
- Joshi S, Joshi M, Degani MS (2020) Tackling SARS-CoV-2: Proposed targets and repurposed drugs. Future Med Chem 12(17): 1579-1601.
- Zhao-Hui Zheng, Ding Wei, Zheng Zhang, Wen-Zhen Kang, Chun-Qiu Hao, et al. (2020) Meplazumab treats COVID-19 pneumonia: An open-labelled, concurrent controlled add-on clinical trial.
- Bonanad C, García-Blas S, Tarazona-Santabalbina F, Sanchis J, Bertomeu-González V, et al. (2020) The effect of age on mortality in patients with COVID-19: A meta-analysis with 611,583 Subjects. J Am Med Dir Assoc 21(7): 915-918.
- Powell T, Bellin E, Ehrlich AR (2020) Older adults and covid-19: The most vulnerable, the hardest hit. Hastings Cent Rep 50(3): 61-63.
- Van Deursen JM (2014) The role of senescent cells in ageing. Nature 509(7501): 439-446.
- Ozsvari B, Nuttall JR, Sotgia F, Lisanti MP (2018) Azithromycin and roxithromycin define a new family of "senolytic" drugs that target senescent human fibroblasts. Aging (Albany NY) 10(11): 3294-3307.
- Sargiacomo C, Sotgia F, Lisanti MP (2020) COVID-19 and chronological aging: Senolytics and other anti-aging drugs for the treatment or prevention of corona virus infection? Aging (Albany NY)12(8): 6511-6517.
- Bosseboeuf E, Aubry M, Nhan T, de Pina JJ, Rolain JM, et al. (2018) Azithromycin inhibits the replication of zika virus. J Antivir Antiretrovir 10: 6-11.
- Madrid PB, Panchal RG, Warren TK, Shurtleff AC, Endsley AN, et al. (2015) Evaluation of ebola virus inhibitors for drug repurposing. ACS Infect Dis 1(7): 317-326.
- Scherrmann JM (2020) Intracellular ABCB1 as a possible mechanism to explain the synergistic effect of hydroxychloroquine-azithromycin combination in COVID-19 therapy. AAPS J 22(4): 86.
- Andreani J, Le Bideau M, Duflot I, Jardot P, Rolland C, et al. (2020) In vitro testing of combined hydroxychloroquine and azithromycin on SARS-CoV-2 shows synergistic effect. Microb Pathog 145: 104228.
- Gielen V, Johnston SL, Edwards MR (2010) Azithromycin induces anti-viral responses in bronchial epithelial cells. Eur Respir J 36(3): 646-654.
- Saleh M, Gabriels J, Chang D, Soo Kim B, Mansoor A, et al. (2020) Effect of chloroquine, hydroxychloroquine, and azithromycin on the corrected QT interval in patients with SARS-CoV-2 infection. Circ Arrhythm Electrophysiol 13(6): e008662.
© 2021 Asis Bala. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






