- Submissions

Full Text
Journal of Biotechnology & Bioresearch
A Systematic Overview of Bioelectronic Medicine and its Impact on Medical Technology
Mahfuzul Islam*
Daffodil International University, Bangladesh
*Corresponding author: Mahfuzul Islam, Daffodil International University, Bangladesh
Submission: February 02, 2022;Published: March 23, 2022

Volume3 Issue4March, 2022
Abstract
The field of medicine has already benefited significantly from technological innovation. One of these developments is Bioelectronic Medicine (BME), which combines molecular medicine, neuroscience, engineering, and computing to create a device capable of diagnosing and treating disorders. Numerous scientific web data sources were gathered and analyzed for this study to produce useful and practical results. Although BMEs are used to treat over twenty diseases, this study focuses on five difficult conditions: paralysis, diabetes, rheumatoid arthritis, CNS problem and injury, and hypertension, as well as their notable BME treatment outcomes. Small, implantable devices that can be linked to a specific nerve can decode and modify neural signaling patterns, resulting in therapeutic effects specific to an organ’s signal characteristic without potentially dangerous drugs. Thousands of clinical trials and studies have been conducted on animal models and humans with the goal of neuromodulation, such as cracking, reading, and regulating ‘Vegas nerve’ signals to treat paralysis or the closed-loop bioelectronic device known as the intermittent vagal blocker for diabetic management, among others. Additionally, there have been remarkable and positive outcomes. These discoveries could be applied to the development of more effective treatments for several ailments.
Keywords: Bioelectronic Medicine; Neuromodulation; Hypertension; Rheumatoid arthritis; Diabetic; Paralysis; Central Nervous System; Vagus nerve; Stimulation; Regulation; Treatment
Introduction
Bioelectronic Medicine is evolving rapidly, and this is an exciting time to be involved. Continuous innovative preclinical research and development enables the investigation of novel diagnostic and therapeutic approaches in inflammatory and autoimmune illnesses, paralysis, and diabetes, among other conditions. This discipline encompasses material science, organic chemistry, biophysics, atomic Medicine, neuroscience, immunology, bioengineering, electrical, mechanical, and software engineering, mathematics, and computerized reasoning, as well as other essential and therapeutic disciplines [1]. Bioelectronic Medicine aims to advance our understanding of the diagnosis and treatment of infections and diseases such as cancer, rheumatoid joint pain, incendiary internal illness, obesity, diabetes, arthritis, loss of motion, visual impairment, ischemia, organ transplantation, cardiovascular disease, neurodegenerative diseases, and mortality. Bioelectronic Medication is based on electrical motions in the sensory system. Its primary focus is on incorporating information into the administrative parts of the sensory system, as well as advancements that record, stimulate, or inhibit neurological movements to alter specific molecular devices. Bioelectronic technologies are largely used to monitor and control natural cycles, acquire insight into host and microbe physiology and illness etiology, restore musculoskeletal capability and adaptability, and treat mobility loss and other important diseases. Across the globe, innovative preclinical and clinical preliminaries exploring novel diagnostic and therapeutic breakthroughs are being conducted. Bioelectronic Medication encourages contributions from various disciplines, including research, innovation, and medical services, on topics such as concepts, local community impact, administrative and legal implications, and patient criticism. Thus, bioelectronics is a future job, with enormous potential for the general public, as electronics are extremely costeffective when mass-produced. By substituting electrons for pharmaceuticals, that concept represents a significant leap forward in therapeutic safety and efficacy [1,2].
Components of BME
Interfaces are required in bioelectronic medicine to gain access to the following neural systems:
Electrodes
Complementary metal oxide semiconductors, penetrating electrodes made of silicon, fine, life, time, and cuff electrode arrays made of polymers, and so on. Platinum, platinum-iridium, gold, noble metals, alloys, laser-patterned, and others.
Polymers Include Polydimethyl Siloxane (PDMS), polyimide, parylene, fluidized crystal polymer, SU-8 photoresist, sheet or film polyimide, and polyurethane.
Lights
Diodes that emit light for optogenetic stimulation and energy transfer devices such as inductors, antennas, and ultrasonic transducers [3].
Treatment of hypertension with bioelectronic medicine
Antihypertensive pharmacotherapy is successful only to a degree. A significant proportion of patients have blood pressure readings over the guidelines while being treated with at least three medications at maximally tolerated doses, a condition known as resistant hypertension. The sympathetic nervous system is a good homeostatic mechanism for changing hemodynamics during stress or illness. Regrettably, in certain circumstances, this process escapes the carotid sinus’s physiologic regulation, resulting in resistant hypertension via various mechanisms [3]. A carotid sinus lead and a pulse generator comprise the system for giving baroreflex activation therapy in hypertension (Barostim neo system, CVRx, Inc., Minneapolis, Minnesota). The lead has a 40cm lead body that terminates in a circular backer 41 with a 2.0mm iridium oxide– coated platinum–iridium disk electrode. Like how a pacemaker is implanted, a subcutaneous infraclavicular chest wall pocket is formed to fit the pulse generator. The carotid sinus is surgically exposed before the electrodes being placed via a transverse cervical incision over the carotid bifurcation. Sensitivity is determined by observing hemodynamic changes associated with acute baroreflex activation, such as decreases in pulse rate or blood pressure due to increased parasympathetic or decreased sympathetic traffic, or both. After determining the precise location of the electrode, six sutures are introduced through the backer and adventitia in a regular pattern around the perimeter of the electrode backer.
The opposite end of the lead is inserted into the pulse generator pocket through a subcutaneous tube and connected to the pulse generator. Finally, the surgery is completed by closing all incisions. In the absence of side effects such as an increased heart rate or a reduction in blood pressure, treatment is initiated with a low dose [3-6].
Methodology
Pre-planning
Bioelectronics is a word that has become more often used in recent years to refer to this multidisciplinary field. Progress is expected in all of these sectors for innovation in cross-cutting areas such as measurement and characterization of physiologic regions and neuromodulation. Unlike in previous ages, scientific research is routinely conducted as part of an education program in all countries. As a result, scientists have written thousands of publications. As a result, it was determined to review this emerging subject.
Process of data collection
Due to the ongoing global epidemic, several countries have reported lockdowns, complicating physical data collecting. As a result, it was agreed that data would be gathered over the internet. Google Scholar, Research-Gate, and PubMed search engines were used to gather information. Numerous documents, articles, and paper works on websites were assembled and important information. Several web resources were consulted to obtain an useable outcome. Priority was given to information gathered over the last decade through inquiries and clinical trials. Additionally, necessary data were gathered and analyzed from earlier investigations. Bioelectronic medicine, neuromodulation, hypertension, rheumatoid arthritis, diabetes, central nervous system disorders, and paralysis were used as search terms to locate information on the internet.
Results
We focused on five conditions (hypertension, rheumatoid arthritis, common CNS diseases, diabetes mellitus, and paralysis) in this study and used revolutionary bioelectronic medicine therapy strategies.
Bioelectronic medicine in hypertension
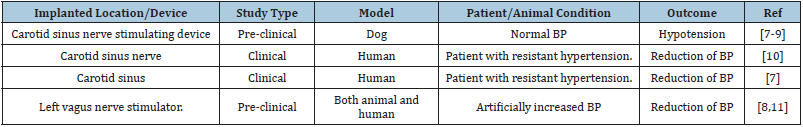
Neurostimulation with bioelectronic medicine, which involves electrical stimulation of the carotid sinus nerve (Hering’s nerve) or the carotid sinus itself to reduce blood pressure, is a last-resort option for treating a patient’s condition when drug-resistant hypertension medication or surgical procedures are either impossible or impractical. To lower blood pressure, people have used electrical stimulation of the carotid sinus nerve (Hering’s nerve) or the carotid sinus itself, and both animals and humans have studied Left Vagus Nerve Stimulation (LVNS) with positive and adequate results [7,8] Table 1.
Table 1: Highlights of researches on the use of neural feedback signals in nerve stimulation for the treatment of hypertension using bioelectronic medicine.
Bioelectronic medicine in Rheumatoid Arthritis (RA)
Numerous studies have demonstrated that the vagus nerve has the ability to control the immune system and decrease inflammation in both viral and inflammatory disorders [8-11]. Cervical vagal stimulation has been proven in a growing number of trials to effectively control experimental and clinical arthritis, particularly in persons who are resistant to traditional antirheumatic medications [12-20] Tables 2 & 3.
Table 2: Highlights of studies and bioelectronic devices that have showed optimistic consequences in preclinical or clinical trials in both in vivo and in vitro models to reduce inflammatory or pro-inflammatory cytokine levels in the treatment of RA.
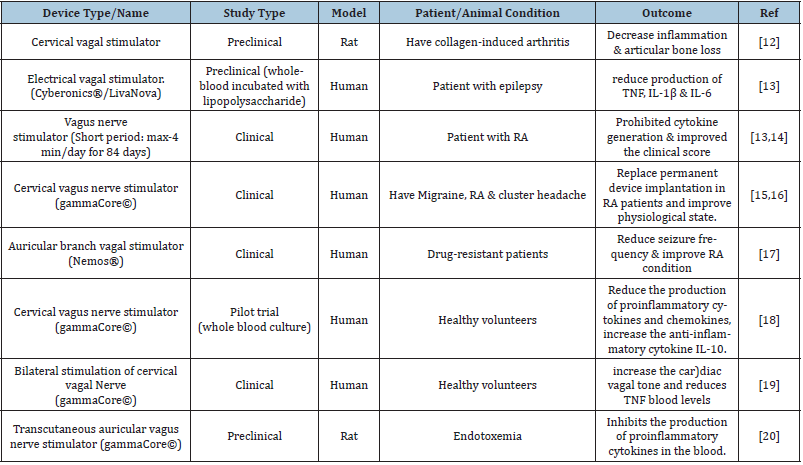
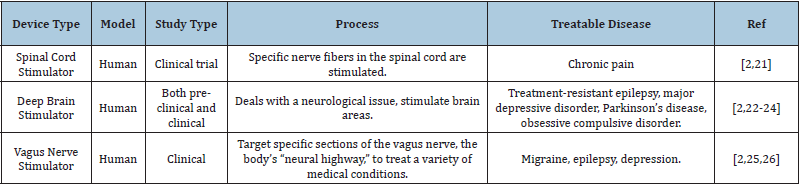
Table 3: Some recently treatable CNS disease with BME.
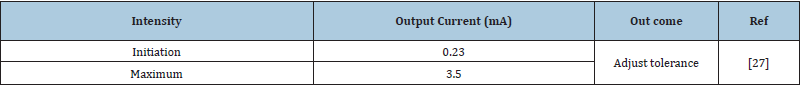
Bioelectronic medicine in CNS disease
After implantation, CNS therapy can begin with a low dose of stimulation [21-27]. Gradually stimulation is increased that listed on Table 4.
Table 4: CNS stimulation intensity of BME.
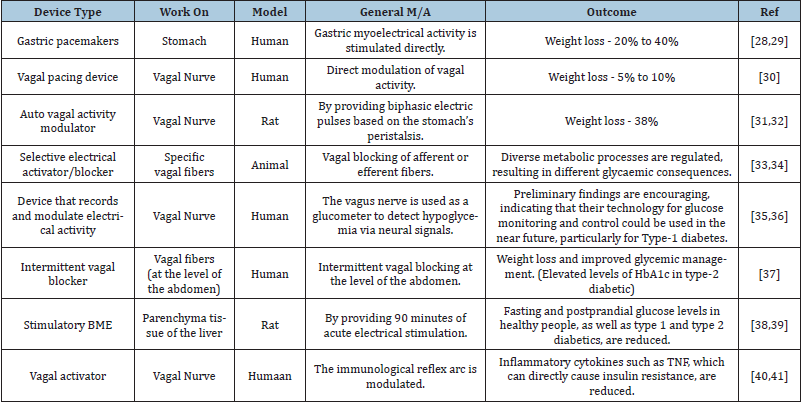
Bioelectronic medicine in Diabetes Mellitus (DM)
Due to the fact that diabetes is a metabolic disease, it can be handled in a variety of ways, including weight loss, metabolic management, glucose utilization or glycemic control, lowering insulin resistance, and modifying insulin activity in the body [28- 41]. BME also focuses on these areas when it comes to managing diabetes Table 5.
Table 5: DM management in several ways that applied CL-BME and neuromodulation.
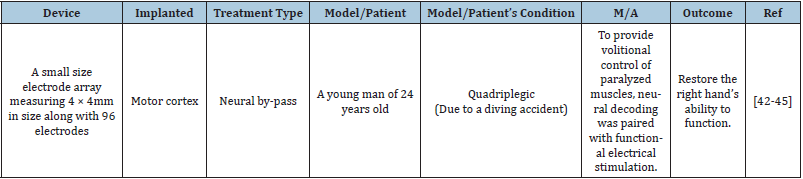
Bioelectronic medicine in paralysis
Decades of research into how movement information is stored in the brain, as well as the development of chronic neural interfaces and neural decoding methods, have paved the way for neural bypass technology in bioelectronics [42-45] Table 6.
Table 6: Consequence of BME in treatment of paralysis.
Conclusion
We make a few observations about the recent content of Bioelectronic Medicine, which covered several critical aspects of the field’s current state. In bioelectronic medicine, it is critical to focus on how information is encoded and how different brain networks are associated. Numerous investigations and laboratory or clinical experiments on neural decoding (understanding the language of the human nervous system) and functional connectivity mapping have been done, and numerous others are now underway. For instance, developing closed-loop methods and equipment adds a control system to an already vast and complicated control system, such as the human nervous system, which treats diabetes and hypertension. Concentrating on the transfer, storage, and connectivity of information would be critical in bioelectronic medicine for the treatment of paralysis, obesity, and other CNS illnesses such as epilepsy or migraine. We will have a greater understanding of the neurological system in the distant future if we can record, study, and interpret these signals to treat disorders with bioelectronic therapy that does not include any painful drug processes.
References
- Pavlov VA, Tracey KJ (2019) Bioelectronic medicine: Updates, challenges and paths forward. Bioelectron Med 5: 1-4.
- Alliance for Advancing Bioelectronic Medicine (2020) Building a bioelectronic medicine movement 2019: Insights from leaders in industry, academia, and research. Bioelectronic Medicine 6: 1-11.
- Patel DA, Chaudhary S (2020) Bioelectronic medicines: Innovation in disease treatment. International Journal of Pharmaceutical Sciences and Research 11(9): 4229-4237.
- Bakris GL, Nadim MK, Haller H, Lovett EG, Schafer JE, et al. (2012) Baroreflex activation therapy provides durable benefit in patients with resistant hypertension: Results of long-term follow-up in the rheos pivotal trial. J Am Soc Hypertens 6(2): 152-158.
- Sevcencu C, Nielsen TN, Struijk JJ (2017) A neural blood pressure marker for bioelectronic medicines for treatment of hypertension. Biosens Bioelectron 98: 1-6.
- Oparil S, Schmieder RE (2015) New approaches in the treatment of hypertension. Circ Res 116(6): 1074-1095.
- Sevcencu C, Struijk JJ (2018) Neural markers and implantable bioelectronic systems for the treatment of hypertension. Bioelectronics in Medicine 1(2): 139-150.
- Nielsen TN, Struijk JJ, Sevcencu C (2017) Stimulation waveforms for the selective activation of baroreceptor nerve fibers in the cervical vagus nerve. Converging Clinical and Engineering Research on Neurorehabilitation Springer International Publishing, New York, USA, pp. 995-999.
- Warner, Homer R (1958) The frequency-dependent nature of blood pressure regulation by the carotid sinus studied with an electric analog. Circ Res 6(1): 35-40.
- Schwartz SI, Griffith LS, Hagfors N (1967) Chronic carotid sinus nerve stimulation in the treatment of essential hypertension. Am J Surg 114(1): 5-15.
- Plachta DTT, Gierthmuehlen M, Cota O, Espinosa N, Boeser F, et al. (2014) Blood pressure control with selective vagal nerve stimulation and minimal side effects. Journal of neural engineering 11(3): 036011.
- Levine YA, Koopman FA, Faltys M, Caravaca A, Bendele A, et al. (2014) Neurostimulation of the cholinergic anti-inflammatory pathway ameliorates disease in rat collagen-induced arthritis. PloS one 9(8): e104530.
- Koopman FA, Chavan SS, Milijko S, Grazio S, Sokolovic S, et al. (2016) Vagus nerve stimulation inhibits cytokine production and attenuates disease severity in rheumatoid arthritis. Proc Natl Acad Sci USA 113(29): 8284-8289.
- Suzuki K, Nakai A (2018) Immune modulation by neuronal electric shock waves. J Allergy Clin Immunol 141(6): 2022-2023.
- Mwamburi M, Liebler EJ, Tenaglia AT (2017) Review of non-invasive vagus nerve stimulation (gammaCore): Efficacy, safety, potential impact on comorbidities, and economic burden for episodic and chronic cluster headache. Am J Manag Care 23(17Suppl): S317-S325.
- Simon B, Blake J (2017) Mechanism of action of non-invasive cervical vagus nerve stimulation for the treatment of primary headaches. Am J Mana Care 23(17Suppl): S312-S316.
- Stefan H, Kreiselmeyer G, Kerling F, Kurzbuch K, Rauch C, et al. (2012) Transcutaneous Vagus Nerve Stimulation (t‐VNS) in pharmacoresistant epilepsies: A proof of concept trial. Epilepsia 53(7): e115-e118.
- Lerman I, Hauger R, Sorkin L, Proudfoot J, Davis B, et al. (2016) Noninvasive transcutaneous vagus nerve stimulation decreases whole blood culture‐derived cytokines and chemokines: a randomized, blinded, healthy control pilot trial. Neuromodulation 19(3): 283-290.
- Brock C, Brock B, Aziz Q, Moller HJ, Jensen MP, et al. (2017) Transcutaneous cervical vagal nerve stimulation modulates cardiac vagal tone and tumor necrosis factor‐alpha. Neurogastroenterol Motil 29(5): e12999.
- Zhao YX, Wei H, Jing XH, Liu JL, Rong PJ, et al. (2012) Transcutaneous auricular vagus nerve stimulation protects endotoxemic rat from lipopolysaccharide-induced inflammation. Evid Based Complement Alternat Med 2012: 627023.
- Hayek SM, Veizi E, Hanes M (2015) Treatment‐limiting complications of percutaneous spinal cord stimulator implants: a review of eight years of experience from an academic center database. Neuromodulation 18(7): 603-609.
- Zangiabadi N, Ladino LD, Sina F, Orozco JP, Carter A, et al. (2019) Deep brain stimulation and drug-resistant epilepsy: A review of the literature. Front Neurol 10: 601.
- Shen HH (2019) Core concept: Can deep brain stimulation find success beyond Parkinson’s disease? Proc Natl Acad Sci USA 116(11): 4764-4766.
- Sankar T, Tierney TS, Hamani C (2016) Novel applications of deep brain stimulation. Surg Neurol Int 3(Suppl 1): S26.
- Cecchini AP, Mea E, Tullo V, Curone M, Franzini A, et al. (2009) Vagus nerve stimulation in drug-resistant daily chronic migraine with depression: Preliminary data. Neurol Sci 30(Suppl 1): S101-S104.
- Beekwilder, J. P., and T. Beems (2010) Overview of the clinical applications of vagus nerve stimulation. J Clin Neurophysiol 27(2): 130-138.
- Magkos F, Yannakoulia M, Chan JL, Mantroz CS (2009) Management of the metabolic syndrome and type 2 diabetes through lifestyle modification. Annu Rev Nutr 29: 223-256.
- Greenway F, Zheng J (2007) Electrical stimulation as treatment for obesity and diabetes. J Diabetes Sci Technol 1(2): 251-259.
- Cha R, Marescaux J, Diana M (2014) Updates on gastric electrical stimulation to treat obesity: Systematic review and future perspectives. World J Gastrointest Endosc 6(9): 419.
- Burneo JG, Faught E, Knowlton R, Morawetz R, Kuzniecky R (2002) Weight loss associated with vagus nerve stimulation. Neurology 59(3): 463-464.
- Yao G, Kang L, Li J, Long Y, Wei H, et al. (2018) Effective weight control via an implanted self-powered vagus nerve stimulation device. Nature communications 9(1): 1-10.
- Apovian CM, Shah SN, Wolfe BM, Ikramuddin S, Miller CJ, et al. (2017) Two-year outcomes of vagal nerve blocking (vBloc) for the treatment of obesity in the ReCharge trial. Obes Surg 27(1): 169-176.
- Meyers EE, Kronemberger A, Lira V, Rahmouni K, Stauss HM, et al. (2016) Contrasting effects of afferent and efferent vagal nerve stimulation on insulin secretion and blood glucose regulation. Physiological reports 4(4): e12718.
- Johnson RL, Wilson CG (2018) A review of vagus nerve stimulation as a therapeutic intervention. J Inflamm Res 11: 203-213.
- Gonzalez AG, Etienne-Cummings R, Georgiou P (2020) Closed-loop bioelectronic medicine for diabetes management. Bioelectronic Medicine 6: 1-7.
- Masi, Emily Battinelli, et al (2019) Identification of hypoglycemia-specific neural signals by decoding murine vagus nerve activity. Bioelectron Med 5(1): 1-10.
- Shikora S, Toouli J, Herrera MF, Kulseng B, Zulewski H, et al. (2013) Vagal blocking improves glycemic control and elevated blood pressure in obese subjects with type 2 diabetes mellitus. J Obes 2013: 245683.
- Chen J, Yin J, Lin L, Pasricha PK, Chen J (2009) T1810 Hepatic electrical stimulation reduces blood glucose in both type-I and type-II diabetic rats. Gastroenterology 136(5): A584-A585.
- Chen J, Pasricha PJ, Yin J, Lin L, Chen DZ (2010) Hepatic electrical stimulation reduces blood glucose in diabetic rats. Neurogastroenterol Motil 22(10): 1109-e286.
- Chang EH, Chavan SS, Pavlov VA (2019) Cholinergic control of inflammation, metabolic dysfunction, and cognitive impairment in obesity-associated disorders: Mechanisms and novel therapeutic opportunities. Front Neurosci 13: 263.
- Nathalie E, Paquot N, Scheen AJ (2015) Anti-inflammatory agents to treat or prevent type 2 diabetes, metabolic syndrome and cardiovascular disease. Expert Opin Investig Drugs 24(3): 283-307.
- Bouton C (2017) Cracking the neural code, treating paralysis and the future of bioelectronic medicine. J Intern Med 282(1): 37-45.
- Bouton CE (2019) Restoring movement in paralysis with a bioelectronic neural bypass approach: Current state and future directions. Cold Spring Harb Perspect Med 9(11): a034306.
- Bouton CE, Shaikhouni A, Annetta NV, Bockbrader MA, Friedenberg DA, et al. (2015) Restoring cortical control of functional movement in a human with quadriplegia. Nature 533: 247-250.
- Bouton C (2015) Neural decoding and applications in bioelectronic medicine. Bioelectronic Medicine 2(1): 20-24.
© 2022 Mahfuzul Islam. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






