- Submissions

Full Text
Innovation in Tissue Engineering & Regenerative Medicine
Tissue Engineering for Reconstitution of Human Testicular Niche; One Step Closer to Fertility Preservation and Male Infertility Treatment
Mahdieh Javidpou1, Jalal Golzadeh1, Fatemeh Hajizadeh Tafti1 and Behrouz Aflatoonian1-5*
1 Stem Cell Biology Research Center, Yazd Reproductive Sciences Institute, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
1 Medical Nanotechnology and Tissue Engineering Research Center, Yazd Reproductive Sciences Institute, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
1 Department of Reproductive Biology, School of Medicine, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
1 Department of Advanced Medical Sciences and Technologies, School of Paraedicine, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
1 Department of Genetics, School of Medicine, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
*Corresponding author:Behrouz Aflatoonian, Stem Cell Biology Research Center, Yazd Reproductive Sciences Institute, Shahid Sadoughi University of Medical Sciences, Yazd, Iran, Email: b.aflatoonian@ssu.ac.ir
Submission: May 20, 2019;Published: June 09, 2019
Volume1 Issue3July, 2019
Abstract
Using various sources of stem cells together with different types of scaffolds provides a new route to investigate developmental process of male gametes, which until now was difficult to investigate in the human. In the future tissue engineering may be used for new regenerative medicine application in male infertility. This brief review outlines the progressive insights of this novel biomedical technology and its capabilities, how tissue engineering can mimic developmental processes in vitro and generate a three-dimensional niche for spermatogenesis for research and potential therapies.
Keywords: In vitro gametogenesis; Male infertility; Stem cells; Tissue engineering; Reproductive medicine
Mini Review
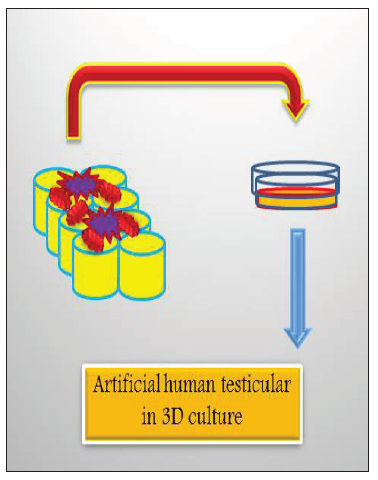
Although assisted reproductive techniques (ART) have facilitated infertility treatments still in some cases especially those with lack of gametogenesis these methods are not helpful. Gametes (sperm and egg: germ cells) which are originated from primordial germ cells (PGCs) play the most crucial role in the body which is transferring genetic information from a generation to the next generation. Therefore, understanding the molecular and cellular mechanisms controlling gametogenesis in human is critical to improve infertility treatments. Nevertheless, ethical and technical difficulties make it almost impossible to access human materials for such researches [1]. Tissue engineering is a multi-disciplinary biotechnological area which employing biomaterial and cell biology techniques for reconstitution of artificial tissues and organs in vitro to use in regenerative medicine [2]. Consequently, according to which tissue or organ is aimed be regenerated various types of biomaterials and different sources of cells using specific growth factors will be applied (Figure 1).
Male infertility is caused by failures in sperm production. Stem cells and biotechnology might be able to help for future treatments using in vitro gametogenesis (IVG). Studies have been started since 1983 by Professor McLaren on PGC culture in mouse [3]. Later, with the birth of embryonic stem cells (ESCs) in mouse [4] and human [5]; scientists have started to work on IVG from ESCs [6-8]. But the first successful report on actual sperm production from mouse ESCs was reported in 2006 with offspring in mouse [9]. Later using organ culture and germ-line stem cells (GSCs) Sato and colleagues were able to produce sperms in vitro [10]. In human, however, the story is different as explained by Surani’s group. They have shown that early primordial germ cell (PGC) development in human is depending on the expression of SOX17 whereas in mouse Blimp1 plays the critical role [11]. Nevertheless, there are debates regarding the pluripotency of the putative GSCs from human testis [12]. Recently, researchers worked on the reconstitution of human testis niche using porous [13] and nanofiber scaffolds [2]. The results of these works are making us one step closer to the actual understanding of the causes of male infertility which will lend it to the regenerative medicine treatments eventually. In the future, using artificial niches produced by testis derived cells seeded onto the scaffolds and IVG from hESCs, it might feasible to mimic testicle organoids as a human in vitro model.
Figure 1:A schematic diagram showing how cells and scaffolds are plated into the dish to form an artificial niche for tissue engineering for sperm production. Testicular derived cells as stromal cells for male germ cells niche together with pluripotent stem cells-derived male germ cells can be cultured onto the scaffold made using testis specific ECM such as laminin and type IV collagen to reconstitute artificial human testis to mimic human male germ cell development for in vitro studies.
Conclusion
According to the recent reports [14,15] the path for the future could be using decellularized seminiferous tubules from different mammals as a natural biocompatible scaffold for reconstitution of human testicular organoids using either human testicular cells or their conditioned medium with hESCs or iPSCs [16].
References
- Moore H, Udayashankar R, Aflatoonian B (2008) Stem cells for reproductive medicine. Mol Cell Endocrinol 288(1-2): 104-110.
- Borzouie Z, Naghibzadeh M, Talebi AR, Pourrajab F, Jebali A, et al. (2019) Development of an artificial male germ cell niche using electrospun poly vinyl alcohol/human serum albumin/gelatin fibers. Cell J 21(3): 300-306.
- De Felici M, McLaren A (1983) In vitro culture of mouse primordial germ cells. Exp Cell Res 144(2): 417-427.
- Evans MJ, Kaufman MH (1981) Establishment in culture of pluripotential cells from mouse embryos. Nature 292(5819): 154-156.
- Thomson JA, Itskovitz-Eldor J, Shapiro SS, Waknitz MA, Swiergiel JJ, et al. (1998) Embryonic stem cell lines derived from human blastocysts. Science 282(5391): 1145-1157.
- Toyooka Y, Tsunekawa N, Akasu R, Noce T (2003) Embryonic stem cells can form germ cells in vitro. Proc Natl Acad Sci USA 100(20): 11457-11462.
- Clark AT, Bodnar MS, Fox M, Rodriquez RT, Abeyta MJ, et al. (2004) Spontaneous differentiation of germ cells from human embryonic stem cells in vitro. Hum Mol Genet 13(7): 727-739.
- Aflatoonian B, Ruban L, Jones M, Aflatoonian R, Fazeli A, et al. (2009) In vitro post-meiotic germ cell development from human embryonic stem cells. Hum Reprod 24(12): 3150-3159.
- Nayernia K, Nolte J, Michelmann HW, Lee JH, Rathsack K, et al. (2006) In vitro-differentiated embryonic stem cells give rise to male gametes that can generate offspring mice. Dev Cell 11(1): 125-132.
- Gohbara A, Katagiri K, Sato T, Kubota Y, Kagechika H, et al. (2010) In vitro murine spermatogenesis in an organ culture system. Biol Reprod 83(2): 261-267.
- Irie N, Weinberger L, Tang WW, Kobayashi T, Viukov S, et al. (2015) SOX17 is a critical specifier of human primordial germ cell fate. Cell 160(1-2): 253-268.
- Sadeghian-Nodoushan F, Aflatoonian R, Borzouie Z, Akyash F, Fesahat F, et al. (2016) Pluripotency and differentiation of cells from human testicular sperm extraction: An investigation of cell stemness. Mol Reprod Dev 83(4): 312-323.
- Borzouie Z, Hekmati MSH, Talebi AR, Rajab F, Jebali A, et al. (2015) Reconstitution of an artificial human testis using a 3-dimensional (3D) culture device. Proc 31st Annual Meeting of the European Society for Human Reproduction and Embryology, Lisbon, Portugal, Hum Reprod 30: 457-458.
- Vermeulen M, Del Vento F, de Michele F, Poels J, Wyns C (2018) Development of a cytocompatible scaffold from pig immature testicular tissue allowing human sertoli cell attachment, proliferation and functionality. Int J Mol Sci 19(1): pii: E227.
- Xie P, Trout A, Rosenwaks Z, Palermo GD (2019) Differentiation of embryonic stem cells into germ line cells using decellularized seminiferous tubules bathed in a conditioned medium. 35th Annual Meeting of the European Society for Human Reproduction and Embryology, Vienna, Austria.
- Del Vento F, Vermeulen M, de Michele F, Giudice MG, Poels J, et al. (2018) Tissue engineering to improve immature testicular tissue and cell transplantation outcomes: one step closer to fertility restoration for prepubertal boys exposed to gonadotoxic treatments. Int J Mol Sci 19(1): pii: E286.
© 2019 Behrouz Aflatoonian. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






