- Submissions

Full Text
Modern Approaches in Drug Designing
Inflammation and Breast Cancer
Li Pin Kao1,2*
1Department of Basic Medical Sciences, Purdue University, USA
2Centre for Cancer Research, Purdue University, USA
*Corresponding author: Li Pin Kao, Department of Basic Medical Sciences, Centre for Cancer Research, Purdue University, West Lafayette, USA
Submission: February 23, 2018;Published: May 24, 2018
ISSN: 2576-9170
Volume2 Issue1
Abstract
Chronic inflammation is a critical factor in tumor progression. Adipocyte accumulation and cytokines storm during inflammation have a significant impact on breast cancer. The development of cancer arises from sites of infection, chronic irritation and inflammation. Furthermore, tumor seed in tumor microenvironment as seed and soil, orchestrated by inflammatory cells, is an indispensable for cells transformed into benign or malignancy status and further fostering proliferation, survival, and migration. These insights are fostering new anti-inflammatory therapeutic approaches to cancer development
Keywords: Breast Cancer; Inflammation; Obesity
Introduction
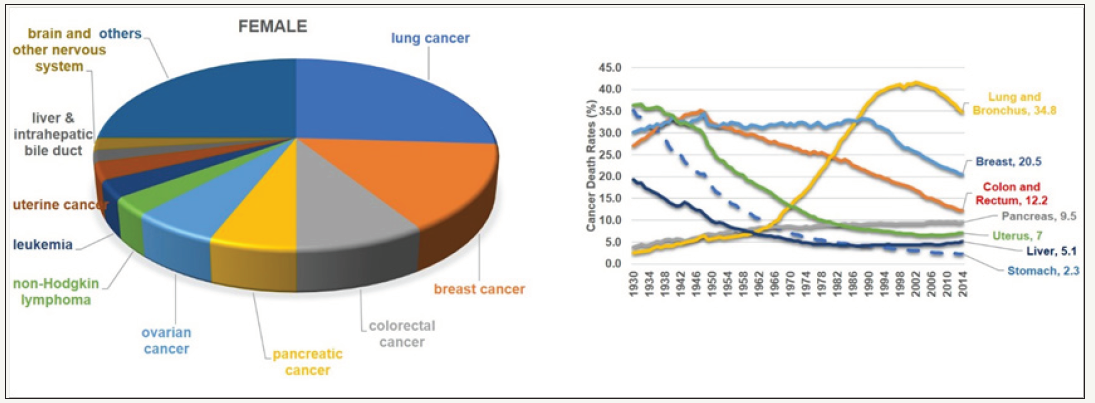
Breast cancer (BC), the first most common malignant tumor in women worldwide (Figure 1) [1]. Many etiological factors such as a wide spectrum of clinical manifestations caused by family clustering, hormonal factors, lactation, early menarche, metabolic and secretory factors, obesity, dietary factors, alcohol consumption, smoking, and lose-dose irradiation [2]. On top of that, obesity, alcoholism, and tobacco smoking were found to result in this incidence [3-6]. Many of the established risk factors are linked to estrogens. Risk is increased by early menarche, late menopause, and obesity in postmenopausal women, and prospective studies have shown that high concentrations of endogenous estradiol are associated with an increase in risk [7].
figure 1: The Overview of the Proportional of different type of Cancers in Female.
Childbearing reduces risk, with greater protection for early first birth and a larger number of births; breastfeeding probably has a protective effect. Both oral contraceptives and hormonal therapy for menopause cause a small increase in breast-cancer risk, which appears to diminish once use stops. Alcohol increases risk, whereas physical activity has been suggested as protective. Mutations in certain genes greatly increase breast cancer risk, but these account for a minority of cases.
The natural therapeutic (i.e. nutritional supplements) are still discovering in progress to prevent the unnecessary aggressive procedures, although there are many FDA-approval drugs for breast cancers [8,9]. Tumors are heterogenous and individual has inherited different genetic background. Thus, it is hard to find an effective treatment and it may recurrent after recovery from first treatment.
Obesity accelerate the worse the breast cancer
The proportion of obesity has been distributed various within United State (Figure 2). Obesity is known as a key contributory factor associated with cancer risk and mortality. Obesity has resulted increase cells accumulated lipids and slowly differentiated into mature adipocytes. Study also demonstrated that adipocytes are released chemokines to attract Eosinophils and monocytes which release cytokine (interleukin-4, 5, -13, and TNFα) which resulted in helminth immunity, activated macrophages associated with glucose homeostasis [10]. Moreover, other study had demonstrated that adipocytes associated lung neutrophilia and subsequent exacerbate the stimulatory effects of a primary tumor on neutrophils and further enhanced metastatic seeding [11].
figure 2: Distribution of Obesity within United State.
A. Adult obesity prevalence maps Prevalence of Self-reported Obesity among Non-Hispanic white Adults by State and Territor
B. Pie chart of 4 main regions.
C. Bar graph of the Proportion of Obesity within each Region.
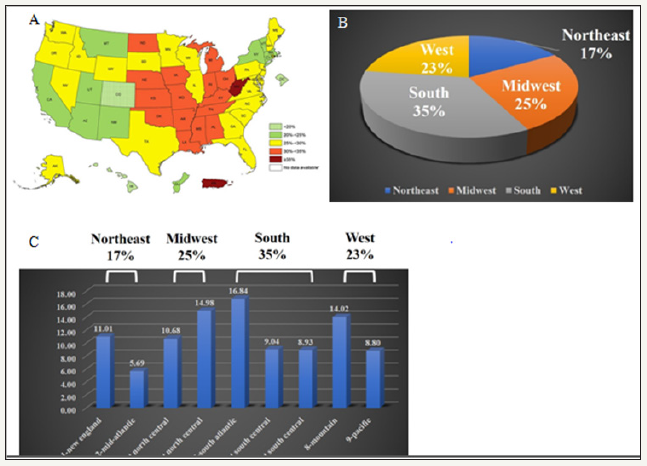
figure 3: The process of cellular transformation into malignancy.
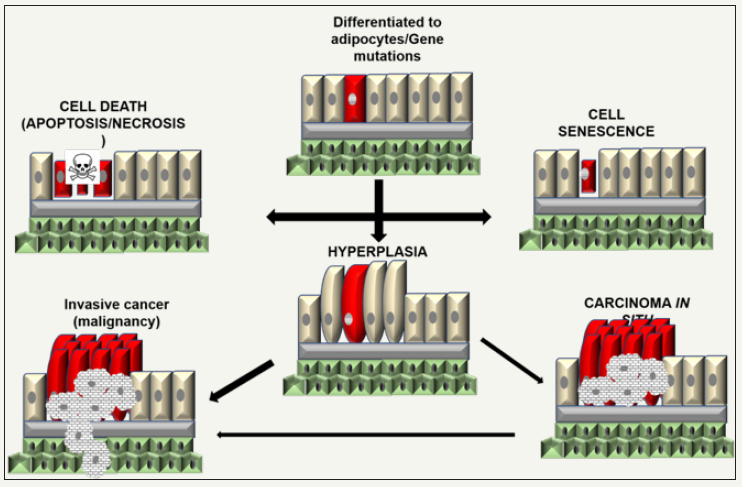
Obesity produces an inflammatory state, characterized by macrophages clustered around enlarged hypertrophied, dead, and dying adipocytes from crown-like structures. There are two different types of adipocytes (white or brown). They have different metabolic demands. Due to adipocytes size and taken over the reasonable space, tissues may damage and slow recovery due to chronic inflammation damage which potentially decreases cell proliferation and increases tissue damage. This abnormal condition results in an increase in fibrous tissue and further leads to the development of cancer [12]. Adipocytes have been suggesting as a major factor in provide as seed and soil to manipulate the microenvironments, may differentiated the normal cells toward to malignancy status (Figure 3). Thus, adipocytes may contribute significant to inflammation, immunity, extracellular matrix mechanics, epigenetic or transcriptional regulation, and protein translation in cancers.
Moreover, inflammatory breast cancer (IBC) is a rare, but aggressive type of locally advanced breast cancer. The great portion of IBC cases are also triple negative (TN) patients. The signs of IBC often appear faster than other type of BC, such as redness and swelling which often first treated with antibiotics. Due to the lack of breast lump and symptoms, IBC often misdiagnosis or miss the best treatment time frame. Most of patients with IBC have advanced-stage disease by the time they begin treatment. The inflammation recruits immune cells which release the cytokines and chemokines which provide seed and soil microenvironment to facilitate metastasis such as Epithelial to Mesenchymal transition (EMT) [13-15].
Thus, it is it important to increase our understanding of how IBC can be better diagnosed and how biology drives its progression which can leads to improve diagnosis, prognosis with more effective treatment for those with this aggressive disease.
Disclosure of potential conflicts of Interest
The author indicates no potential conflict of interest.
Acknowledgement
The author would like to acknowledge the financial support of the Purdue University for provided support in the form of salaries of KLP listed but did not have any additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- Siegel RL, KD Miller, A Jemal (2017) Cancer Statistics. CA Cancer J Clin 67(1): 7-30.
- Key TJ, GK Reeves (2016) Alcohol diet and risk of breast cancer. BMJ 353: i2503.
- Kerr J, C Anderson, SM Lippman (2017) Physical activity sedentary behaviour diet and cancer: an update and emerging new evidence. Lancet Oncol 18(8): e457-e471.
- Macacu A (2015) Active and passive smoking and risk of breast cancer: a Meta analysis. Breast Cancer Res Treat 154(2): 213-224.
- Calle EE (2003) Overweight obesity and mortality from cancer in a prospectively studied cohort of US adults. N Engl J Med 348(17): 1625- 1638.
- Key TJ (2004) Diet nutrition and the prevention of cancer. Public Health Nutr 7(1A): 187-200.
- Key TJ (2002) The effect of diet on risk of cancer. Lancet 360(9336): 861-868.
- Shui IM (2015) Circulating vitamin D vitamin D-related genetic variation and risk of fatal prostate cancer in the National Cancer Institute Breast and Prostate Cancer Cohort Consortium. Cancer 121(12): 1949-1956.
- Bakker MF (2016) Plasma carotenoids, vitamin C, tocopherols, and retinol and the risk of breast cancer in the European Prospective Investigation into Cancer and Nutrition cohort. Am J Clin Nutr 103(2): 454-464.
- Wu D (2011) Eosinophils sustain adipose alternatively activated macrophages associated with glucose homeostasis. Science 332(6026): 243-247.
- Quail DF (2017) Obesity alters the lung myeloid cell landscape to enhance breast cancer metastasis through IL5 and GM CSF. Nat Cell Biol 19(8): 974-987.
- Sanyal AJ, SK Yoon, R Lencioni (2010) The etiology of hepatocellular carcinoma and consequences for treatment. Oncologist 15 Suppl 4: 14- 22.
- Jolly MK (2017) Inflammatory breast cancer: a model for investigating cluster based dissemination. NPJ Breast Cancer 6(3): 21.
- DeNardo DG, LM Coussens (2007) Inflammation and breast cancer Balancing immune response: crosstalk between adaptive and innate immune cells during breast cancer progression. Breast Cancer Res 9(4): 212.
- Morrow RJ (2017) Challenging a Misnomer? The Role of Inflammatory Pathways in Inflammatory Breast Cancer. Mediators Inflamm.
© 2018 Li Pin Kao. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






