- Submissions

Full Text
Intervention in Obesity & Diabetes
Effect of Diabetes and other Risk Factors on Bone Health
Debjita Mukherjee1 and Jhaleh Amirian2*
1Department of Biotechnology, SRM University, India
2College of Materials Science and Engineering, Shenzhen University, China
*Corresponding author:Jhaleh Amirian, College of Materials Science and Engineering, Shenzhen University, Shenzhen 518055, Guangdong Province, PR China
Submission:January 21, 2022;Published: February 01, 2022

ISSN 2578-0263Volume5 Issue5
Abstract
Diabetes Mellitus (DM) affects a significantly large part of the population globally. Several kinds of research are being conducted every day around the world trying to understand the underlying mechanisms of the disease better to develop better treatments. One of the significant effects of diabetes is on the skeletal system of the patients. The disease affects the bone quality, mineral density, bone turnover and in turn bone health at large. This effect on bone health is worsened by several risk factors as well. This mini review aims at presenting some of the most important mechanisms behind this deterioration of bone health and how risk factors affect them according to latest research done in this field.
Keywords:Diabetes; Bone mineral density; Bone health; Risk factors
Introduction
Diabetes is a metabolic disease leading to increased levels of glucose in blood. This happens due to insufficient secretion of the hormone insulin like in Type 1 Diabetes due to destroyed beta cells in the pancreatic islets (auto-immune). Diabetes can also be caused by inability of the insulin to act on the glucose due to resistance towards it in the patient’s system as in Type 2 Diabetes [1]. The insulin helps in breaking down glucose to glycogen which is accepted by cells for various metabolic activities. According to the statistics published by the International Diabetes Federation (IDF) for 2021, about 537 million adults and around 1.2 million children and adolescents are suffering from diabetes [2]. This value is estimated to increase by more than a 100 million within the next 10 years. The symptoms of diabetes include polyuria (frequent urination), polydipsia (increased thirst), polyphagia (increased hunger), fatigue, blurred vision, delayed wound healing, and skin problems [3,4]. Prolonged exposure to the disease leads to fatal conditions such as keto-acidosis, cardiovascular diseases, kidney disorders, and diabetes has also to be a co-morbidity factor for COVID-19 related deaths recently [4,5].
Bone Mineral Density (BMD) is the measure of the mass of bone minerals within the bone tissues which determines the strength of the bone. The BMD is highly useful for diagnosing conditions such as osteoporosis [6]. The bone quality of an individual is also a factor which results in bone defects or fractures. It affects bone strength independently from BMD. It includes several structural and compositional factors such as internal and matrix composition of the bone, bone turnover, mineralization, microarchitecture, and microdamage [7]. Bone health is also indicated by the Bone Turnover Markers (BTM) which are indicative of the interplay of the bone cells in bone development and metabolism [8]. The bone formation markers like procollagen type I N propeptide (PINP), osteocalcin or alkaline phosphatase are directly related to osteoblast activity. The resorption marker levels, on the other hand, indicate osteoclast activity. These include N-telopeptide of type I collagen (NTX), carboxy-terminal crosslinking telopeptide of type I collagen (CTX), and Deoxypyridinoline (DPD). Over the years, several research have shown diabetes to affect the BMD, bone quality, and bone turnover of the patients leading to increase in incidents of fractures and defects in the bone. This review will target on the recent findings showing how diabetes along with several risk factors affects these three factors resulting in bone fracture or defects.
Mechanisms Behind Diabetes Leading to Bone Fragility
Several complex mechanisms affect bone fragility in patients with Diabetes Mellitus (DM) based on its effect on the genetic expressions, biochemical pathways, bone formation process, and cell-signaling mechanisms. Insulin is involved in the differentiation and apoptotic cell-signaling pathways for osteoblasts [9]. It de-represses the CDK-2 (cyclin-dependent kinase) pathway by blocking p27, resulting in proliferation and maturation of osteoblasts. Also, insulin inhibits apoptosis by activating the PI3K (phosphatidylinositol 3-kinase) pathway which inhibits BAD (BCLassociated death promoter) by phosphorylation. The Wnt signaling pathway is also affected in the diabetic patients resulting in poorer bone quality. The Sirtuin class of proteins, seven of which are present in the mammalian genome, has been found to play an important role in apoptosis and senescence of cells thereby affecting aging [10,11]. The altered expression of the Silent Information Regulator of Transcription1 (SIRT1) gene has also shown to affect insulin resistance, beta cell dysfunction and alterations in metabolic regulations in both T2DM and T1DM [12]. The SIRT1 gene expression is directly related to bone mass and has also been identified as an important genetic factor in osteoporosis [13]. Hence, depending on SIRT-1 expression levels, bone health in diabetic patients can vary. Biochemical pathway disruptions in diabetic patients lead to effects like accumulation of Advanced Glycation End-Products (AGEs) and amylin over-secretion. In T1DM patients, autoantibodies destroy the pancreatic beta cells inhibiting insulin production, but it also increases amylin production [14]. The amylin destroys osteoclasts and promotes osteoblast formation thus affecting bone resorption. The non-enzymatic glycation of proteins, phospholipids, and nucleic acids lead to formation of AGEs which is observed in Type 1 collagen resulting in its cross-linking [9,15]. This prevents adhesion of the osteoblasts to the ECM (Extracellular Matrix) making bones fragile. This occurs if the body is in hyperglycemic state which commonly happens in diabetic patients. In T2DM, decreased vitamin D serum levels affect calcium and phosphate homeostasis [16]. Also, number and function of osteoblasts decrease as they differentiate into fat-storing adipocytes resulting in bone marrow adiposity. Inflammation increases due to micro hypoxia in bone niche and expression of cytokines and chemokines increase leading to accumulation of pro-inflammatory macrophages (M1).
Among structural issues due to diabetes, micro- and macroarchitecture abnormalities and tissue material damage result in bone fragility. Patients with T1DM and T2DM diabetes respectively suffer from early bone loss or development of abnormal osseous architecture which incorrectly show increased or normal BMD. These at a later stage result in increase of incidents of bone fracture and defects [17]. Factors like increased frequency of falls also occur due to diabetic complications or treatment induced hypo-glycemia thereby leading to poor bone health and increased risk of fractures [18].
Bone Health Depends on other Risk Factors in Diabetic Patients
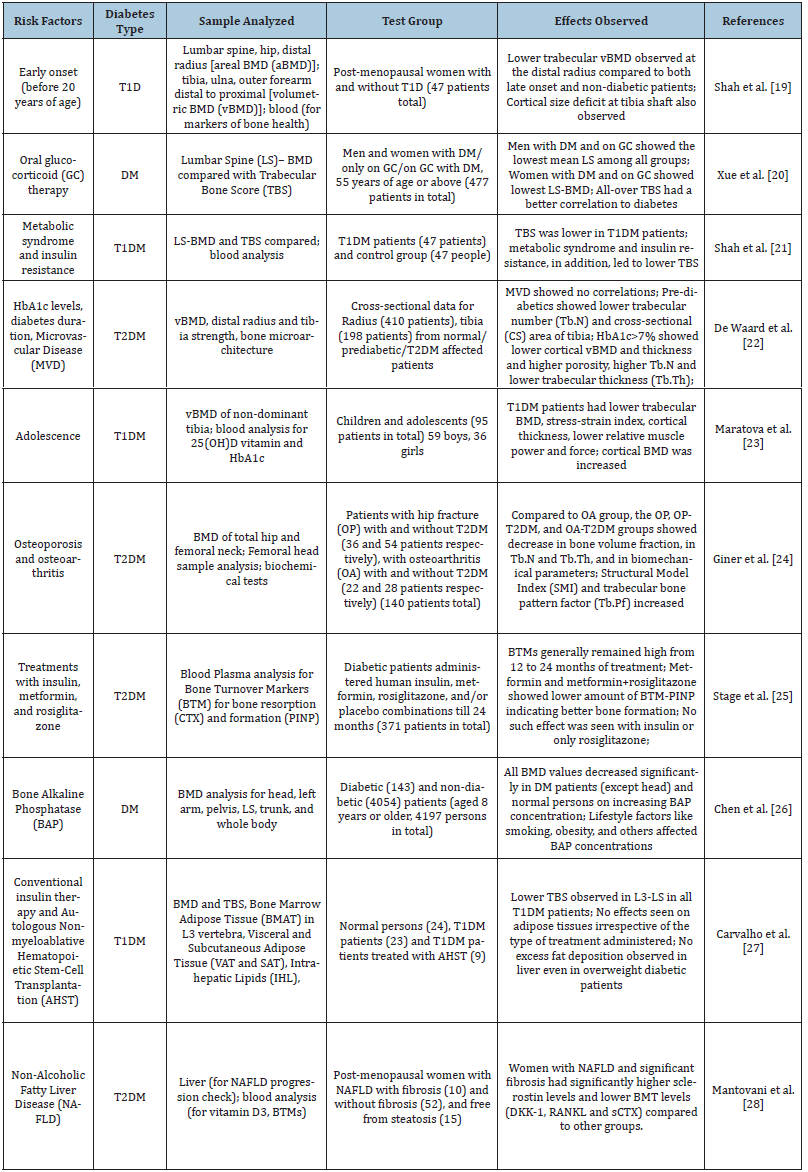
Other than the mechanisms indicated above, various risk factors such as age, sex, other diseases, treatment options and other lifestyle factors also contribute to poorer bone quality and/or BMD thereby leading to poor bone health. Some of the recently studied risk factors have been documented in the table below (Table 1) [19- 28].
Table 1:
Conclusion
The poor quality and mineral density of bones make managing the already complicated diabetes much more difficult. Keeping the risk factors and mechanisms in mind, newer therapies should be developed which will help make the lives of the patients easier. This mini-review attempts at shortly summarizing the most recent research done in this aspect for researchers. Not only that, but it also aims at increasing awareness among the patients and their relatives regarding the potential risk factors responsible for worsening the disease.
Abstract
- American Diabetes Association (2006) Diagnosis and classification of diabetes mellitus. Diabetes Care 31: S81-S90.
- International Diabetes Federation (2021) IDF Diabetes Atlas, (10th edn), Brussels, Belgium.
- Cooke DW, Plotnick L (2008) Type 1 diabetes mellitus in pediatrics. Pediatr Rev 29(11): 374-384.
- Rockefeller JD (2015) Diabetes: symptoms, causes, treatment and prevention.
- Shenoy A, Ismaily M, Bajaj M (2020) Diabetes and covid-19: A global health challenge. BMJ Open Diabetes Res Care 8(1): e001450.
- Richards JB, Rivadeneira F, Inouye M, Pastinen TM, Soranzo N, et al. (2008) Bone mineral density, osteoporosis, and osteoporotic fractures: a genome-wide association study. Lancet 371(9623): 1505-1512.
- Compston J (2006) Bone quality: what is it and how is it measured? Arq Bras Endocrinol Metabol 50(4): 579-585.
- Lane NE, Saag K, O Neill TJ, Manion M, Shah R, et al. (2021) Real-world bone turnover marker use: impact on treatment decisions and fracture. Osteoporos Int 32(5): 831-840.
- Romero DC, Duarte MD, Gutiérrez Romero SA, Mendivil CO (2021) Diabetes and bone fragility. Diabetes Ther 12(1): 71-86.
- Zainabadi K, Liu CJ, Caldwell AL, Guarente L (2017) SIRT1 is a positive regulator of in vivo bone mass and a therapeutic target for osteoporosis. PLoS One 12(9): e0185236.
- Martins IJ (2016) Anti-aging genes improve appetite regulation and reverse cell senescence and apoptosis in global populations. Advances in Aging Research 5(1).
- Martins IJ (2017) Single gene inactivation with implications to diabetes and multiple organ dysfunction syndrome. J Clin Epigenet 3(24): 2472-1158.
- Yang X, Jiang T, Wang Y, Guo L (2019) The role and mechanism of SIRT1 in resveratrol-regulated osteoblast autophagy in osteoporosis rats. Scientific Reports 9(1): 1-15.
- Horcajada Molteni MN, Chanteranne B, Lebecque P, Davicco MJ, Coxam V, et al. (2001) Amylin and bone metabolism in streptozotocin‐induced diabetic rats. J Bone Miner Res 16(5): 958-965.
- Poundarik AA, Wu PC, Evis Z, Sroga GE, Ural A, et al. (2015) A direct role of collagen glycation in bone fracture. J Mech Behav Biomed Mater 52: 120-130.
- Picke AK, Campbell G, Napoli N, Hofbauer LC, Rauner M (2019) Update on the impact of type 2 diabetes mellitus on bone metabolism and material properties. Endocr Connect 8(3): R55-R70.
- Henderson S, Ibe I, Cahill S, Chung YH, Lee FY (2019) Bone quality and fracture-healing in type-1 and type-2 diabetes mellitus. J Bone Joint Surg Am 101(15): 1399-1410.
- Jiang N, Xia W (2018) Assessment of bone quality in patients with diabetes mellitus. Osteoporos Int 29(8): 1721-1736.
- Shah VN, Joshee P, Sippl R, Pyle L, Vigers T, et al. (2019) Type 1 diabetes onset at young age is associated with compromised bone quality. Bone 123: 260-264.
- Xue Y, Baker AL, Nader S, Orlander P, Sanchez AJ, et al. (2018) Lumbar spine trabecular bone score (TBS) reflects diminished bone quality in patients with diabetes mellitus and oral glucocorticoid therapy. J Clin Densitom 21(2): 185-192.
- Shah VN, Sippl R, Joshee P, Pyle L, Kohrt WM, et al. (2018) Trabecular bone quality is lower in adults with type 1 diabetes and is negatively associated with insulin resistance. Osteoporos Int 29(3): 733-739.
- De Waard EAC, de Jong JJA, Koster A, Savelberg HHCM, van Geel TA, et al. (2018) The association between diabetes status, HbA1c, diabetes duration, microvascular disease, and bone quality of the distal radius and tibia as measured with high-resolution peripheral quantitative computed tomography—The Maastricht Study. Osteoporos Int 29(12): 2725-2738.
- Maratova K, Soucek O, Matyskova J, Hlavka Z, Petruzelkova L, et al. (2018) Muscle functions and bone strength are impaired in adolescents with type 1 diabetes. Bone 106: 22-27.
- Giner M, Miranda C, Vázquez GMA, Altea MP, Miranda MJ, et al. (2021) Microstructural and strength changes in trabecular bone in elderly patients with type 2 diabetes mellitus. Diagnostics 11(3): 577.
- Stage TB, Christensen MMH, Jørgensen NR, Beck NH, Brøsen K, et al. (2018) Effects of metformin, rosiglitazone and insulin on bone metabolism in patients with type 2 diabetes. Bone 112: 35-41.
- Chen H, Li J, Wang Q (2018) Associations between bone-alkaline phosphatase and bone mineral density in adults with and without diabetes. Medicine 97(17).
- Carvalho AL, Massaro B, e Silva LT, Salmon CE, Fukada SY, et al. (2019) Emerging aspects of the body composition, bone marrow adipose tissue and skeletal phenotypes in type 1 diabetes mellitus. J Clin Densitom 22(3): 420-428.
- Mantovani A, Sani E, Fassio A, Colecchia A, Viapiana O, et al. (2019) Association between non-alcoholic fatty liver disease and bone turnover biomarkers in post-menopausal women with type 2 diabetes. Diabetes Metab 45(4): 347-355.
© 2022 Jhaleh Amirian. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






