- Submissions

Full Text
Innovation in Tissue Engineering & Regenerative Medicine
Tissue Engineering and Human Regenerative Therapies in Space: Benefits for Earth and Opportunities for Long Term Extra-Terrestrial Exploration
Martin Braddock*
Sherwood Observatory, Mansfield and Sutton Astronomical Society, UK
*Corresponding author:Martin Braddock, Sherwood Observatory, Mansfield and Sutton Astronomical Society, Coxmoor Road, Sutton-in-Ashfield, Nottinghamshire, United Kingdom,NG17 5LF, Tel: +44 (0) 7748 761258;
Submission: May 23, 2019;Published: June 03, 2019
Volume1 Issue3June, 2019
Abstract
Living and working in space presents many challenges for maintenance of optimal human physiology and psychology. The physical effects of microgravity and increased radiation exposure together with the psychological effects of isolation on human beings pose problems which are under intense investigation by global space agencies, corporate and academic research institutions. An unsurmountable challenge, at least today, for deep space exploration and colonisation (DSEC) is the longevity of human lifespan and the potential for organ system dysfunction which may lead to premature death and mission termination in the absence of bio-reparative capabilities. The unique nature of microgravity encountered in space provides both a challenge and an opportunity for regenerative medicine that cannot be fully replicated on Earth. This minireview describes some recent advances in the use of stem cells, tissue engineering and the potential for 3D bioprinting in space as future concepts for consideration in the design of missions supporting longer term space exploration and colonisation.
Introduction
On Earth gravity is constant and although the precise value depends upon location, the standard value of acceleration due to gravity is 9.81ms-2. This is referred to as 1g. In space astronauts experience microgravity (μG) of approximately 1x10-6ms-2 and on the International Space Station (ISS), astronauts float in space as they are in free fall because for any spacecraft to stay in Earth orbit, it must move at almost exactly the right speed so that the curve of downward acceleration matches the curvature of the Earth. This means that the ISS is an ideal laboratory [1] for studying the effects of μG on living systems to investigate growth and development at both the cellular level, in cell co-culture and in complex cellular systems where scaffolds may be required to build architecture and shape that is unconstrained by gravity as is the case in an Earth-bound laboratory. The deleterious effects of living and working in μG on astronaut physiology and psychology have been extensively reviewed [2-9]. As of May 21st 2019, 571 people have travelled into space [10] spending from Alan Shepherd’s 15min flight on board Freedom 7 in 1961 to Valerei Polyakov’s 437d 18h flight on the Mir space station in 1995. The length of time that astronauts have lived in μG has varied widely and it is principally since the launch of the ISS, that long duration missions (LDMs) of >3mo have become the norm.
Astronauts typically spend 6mo on the ISS, however, for supporting the planned LDMs to Mars expected in the late 2020s and early 2030s, it is expected that astronauts will spend a minimum time of 18mo in μG, during which time they will experience both soft and hard tissue atrophy and receive a large component of the recommended lifetime exposure to radiation. Although today, LDMs beyond our solar system remain purely conceptual and a likely consequence of successful travel and colonisation of Mars, mission planners in the all the major space agencies are considering the possibility of very long duration missions (vLDMs) for a number of years, even including the possibility of multi-generational space travel [11,12]. National Aeronautics and Space Administration (NASA) has compiled an inventory of studies, some of which are aimed at studying the effects of μG on cell and tissue growth and on the use of three-dimensional (3D) printing in space. The inventory of experiments by hardware [13] or by name [14] describes completed studies and studies in progress and together with an archive of historical studies is a valuable repository of information. A further useful repository of information is the public open access tool describing significant safety related incidents in spaceflight [15] and despite the high risk, the principal injuries to astronauts in situ have been restricted to musculoskeletal injury and space adaptation back pain [16]. This in part, may emphasize a potential requirement for restorative surgery for body parts during vLDMs where their impaired function is a consequence of the environment of μG and increased exposure to radiation. In this mini-review I will highlight recent advances in tissue engineering, stem cell biology and 3D bio-printing drawn from studies conducted in space. I will conclude with some future looking perspectives and speculate on Earth-bound advances that may drive future studies in an extraterrestrial environment.
Tissue Engineering and Regenerative Medicine (TERM)
Driven in part by a lack of donor tissues and organs on Earth [17], the field of TERM has made remarkable progress over the years [18] and has exploited the use of simulated μG in rotating wall vessel (RWV) bioreactors to generate both soft and hard tissue constructs [19] and in RWVs on the Mir space station [18,20]. Starting from the mid-1990s, numerous studies have suggested that studies supporting TERM in simulated μG on Earth may produce a 3D construct of higher quality when compared with counterparts produced at 1g [21,22] and numerous elaborate methodologies have been developed [23]. The manufacture of tissues on Earth and in space using conditions of simulated or real μG is a field that attracts and receives much attention in regenerative medicine and has been described in many excellent reviews e.g. [24,25].
Organoid and Organ Growth
The use μG to overcome limitations of monolayer cell growth as either a single cell type or in co-culture with multiple cell types has been recently reviewed [24,25]. μG has been successfully exploited to manufacture microtissues and organoids [26], in either simulated or real μG conditions sustained over longer periods of time and it may be possibly to construct a self-assembling organoid where cell to cell contacts are not constrained by Earth gravity leading to the production of tissue assemblies. The construction of 3D aggregates from different cell types using devices originally created to prepare for spaceflight such as the random positioning machine (RPM), fast rotating clinostat (FRC), or rotating wall vessel bioreactor may lead to the development of blood vessels and other soft and hard tissues such as cartilage and bone [25,26].
Two recent papers further progress this field. In the first paper, human thyroid cancer cells and human endothelial cells were shown to form 3D spheroids when grown in cultures exposed to simulated μG in an RPM and FRC or in real μG on board the ISS for up to 14d [27]. Studies in both μG regimes may inform on the design of future human tissue fabrication for use in transplantation and in the most recent study published in 2019, Earth-based studies in simulated μG have successfully informed on experimental design for growing blood vessels in space on board the ISS [28]. The latter study is important because, for the first time, human endothelial cells have been shown to assemble into multi-cellular spheroids and subsequently tubular structures resembling the intima of rudimentary blood vessels and in the absence of a supporting scaffold. This early study may hold promise for the ultimate development of blood vessels for transplantation and bypass surgery and suggests that the environment of μG, which does not constrain cell sedimentation, may provide an environment more conducive to blood vessel manufacture than can be achieved on Earth.
Stem Cell Manipulation
On Earth the potential for human stem cells to produce soft and hard tissue structures either with or without supporting scaffolds is an area of great potential promise for the future of translational medicine and has recently been reviewed [29,30]. In 2018, a novel type of stem cell that is able to produce new air sac cells in murine models of lung injury and in human lung tissue was discovered and characterised [31]. The duration of simulated μG has been shown to affect the differentiation of mesenchymal stem cells [32] and a further study [33], employing rabbit articular chondrocytes (ACs) or adipose-derived stem cells (ASCs) showed rapid attachment to the surface of cartilage extracellular matrix (ECM)-derived particles (CEDPs) and cell proliferation of high viability under conditions of μG in a rotary cell culture system or under static conditions. Interestingly under culture conditions of μG in the bioreactor used, maintenance of the chondrogenic phenotype of ACs and their ability to induce ACS chondrogenesis was superior to cultures grown under static conditions [33].
Stem cell growth and differentiation has been investigated in space on both the Mir and ISS and the study showed that μG inhibited stem cell differentiation while preservation of stemness was maintained [34]. A further ISS-based study exploring stem cell expansion in μG completed in 2017 and the results have yet to be published [35]. A third study reported in 2019 [36] showed that stem-like cells which are precursors for tissue regeneration in the newt Urodela under simulated μG, showed up to a 2 fold enhancement of cell proliferation, accelerating source cell differentiation in addition to sequential differentiation in the retina, lens and limb, producing larger and more developed regenerates than their 1g control counterparts.
This is a field still in the early stages of delivering on the promise of generalised tissue repair for humankind and the high cost of space missions precludes design and completion of a large number of studies in space, placing a dependency on Earth-based experiments in simulated μG. There is much to learn and gain from working in simulated and real μG where there may be many applications for human health in the field of stem cell derived TERM.
3D Bioprinting
3D bioprinting is an additive manufacturing methodology which employs simultaneous layer by layer deposition of cell types and cyto-compatible biomaterials such as hydrogels which, together provide a supporting structure capable of generating organoids or potentially whole functional organs. It has been successfully used on Earth to produce ear-shaped cartilage for auricular reconstruction [37]. The area has been recently reviewed and the state of the bioprinting art on Earth and potential applications for regenerative medicine in space is discussed [38]. In February 2019, the world’s first bio-fabrication experiment was reported [39] having been performed during Expedition 57 on board the ISS. 3D Bioprinting Solutions, in partnership with the Russian Federal Space Agency Roscomos, has successfully tested formative bioprinting of threedimensional tissue spheroids comprising mouse thyrocytes using low concentrations of paramagnetic nanoparticles which are more amenable to the protection of cell culture viability. The thyroid gland’s sensitivity to radiation exposure has been well documented [40] and is an ideal first target organ for study, which together with human cartilage provided reference points for Earthbased laboratory work. The fabrication of other organ constructs should follow in future experiments. The images obtained show the thyroid gland constructed from spheroids and comprising thyrocytes (Figure 1a) and a histological section of a fabricated human cartilage construct consisting of chondrocytes (Figure 1b). Both constructs showed living cells with typical morphology.
Figure 1:Photographs of constructs generated on Expedition 57 on board the ISS. a). Thyroid gland constructed from spheroids and b). Histological section of a cartilage construct consisting of chondrocytes. Scale bar=250μm. Images are reproduced with the permission of 3D Bioprinting Solutions (Moscow, Russia).
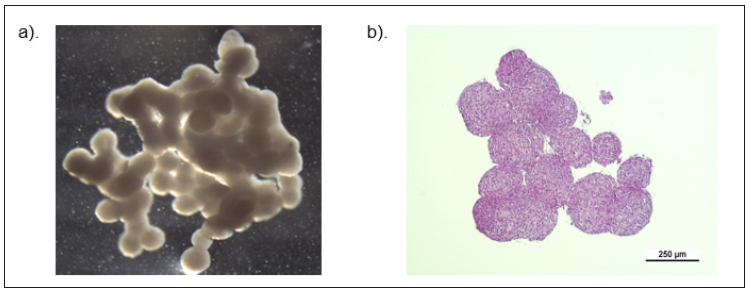
This pioneering study has confirmed the feasibility of formative bioprinting in uG and may pave the way for in situ manufacture of human organ constructs, with the future potential for organ replacement on long space voyages. Together with the development of autonomous and semi‐autonomous robotic surgical systems which include the STAR (smart tissue autonomous robot) [41,42], a futuristic scenario may be for subsequent generations of space travelling astronauts to request organ replacements and autonomous surgery on demand.
Potential Future Clinical Application and Conclusions
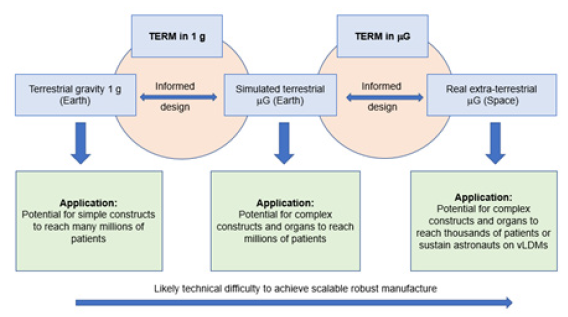
This mini-review has provided a brief update of selected studies in tissue engineering, stem cell application and 3D bioprinting recently published which illustrate the potential opportunity for TERM based on studies conducted in either simulated μG on Earth or real μG in space, when compared with 1g on Earth (Figure 2). Though TERM in 1g holds promise to deliver benefit to many millions of patients and may be less technically demanding to achieve, TERM in either simulated or real μG may generate constructs of better quality albeit for fewer patients and with fabrication challenges which have yet to be solved on a large scale. As described earlier, there are many potential advantages for TERM in μG, which principally lie in the replication of three-dimensional structure which are challenging to obtain under conditions of 1g on Earth. In part, the review adds further support to two potential applications, the first being to increase scientific knowledge for the design of tissue reparative approaches which may benefit humankind on Earth. As it appears, at least for studies in mammalian cell culture that simulated μG is a good analogue for real μG [43], cost-effective terrestrial studies may provide essential guidance to inform decision making to steer forward-looking enterprise. Secondly and more futuristically, TERM studies in μG may support the concept of DSEC via vLDMs either within or maybe out with our solar system where designer organs may be requested on demand. Given the rapid advancement of 3D bioprinting on Earth and the promising early stage results shown in some autonomous surgical procedures, this technology may become an option for future mission planners who may be mandated to prolong human lifespan beyond that achieved on Earth.
Figure 2:Representation of TERM in 1g, simulated μG (Earth) and real μG (space) with potential applications and reach to patients and astronauts together with speculated likely level of difficulty to achieve robust and scalable construct manufacture.
Acknowledgement
I would like to acknowledge 3D Bioprinting Solutions (Moscow, Russia) for their kind permission to use the images of bioprinted constructs from ISS Expedition 57. I am a member of the Mansfield and Sutton Astronomical Society (MSAS), a Fellow of the Royal Society of Biology and a Fellow of the Royal Astronomical Society. MSAS is a registered charity, number 51813 and was founded in 1970 to foster interest in astronomy in Ashfield, Nottinghamshire, United Kingdom and surrounding district.
References
- International Space Station Benefits for Humanity. https://www.nasa. gov/mission_pages/station/research/benefits/index.html. Retrieved on May 21st, 2019.
- Aubert AE, Larina I, Momken I, Blanc S, White O, et al. (2016) Towards human exploration of space: the THESEUS review series on cardiovascular, respiratory and renal research properties. NPJ Microgravity 2: 16031.
- Caiani EG, Martin-Yebra A, Landreani-F, Bolea J, Laguna P, et al. (2016) Weightlessness and cardiac rhythm disorders: current knowledge from space flight and bed-rest studies. Front Astron Space Sci 3: 27.
- Carpenter RD, Lang TF, Bloomfield SA, Bloomberg JJ, Judex S, et al. (2010) Effects of long-duration spaceflight, microgravity and radiation on the neuromuscular, sensorimotor and skeletal systems. J Cosmol 12: 3778-3780.
- Cavanagh PR, Licata AA, Rice AJ (2005) Exercise and pharmacological countermeasures for bone loss during long duration space flight. Gravit Space Biol Bull 18(2): 39-58.
- Graebe A, Schuck EL, Lensing P, Putcha L, Derendorf H (2004) Physiological, pharmacokinetic and pharmacodynamic changes in space. J Clin Pharmacol 44(8): 837-853.
- Lang T, van Loon JJWA, Bloomfield S, Vico L, Chopard A, et al. (2017) Towards human exploration of space: the THESEUS review series on muscle and bone research priorities. NPJ Microgravity 3: 8.
- Van Ombergen A, Demertzi A, Tomilovskaya E, Jeurissen B, Sijbers J, et al. (2017) The effects of spaceflight and microgravity on the human brain. J Neurol 264 (Suppl 1): S18-S22.
- Braddock M (2017) Ergonomic challenges for astronauts during space travel and the need for space medicine. J Ergonomics 7: 1-10.
- Astronaut/Cosmonaut Statistics. https://www.worldspaceflight.com/ bios/stats.php. Retrieved on May 21st, 2019.
- Smith CM (2014) Estimation of a genetically viable population for multi-generational interstellar voyaging: Review and data for project Hyperion. Acta Astronautica 97: 16-29.
- Marin F, Beluffi C (2018) Computing the minimal crew for a multigenerational space journey towards Proxima b. J Brit Interplan Soc 71: 45-52.
- Experiments by Hardware - 10.04.18. https://www.nasa.gov/mission_ pages/station/research/experiments/experiments_hardware.html. Retrieved on May 21st, 2019.
- Experiment List - Alphabetical - 10.04.18. https://www.nasa.gov/ mission_pages/station/research/experiments/experiments_by_name. html. Retrieved on May 21st, 2019.
- Significant Incidents and Close Calls in Human Spaceflight. https:// spaceflight.nasa.gov/outreach/SignificantIncidents/index.html. Retrieved on May 21st, 2019.
- Braddock M, Szocik K, Campa R (2019) Ergonomic constraints for astronauts: challenges and opportunities today and for the future in contemporary ergonomics and human factors. In: Charles R and Golightly D (Eds.), IEHF ISBN: 978-1-9996527-1-5, pp. 293- 301.
- Lieben L (2016) Regenerative medicine: the future of 3D printing of human tissues is taking shape. Nat Rev Rheumatol 12(4): 191.
- Unsworth BR, Lelkes PI (1998) Growing tissues in microgravity. Nature Med 4(8): 901-907.
- Barzegari A, Sael AA (2012) An update to space biomedical research: tissue engineering in microgravity bioreactors. BioImpacts 2(1): 23-32.
- Freed LE, Langer R, Martin I, Pellis NR, Vunjak-Novakovic G (1997) Tissue engineering of cartilage in space. Proc Natl Acad Sci USA 94(25): 13885-13890.
- Freed LE, Vunjak-Novakovic G (1997) Microgravity tissue engineering. In vitro Cell Dev Biol Animal 33(5): 381-385.
- Wehland M, Grimm D (2017) Tissue engineering in microgravity. Biotechnology in Space, pp.73-85.
- Grimm D, Wehland M, Pietsch J, Aleshcheva G, Wise P, et al. (2014) Growing tissues in real and simulated microgravity: new methods for tissue engineering. Tissue Eng Part B Rev 20(6): 555-566.
- Grimm F, Egli M, Kruger M, Riwaldt S, Corydon TJ (2018) Tissue engineering under microgravity conditions -use of stem cells and specialized cells. Stem Cells Dev 27(12): 787-804.
- Costa-Almeida R, Granja PL, Gomes ME (2018) Gravity, tissue engineering and the missing link. Trends Biotech 36(4): 343-347.
- Aleshcheva G, Bauer J, Hemmersbach R, Slumstrup L, Wehland M, et al. (2016) Scaffold-free tissue formation under real and simulated microgravity conditions. Basic Clin Pharm Toxicol 119(Suppl 3): 26-33.
- Kopp S, Kruger M, Wehland M, Bauer J, Dittrich A (2018) Growing tissues in space. Frontiers in Physiology 9.
- Kruger M, Kopp, S, Wehland, M, Bauer J, Baatout S, et al. (2019) Growing blood vessels in space: preparation studies of the SPHEROIDS project using related ground-based studies. Acta Astronautica 159: 267-272.
- Xu XY, Li X, Wang J, He XT, Sun HH, et al. (2019) Concise review: periodontal tissue regeneration using stem cells: strategies and translational considerations. Stem Cells Trans Med 8(4): 392-403.
- Xia H, Li X, Gao W, Fu X, Fang RH, et al. (2018) Tissue repair and regeneration with endogenous stem cells. Nature Reviews Materials 3: 174-193.
- Zacharias WJ, Frank DB, Zepp JA, Morley MP, Alkhaleel F, et al. (2018) Regeneration of the lung alveolus by an evolutionarily conserved epithelial progenitor. Nature 555(7695): 251-255.
- Xue L, Li Y, Chen J (2017) Duration of simulated microgravity affects the differentiation of mesenchymal stem cells. Mol Med Rep 15(5): 3011- 3018.
- Yin H, Wang Y, Sun X, Cui G, Sun Z, et al. (2018) Functional tissueengineered microtissue derived from cartilage extracellular matrix for articular cartilage regeneration. Acta Biomaterialia 77: 127-141.
- Blaber EA, H Finkelstein, N Dvorochkin, KY Sato, R, Yousuf et al. (2015). Microgravity reduces the differentiation and regenerative potential of embryonic stem cells. Stem Cells Dev 24(22): 2605-2621.
- Stem cell expansion in microgravity. www.nasa.gov/ mission_pages/ station/research/experiments/1971.html. Retrieved on May 21st, 2019.
- Grigoryan EN, Radugina EA (2019) Behaviour of stem-like cells, precursors for tissue regeneration in Urodela, under conditions of microgravity. Stem Cells Dev 28(7): 423-437.
- Zhou G, Jiang H, Yin Z, Liu Y, Zhang Q, et al. (2018) In vitro regeneration of patient-specific ear shaped cartilage and its first clinical application for auricular reconstruction. EBioMedicine 28: 287-302.
- Ghidini T (2018) Regenerative medicine and 3D bioprinting for human space exploration and colonisation. J Thorac Dis 10 (Suppl 20): S2363-S2375.
- Three dimensional bioprinting in space. https://bioprinting.ru/en/ press-center/publications/nasa-organaut/. Retrieved on May 21st, 2019.
- Sinnott B, Ron E, Schneider AB (2010) Exposing the thyroid to radiation: a review of its current extent, risks, and implications. Endocr Rev 31(5): 756-773.
- Shademan A, Decker RS, Opfermann JD, Leonard S, Krieger A, et al. (2016) Supervised autonomous robotic soft tissue surgery. Science Trans Med 8(337): 337ra64.
- Aruni G, Amit G, Dasgupta P (2018) New surgical robots on the horizon and the potential role of artificial intelligence. Investig Clin Urol 59(4): 221-222.
- Wuest SL, Richard S, Kopp S, Grimm D, Egli M (2015) Simulated microgravity: critical review on the use of random positioning machines for mammalian cell culture. BioMed Res Int: 971474.
© 2019 Martin Braddock. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






