- Submissions

Full Text
Innovation in Tissue Engineering & Regenerative Medicine
Radiotherapy for Wound Treated with BTM: A Case Report and Review of Literature
L Sun, S Cox and Ek Tan*
Department of Plastic and Reconstructive Surgery, New Zealand
*Corresponding author:EK Tan, Department of Plastic and Reconstructive Surgery, New Zealand
Submission: July 16, 2021;Published: September 15, 2021
Volume1 Issue4September , 2021
Abstract
Biodegradable Temporizing Matrix (BTM) is a synthetic absorbable scaffold dressing that facilitates rapid growth of granulation tissue when laid on a vascular wound bed. Radiation is often known to hinder the regenerative potential of soft tissues due to early effects of the induction of apoptotic cell death and late effects of dysregulated collagen deposition due to damaged fibroblasts. There are no established results on the use of radiation following BTM integration and whether taken grafts layered on top of BTM are adversely affected or buffered from the damage of radiation due to the robust granulation layer underneath. Here, we present a case where a staged approach of BTM and split skin graft reconstruction have led to a cosmetically favorable result, without skin graft breakdown following adjuvant radiation.
Introduction
The survival of biodegradable temporizing matrix (BTM) after radiotherapy is largely unknown. This is a case report of the survival of a left preauricular wound in an 82-year man who was treated with BTM and autograft post excisional skin cancer surgery.
Case Report
This patient presented with biopsy proven recurrent basal cell carcinoma (BCC) over his left preauricular area that previously treated in 2018 with excisional surgery and split thickness autograft. He is a nonsmoker with no other significant past medical history. He underwent subsequent wide local excisional surgery and staged BTM wound reconstruction and autograft, followed by adjuvant radiotherapy. The excisional surgery was down to periosteum overlying zygoma and branches of the facial nerve, measuring 5cmx13cm extending from lateral to the lateral canthus. Histological analysis of excised specimen reported showed an infiltrating BCC of 11cm in diameter. BTM was applied to the wound with subsequent autograft harvested at 10/1000th inch thickness from his donor. He was further treated with 45/Gyx20 treatment of adjuvant radiation. He did not develop any wound related complication on review 6 months after completion of his adjuvant radiotherapy of the reconstructed wound.
Discussion
BTM is an adjunct used in Plastic Surgery for problematic wounds [1]. It is a synthetic dermal replacement scaffold which facilitates integration of vascular tissue to form a neo dermis for subsequent autograft. BTM has been shown to be a safe and effective treatment in both animal and human [2-5] wounds. It is commonly applied at free flap donor sites [6] for improved skin graft take and when relevant, promotes better tendon glide compared to traditional autograft alone [7-9]. To the best of our knowledge, we are not aware of any published literature on survival of BTM treated wounds after radiotherapy
The negative effects of radiotherapy on skin and wound healing are well documented: both acutely via radiodermatitis (the combination of erythema, oedema, desquamation and pigmentation) and ulceration (due to failure of epidermal regeneration after the elimination of germinal cell populations [10]). Long-term atrophy, contraction and ulceration through depletion of parenchymal and stromal elements [11] is also seen following radiotherapy, with observed hypoxic, hypocellular and hypo vascular tissue [12], which is proposed to be mediated via the deregulated production of various cytokines including TGF-β causing sustained activation of myofibroblasts [13].
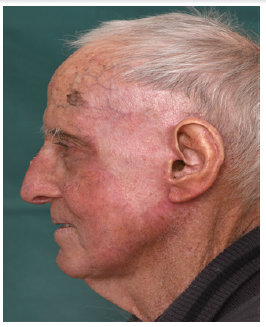
Well vascularized tissue such as local, regional and free flaps are commonly used for reconstruction of wounds that are expected to receive radiotherapy. We hope our case report demonstrates BTM and autograft as an alternative reconstructive option, but more robust research is required to investigate this further (Figure 1-4).
Figure 1:Large keratotic BCC prior to any surgical intervention.

Figure 2:Initial excisional surgery and autograft for first skin cancer in 2018.
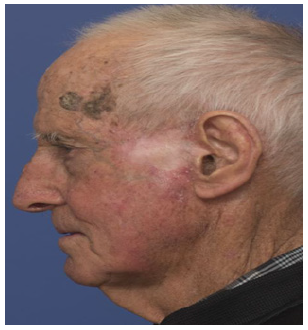
Figure 3: Clinical recurrence of telangiectasia and nodularity at 10 o’ clock and 6 o’clock margins (biopsy proven).

Figure 4: Result, 10 months after BTM, SSG and 6 months after completion of adjuvant radiation.
Conclusion
Our case report showed a positive experience of a wound treated with staged BTM and autograft and subsequent radiotherapy.
References
- Li A, Dearman BL, Crompton KE, Moore TG, Greenwood JE (2009) Evaluation of a novel biodegradable polymer for the generation of a dermal matrix. J Burn Care Res 30(4): 717-728.
- Greenwood JE, Li A, Dearman BL, Moore TG (2010) Evaluation of NovoSorb™ novel biodegradable polymer for the generation of a dermal matrix. Part 2: In-vivo studies. Wound Pract Res 18(1): 24-34.
- Greenwood JE, Dearman BL (2012) Comparison of a sealed, polymer foam biodegradable temporising matrix against Integra™ dermal regeneration template in a porcine wound model. J Burn Care Res 33(1): 163-173.
- Wagstaff MJD, Driver S, Coghlan P, Greenwood JE (2014) A randomised, controlled trial of negative pressure wound therapy of pressure ulcers via a novel polyurethane foam. Wound Repair Regen 22(2): 205-211.
- Wagstaff MJ, Schmitt BJ, Coghlan P, Finkemeyer JP, Caplash Y, et al. (2015) A biodegradable polyurethane dermal matrix in reconstruction of free flap donor sites: A pilot study. Eplasty 15: e13.
- Wagstaff MJ, Schmitt BJ, Caplash Y, Greenwood JE (2015) Free flap donor site reconstruction: A prospective case series using an optimized polyurethane biodegradable temporizing matrix. Eplasty 15: e27.
- Li H, Lim P, Stanley E, Lee G, Lin S, et al. (2021) Experience with novosorb® biodegradable temporising matrix in reconstruction of complex wounds. ANZ J Surg, USA.
- Wagstaff MJ, Caplash Y, Greenwood JE (2017) Reconstruction of an anterior cervical necrotizing fasciitis defect using a biodegradable polyurethane dermal substitute. Eplasty 17: e3.
- Damkat TL, Greenwood JE, Wagstaff MJD (2019) A synthetic biodegradable temporising matrix in degloving lower extremity trauma reconstruction: A case report. Plast Reconstr Surg Glob Open 7(4): e2110.
- Olascoaga A, Vilar CD, Poitevin CA, Contreras RJ (2008) Wound healing in radiated skin: Pathophysiology and treatment options. Int Wound J 5(2): 246-257.
- Rudolph R, Vande Berg J, Schneider JA, Fisher JC, Poolman WL (1988) Slowed growth of cultured fibroblasts from human radiation wounds. Plast Reconstr Surg 82(4): 669-677.
- Marx RE, Ehler WJ, Tayapongsak P, Pierce LW (1990) Relationship of oxygen dose to angiogenesis induction in irradiated tissue. Am J Surg 160(5): 519-524.
- Devalia HL, Mansfield L (2008) Radiotherapy and wound healing. Int Wound J 5(1): 40-44.
© 2021 EK Tan. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






