- Submissions

Full Text
Intervention in Obesity & Diabetes
Factors Contributing to Obesity and Associated Health Risks
Qamar Abbas Syed1*, Anam Layla1, Rizwan Shukat1, Muhammad Haseeb Ahmad2 and Hafiza Anum Asghar1
1National Institute of Food Science and Technology, Faculty of Food, Nutrition and Home Sciences, University of Agriculture, Faisalabad, Pakistan
2Institute of Home and Food Sciences, Government College University, Faisalabad, Pakistan
*Corresponding author:Qamar Abbas Syed, National Institute of Food Science and Technology, Faculty of Food, Nutrition and Home Sciences, University of Agriculture, Faisalabad, Pakistan
Submission:July 06, 2021;Published: September 23, 2021

ISSN 2578-0263Volume5 Issue4
Abstract
Obesity is a serious health issue in both developed and developing societies of the world. Apart from being a problem itself, obesity may also result in many chronic health conditions. Uncontrolled obesity may lead to diabetes, cancer, arthritis as well as liver and kidney problems. Obesity is always stigmatized to overeating rather several other factors including metabolic health, cultural and lifestyle factors are also associated with disease progression. Risk of chronic diseases due to genetic factors is less as compared to environmental, behavioral and dietary factors. Behavioral/lifestyle modification is recommended. Developed countries face problem due to high fat (junk food) and sugar containing food (refined carbohydrates) consumption along with amplified alcohol consumption and smoking. Dietary changes like replacing high fat and sugar containing food with high fiber, low sugar and fat foods would impact health status of the individuals in positive way by decreasing risk of chronic diseases.
Keywords:Obesity; Chronic issues; Diabetes; Cancer; Kidney stones
Introduction
Global epidemic of overweight and obesity is of great concern, posing a serious public health threat in both developed and under-developed countries by increasing the burden of chronic non-communicable maladies. The obesity epidemic is affecting all age groups and among them children are given more attention nowadays because childhood overweight leads to obesity in adulthood. Overweight and obesity can be expressed as “abnormal or excessive fat accumulation that may impair health” [1]. Obesity is a major risk factor for the development of cardiovascular disease [2], type 2 diabetes and other metabolic syndromes [3]. Obesity is considered a landmark in rising double burden stress on global societies. The western societies believe thinness is an important factor for one’s personality that results in the development of sense of inequity and deprivation in the obese subjects, especially in women. Weight management is a complex mechanism that is influenced by physiological, genetic, societal, behavioral and environmental factor [4]. The occurrence of overweight and obesity is increasing in developing countries, and even in low-income groups in developed countries. A combined approach to the causes of unhealthy food habits and reduced physical activity may contribute to reducing the future burden of non-communicable diseases like obesity (WHO). At individual/personal level different type of signals are generated within the brain which includes neural, hormonal, nutritional and metabolic to produce changes in manners of eating, physical activity and metabolism to maintain energy balance in the body. Various studies have been conducted to know mechanism and reason of weight gain. A study suggested that there are about 200 genes and loci associated to the obesity in humans [5]. Excessive accumulation of adipose tissue in the abdominal region is an independent and more cardio metabolically relevant risk factor than general obesity [6]. Fat deposition at abdominal region is called abdominal obesity. It is further categorized into subcutaneous and visceral. Several studies have been postulated that elevated accrual of abdominal adipose tissue, particularly visceral fat has significance in the progress of insulin resistance and glucose intolerance, and also a better interpreter of Cardiovascular Disease (CVD) and type 2 diabetes than generalized obesity [7]. Around the world in 2013 it was found that 42 million children under the age of 5 were overweight or obese. In 2014, more than 1.9 billion adults, 18 years and older, were overweight, of these over 600 million were obese, further more mentioned that out of the whole population in the world 13 % (11% of men and 15% of women) were obese in 2014 [1].
Worldwide, pervasiveness of overweight and obesity collectively rose by 27·5% for adults and by 47·1% in children between 1980 and 2013. The amount of overweight and obese persons amplified from 857 million in 1980, to 2.1 billion in 2013. Globally proportion of men who were overweight increased from 28·8% in 1980 to 36·9% in 2013 and the proportion of women who were overweight increased from 29·8% to 38.0% [8]. During 1980- 2013 in developed and developing countries, the rate of prevalence of overweight and obesity in men and women changed drastically. Previously men of developed countries were more overweight and obese than women, while in developing countries women found more overweight and obese than men and this connection prevailed in both developed and undeveloped countries [1]. There was seen a significant increase in trends of overweight and obesity between 1992 and 2002, but in developed countries condition changed, and has been slowed down in past ten years [8]. Public health interventions in combination of dietary modifications are required to tackle the growing burden of the obesity.
Situation in Pakistan
One of the major global health burdens is due to chronic Non Communicable Diseases (NCDs) which mainly include heart stoke, diabetes, cancer, respiratory diseases that accounts for 60% of the worldwide deaths [9]. Low and middle-income developing countries are being affected by NCDs in higher ratio posing a massive negative economic impact. These countries particularly India, Pakistan, Bangladesh, Sri Lanka, Nepal and Bhutan comprise of 25% world’s population and accounts for 80% of death due to NCDS Pakistan is ranked 8th number in diabetes prevalence and expected to replace 4th position by the year 2025 [10]. Hypertension is also posing stress to society but not as abruptly as diabetes. Pakistan is suffering with a huge load of child and maternal morbidity and motility along with other infections and nutritional deficiencies. According to the World Health Organization (WHO) the incidence of obesity in Pakistan was 2.1 times high in urban areas as compared to rural areas. Approximately 40% of the women (aged 25-64) in urban settings were more obese as compared to urban men. Focusing on younger Pakistanis, approximately 40% youngsters of age between 15-24 year were characterized as underweight (BMI 18.5). Underweight was found more common in rural areas than urban areas [1]. BMI recommendations were revised for the study of obesity for adults of Asia pacific region by world health organization and the International Obesity Task Force in February 2000 suggested people of pacific region overweight at BMI>23 and obesity at BMI>25. Asians tend to build up more abdominal fat being at lower BMI representing more risk of co-morbidities as compared to Europeans who have such risk at high BMI this difference lead to develop a lower cut-off point for Asian [11]. These adjusted lower cut-off points of BMI>23 for Asians would categorize fraction Pakistani adults as overweight which were declared normal weight in previous survey. This large fraction of population considered overweight and obese are posing a serious health burden in Pakistan. If the use of lower cut-off points becomes common in Pakistan this would contribute to promote healthy body size and weight related perceptions of the people. Health professional should be emphasized to put this into practice.
Measuring overweight and obesity
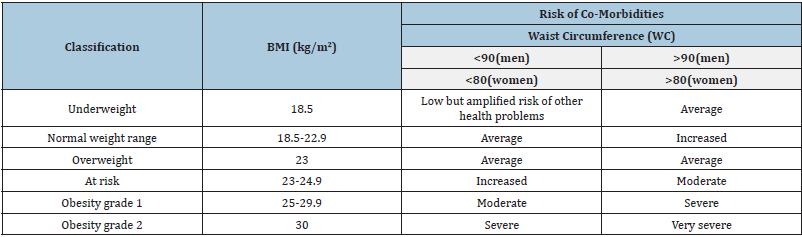
In recent years the global interest in measuring overweight and obesity has increased. The obese condition is measured using Body Mass Index (BMI), Waist Circumference (WC) and waist-to-hip ratio [12]. BMI is calculated by dividing weight in kilogram with height in meter squares. It is the most commonly used method around the world although it just represents the condition of excess of fat in the body, but it does not consider other factors like body composition and body shape. Besides these there are more reliable measuring instruments used to measure adiposity and body fat distribution like under water weighing, bioelectrical impedance computer tomography, magnetic resonance imaging and ultrasound [13]. But they are used in research and clinical setting because they are complex and expensive. According to WHO expert consultation, BMI classification is most likely to collapse in Asian populations where low BMI is common and people with low BMI comes with higher fat accumulation which in turns lead to risk of different chronic diseases [11]. Therefore, BMI alone cannot measure risk of obesity accurately. BMI use to measure excess weight relative to height while a person who is muscular means body builder may have higher BMI without having too much body fat. BMI should be used in conjunction with WHR. WHR is measured as WHR=(waist circumference in cm)/(hip circumference in cm). It is a marker of body fat allocation and shape of the body [12]. The Waist Circumference (WC) in cm has the most excellent anthropometric relationship with the quantity of visceral abdominal fat [14]. WC cut-points coupled with BMI to improve fortitude of health status. An elevated WC is a marker of quantity of abdominal fat, this applies to both male and female for the given value of BMI. Though the recommended cut-off points of BMI and WC are based on limited studies in Asians, but there is growing support for the use of BMI in conjunction with WC to more precisely conclude a person’s health risk irrespective of gender, ethnicity or age (Table 1).
Table 1: Suggested range of BMI and WC measurements to determine risk of co-morbidities in Asian population.
Factors Influencing Weight Gain
The upward trajectory of overweight and obesity in both developed and developing countries is associated with drift in behavioral, environmental and dietary habits instead of hereditary factors [4]. A shift in dietary choices from traditional fiber rich diets to energy-dense refined sugars and high fat diets are the main dietary factors responsible for increasing the obesity burden. Developing countries face “double burden” of health problems in terms of both undernutrition and overnutrition [15]. Obesity is directly associated with socioeconomic status and is more pronounced in wealthy communities [16]. Recent dietary trends originated from western countries such as use of high fat diet, junk food and restaurant eating coupled with physical inactivity have contributed a significant role in weight gain. Food consumption more than optimal energy expenditure need of body stores in storage cells i.e. muscles and adipose tissues with the passage of time and increase the likelihood of high plasma glucose, high cholesterol and blood pressure [17]. Subsequently these conditions lead to life threatening health problems including stroke, cardiovascular disease, type 2 diabetes and certain type of cancer.
Family
All physical and genetic characteristics inherent from parents to their offspring. Information present in genes influence the traits of an organism. Research have confirmed that obesity tends to prevail in families signifying role of genetics in obesity [18]. Families also share same lifestyle and dietary habits that may contribute to weight gain. Overweight and obesity affect both high-income and low-income families. Interestingly, people belonging to low-income families are at higher risk because they stuck to specific type of food especially in Asian countries, where carbohydrate is major source of energy specifically limited to starchy foods [11]. Therefore, Asians with low BMI have high amount of fat accumulation because excess carbohydrates store in body as fat. Whereas people of high-income countries have been found with excessive consumption of energy dense food i.e. fats, baked products, fried products, meat and soda than they require and have less physical activity due to which they gain weight [19].
Culture
Surrounding social culture also affect weight gain. Some cultures prefer fatty and sugar rich foods making hard to manage weight. Dietary habits of normal routine tend to deviate during family events and people usually consume large portion size of meals [20]. In Asian societies, including Arabs and sub-continent, mostly people overeat at marriage parties and other social gatherings. In near past, eating large portions was considered as a symbol of one’s physical strength. But now the trend is being changed and generally people become conscious about their portion size.
Socioeconomic status
Traditionally, obesity in developed countries was associated with wealth over the last 50 years. On the other hand, there is observed an inverse association between obesity and Socioeconomic Status (SES) in women compared to men [21]. People belonging to high SES have education, knowledge and resources which in turns impact their dietary choices and have less chances of obesity and related co-morbidities. While in developing countries obesity has seen with direct relationship with (SES) it is because people of developing countries especially Asian has staple food grains, carbohydrates source starch in them people who belong to high SES have resources money or may be educated as well but are physically inactive [11]. On the other hand, people of low SES have low resources are physically more active due to which bears low chances of becoming obese. Fast economic growth and social changes (e.g. sedentary lifestyles and the involvement of more women in the workforce) have led to an increased eat-out habits, which may contribute to the increased prevalence of obesity [22].
Sleep
Research have reported that incomplete rest and lack of sleep is associated with weight gain [23]. Recently, studies have found that insufficient sleep may make harder to lose weight. Obese or overweight when sleep late at night eat snakes and tend to accumulate more calories in their adipose tissues [24].
Obesogenic drugs
Certain drugs used in specific illness or disease strongly impact the health status of the person using these drugs. Currently, the trend of using anti-depressants and steroids is at peak. Instead of counseling people like to go for anti-depressants which in turn contribute to weight gain [25]. On the other hand, trend of having a muscular body is becoming common in young adults they make the use of several types of steroids which add to gaining weight and eventually lead to being overweight and later obese.
Obesity Associated Co-Morbidities
Obesity-induced hypertension
Hypertension is an ailment develops as a result of high Blood Pressure (BP), strongly correlated with increased Body Mass Index (BMI) [26]. Obesity is major risk for incidence of hypertension. Excessive fat is unswervingly associated with increased internal pressure, impaired pressure natriuresis, and hypertension. In addition to increased BP, increased cardiac output, heart rate as well as activation of the Sympathetic Nervous System (SNS) and Renin-Angiotensin-Aldosterone system (RAAS) are observed due to excessive weight in terms of fats. Increased visceral and retroperitoneal fat may increase BP by physically compressing the kidneys that gathers extra fat in and around the kidneys which cause increased pressure on kidney, impaired natriuresis, and hypertension [27]. Rapid weight gain also stimulates renal tubular sodium re-absorption, and obese individuals require higher than normal BP to maintain balance between intake and renal excretion of sodium indicating impaired renal pressure natriuresis [28]. Pressure natriuresis usually happens due to three factors which initially raise BP during rapid weight gain. These are increased SNS, activation of RAAS, and physically compress kidney due to fat deposition in and around the kidneys and excessive visceral fat. This is the mechanism which directly interacts with obese individual’s blood pressure. Hypertension is directly linked with BMI. It reveals that increased BMI increases the inclination of hypertension in both females and males [29]. Therefore, weight loss in beneficial strategy for treating hypertension. Obese individuals need immediate lifestyle modifications to maintain healthy body weight and loss the excess. Therapeutic approaches must be combined with dietary approaches coupled with routine workout by hypertension and other obesity induced metabolic disorders like diabetes mellitus, CVD, and cancer. These alignments will be treated in a better way.
Type 2 diabetes
Diabetes mellitus is a chronic, lifetime condition that affects body’s capability to use the food energy. There are three major types of diabetes prevailed in our civilization. Type 1 diabetes also called juvenile-onset diabetes, type 2 Diabetes originate in adults known as adult-onset diabetes, and pregnancy related diabetes called gestational Diabetes [30]. All types of diabetes have some common physiognomies. In general, our body breaks down food sugars and carbohydrates into simpler sugar glucose that acts as a fuel for body cells. But the body cells need hormone insulin for the glucose uptake and energy purposes. Due to diabetes mellitus, there are two possible body conditions either body does not make enough insulin or could not use the produced insulin [31]. The occurrence of worldwide obesity and Type 2 diabetes has increased and is predicted to rise to 30% of the global population [32]. Type 2 diabetes occur when body produces insulin, but body doesn’t use it effectively. Due to this insulin resistance glucose pile up in plasma instead of getting stored in cell and increase blood glucose level. Obesity is also a major contributor for insulin resistance [33]. Obese persons build up resistance to the cellular actions of insulin, characterized by an inability of insulin to restrain glucose release from the liver and to promote glucose uptake in fat and muscle. The disease doesn’t happen in one day. Body face this condition for countless time may be daily, every next day or whatsoever is the pattern. It has certain mechanism through which it causes damage to body and leads towards disease prognosis. The studies indicate strong relationship between gaining/losing weights with increasing/decreasing insulin sensitivity [34].
Glucotoxicity categorized by insulin resistance, firstly initiates with very little elevation in fasting glucose level which if prolonged causes amplified insulin secretion instead of causing a lack of it. For as long insulin resistance succeeds it results in mild hyperglycemia which in returns cause pancreas to secrete insulin excessively. This condition is categorized as “allostatic load”. Different studies have been done to know this mechanism. The conclusion drawn from these studies reveals that person who has normal tolerance for glucose uptake having high allostatic load and bears amplified risk of developing type 2 diabetes in comparison to the individuals with a decreased allostatic load [35]. Second culprit behind causing diabetes is Lipotoxicity. Acute or chronic elevation of fatty acid delivery to peripheral tissues might play a vigorous character in disturbing glucose storage and uptake by the muscle in the body [36]. Features of obesity-induced-diabetes are increased free fatty acid level in body that generate insulin resistance through intracellular metabolites which activate PKC (protein kinase C enzyme) leading to activation of serine/threonine kinase that inhibit insulin signaling [37]. Changes in the secretion of adipokines which amend insulin signaling also induce diabetes. Increased construction of inflammatory cytokines causes inhibition of insulin signaling by adipose tissues which contribute to diabetes mellitus. Endocrine and inflammatory mediators congregating serine/threonine kinases that obstruct insulin signaling and leads towards diabetes. Obesity-induced stimulation of NF-κB hoist inflammatory accounts which exacerbate insulin resistance. Adipokines persuades proteins SOCS family, basis insulin resistance either by intrusive with IRS- 1 and IRS-2 tyrosine phosphorylation or by directing IRS-1 and IRS-2 for proteasomal degradation also leads towards diabetes [38]. Augmented fatty acids also excite insulin resistance by direct activation of TLR4 and the innate immune response. Obesity-linked modification in the central response to hormonal and nutrient signals changes peripheral insulin sensitivity [39]. Higher lipid profile basis augmented production of Reactive Oxygen Species (ROS) which cause disparity between construction of highly reactive oxygen species and antioxidants action in body [40]. Besides these endocrine mechanism’s other factors like sedentary lifestyle, aging, environmental factors, genetic and behavioral factors like stress, alcohol consumption and smoking are contributor for developing type 2 diabetes.
Cancer
Cancer is a serious health problem and considered first cause of death in developed countries while second cause in developing countries [41]. Overweight and obese individual are at greater risk of cancer development. Surveillance, Epidemiology, and End Results (SEER) Program of NIC in United States identified 34,000 cases of cancer among men and 50,500 cases among women caused due to obesity during the year 2007. Obesity is associated with cancer; however, modest weight loss in the 5%-10% range, and above, can significantly improve health-related outcomes [42]. The pathophysiology of obesity induced cancers vary from person to person, however, around 40% obese patients are at higher risk for the development of endometrial, esophageal and adenocarcinoma. It is predicted that global health burden of cancer due to obesity will be increased by the year 2030 leading to 500,000 cases of cancer [43]. In clinical settings, Body Mass Index (BMI) is an adequate indicator to predict overweight or obese state but could not measure obesity induced internal metabolic changes which may be involved in carcinogenesis. The presence of metabolic syndrome especially combination of central adiposity, hypertension, dyslipidemia and hyperglycemia is a strong qualitative indicator showing obesity potential to induced cancer [44,45]. Adipose tissue is an active endocrine and metabolic organ that is chiefly composed of preadipocytes, adipocytes, macrophages, fibroblasts and blood vessels.
Several active adipokines like adiponectin, leptin, Plasminogen Activator Inhibitor (PAI)-1, Interleukin (IL) -6 and tumor necrosis factor-alpha (TNF-α) are released by adipocytes. During obese state size of adipocytes enlarges (hypertrophy) and expended adipose tissues release chemotactic factors like Monocyte Chemo- Attractant Protein (MCP)-1that attract macrophages resulting in adipose tissues inflammation [46,47]. The consequent increased production of adipokines and pro-inflammatory cytokines [48], whereas reduction in adiponectin production and adipose tissue incapability to store excessive Free Fatty Acids (FFA) leads towards FFA’s oxidation [49]. Obesity induced low-grade inflammation results in adipose tissues dysfunction which is a key factor for carcinomas development [50].
The enlarged adipose tissues suffer from hypoxia due to poor oxygenation that result in chronic inflammatory response of adipose tissues. The relative state of hypoxia activates Hypoxia- Induced Factor (HIF)-1 α to regulate oxygen homeostasis. On the other hand, HIF-1 α upregulate expressions of IL-6 and leptin while downregulate adiponectin production that stimulates inflammatory response via macrophages accumulation in adipose tissues. In addition, obese individuals commonly suffer from insulin resistance and release insulin in augmented levels to turn away hyperglycemia. Higher levels of insulin in blood circulations results in the production of Insulin-like Growth Factor (IGF) -1 in excess amounts that is related with genetic mutation which favors carcinogenesis [51]. Similarly, overexpression of serine protease inhibitor PAI-1 in visceral adipose tissues is involved in obesityrelated multiple types of cancer [52]. Genetic factors of cancer are complex and difficult to address. However, modifiable risk factors such as environmental, behavioral and dietary factors should be focused to reduce the risk of obesity associated cancer.
Cardiovascular diseases
Several epidemiological studies reported that obesity have strong association with cardiac unrest in several ways. Obesity linked comorbidities like metabolic syndrome including hypertension, glucose intolerance and dyslipidemia coupled with sleep disorders might be indirectly initiate heart problems [53]. Central or abdominal obesity allocates more fatty mass chiefly in abdominal region than the extremities and hence, increasing the chances of metabolic syndrome and cardiac events. Waist circumference and waist–hip ratio are popular indicators to assess the fatty mass allotment in visceral region and additionally indicate the risk of cardiovascular events. Inflammation markers and prothrombotic state are more pronounced in obesity especially abdominal adiposity. In obese individual after food intake blood flow in adipose tissues increases up to 10-folds than the fast state blood flow rate (2-3mL/100g/min). Afterward, these adipose tissues initiate local response to release adipokines, which is a primary event to damage adjacent myocardial cells. The secretion of adipokines, hormones, binding proteins and inflammatory markers like Interleukin-6 (IL-6), Plasminogen Activator Inhibitor-1 (PAI- 1), Tumor Necrosis Factor-Alpha (TNF- α) is stigmatized in obese patients [54]. The amplified concentrations of pro-inflammatory markers along with prothrombotic state induce endothelial cells damage and Vascular hypertrophy [55].
Obesity induced hypoventilation syndrome (sleep apnea) is also associated with heart health damage. Obese individuals have higher metabolic activities due to adipose tissue and require more cardiac output to meet metabolic demand. The heart maintains increased stroke volume by dilation of left ventricular chamber to increase venous return but sequentially, develops eccentric type of hypertrophy due to prolonged stress kept on the walls of normal heart [56]. The increased cardiac output and venous return enlarges left atrium in obese individuals [57]. Cardiomyopathy is another heart problem which have direct association with obesity. Primarily, the accumulation of fat content in heart tissues is boosted by metaplastic phenomenon while infiltrative process is downregulated. Ultimately, deposition of triglyceride in nonfat heart muscle cells (myocytes) causes cell unrest or dysfunction due to lipotoxicity [58]. In addition, in some cases heart myocardial tissues stripe with irregular bands of adipose tissues which may leads towards pressure-induced atrophy of the myocardial tissues. This phenomenon is more pronounced in some heart tissues like sinus node, atrioventricular node, myocardium near the atrioventricular ring and right bundle branch that can be replaced by fat cells in obese individuals [57]. CVD is related to abdominal obesity largely so one must focus on reducing the waist circumference along with maintaining healthy weight. Modifying the diet regarding carbohydrates (fiber rich) and focusing on Poly-Unsaturated Fatty Acids (PUFA) like omega-3 and omega-6 could benefit in reducing the chances of heart related problems in obese individuals.
Obstructive sleep apnea (OSA)
Obesity is considered a major risk factor for the development and succession of obstructive sleep apnea [42,59]. The Obstructive Sleep Apnea (OSA) affects obese individual two times more than normal-weight individuals. Furthermore, OSA is not limited to adults and older age obese subjects rather equally distributed in obese children. Results obtained from a clinical study reported that OSA was prevalent 46% among obese children as compared to lean children seen in a general pediatric clinic [60]. The deposition of fat at some specific sites in obese individuals may exacerbate OSA. The fatty mass developed in tissues surrounding the upper airway tract may predispose to apnea via narrowing the lumen and increasing chances of collapsibility of airway [61]. On the other hand, fatty mass deposition around the thorax cavity (truncal obesity) reduces functional residual capacity of lungs and increases oxygen demand that may lead to reduction in chest compliance [62]. In addition, OSA is more pronounced in subjects with visceral obesity. A convincing body of literature reported that visceral adiposity may dispose towards OSA, and this situation could be reversed by weight loss [63]. Factors like physical activity and reduction of high caloric diet especially refined carbohydrates should be promoted in order to minimize obesity induced OSA [64].
Gallbladder stones
In the human gastrointestinal tract, gallbladder is a small pearshaped sac like organ present underneath the liver that collect bile from liver. Hard particles/mass that develops in the gallbladder are called gallstones. The number of gallstones vary from a single large stone to many tiny stones or a combination of both large and small stones. These stones block ducts of billiard tract and are responsible for sudden pain (biliary colic) in the upper right abdomen [65]. Mechanisms through which obesity can cause gallstone disease to comprise the fact that obesity might boost hepatobiliary cholesterol efflux and hepatic de novo cholesterol synthesis, a key factor responsible for the development of cholesterol gallstones [66].
Reproduction related complications
Obesity negatively affect reproduction cycle and is a risk factor for infertility among both men and women [67]. Obesity dysregulate both natural and assisted conception cycles in women and reduces the rate of successful pregnancies. This condition could be partially restored with weight management. The complex mechanism of obesity induced anovulation is associated with insulin resistance in peripheral tissues [68]. Higher levels of insulin in vascular system reduces sex-hormones binding proteins release and increase levels of free insulin-like growth factor 1 and hyperandrogenaemia. The reduction of body weight at around 5% could contribute to reverse biochemical abnormalities and increase in ovulation rates. Furthermore, lower levels of adiponectin and higher levels of leptin in obese women are also related with reduced conception rates, however, there is very less information available on their role [69]. In addition to irregular ovulation, inferior quality oocyte production and incapability of endometrial wall receptivity further amplifies the risk of miscarriage in obese women [70]. In comparison to defective reproduction cycle in obese women, there is less information about direct effects of obesity on male fertility. Scientific literature reported that obese men have lower levels of total and free testosterone but there is no significant impact of obesity on semen quality and fertility rate [71]. However, obese women are at greater risk of pregnancy related complications than their lean counterparts [72]. To avoid such situation, one must plan pregnancy after achieving normal body weight or should have complete tract over pre pregnancy weight.
Conclusion
With the increase in urbanization and modernization obesity has become a serious issue of both developed and underdeveloped countries. Risk of chronic diseases due to genetic factors is less as compared to environmental, behavioral and dietary factors. Developed countries face problem due to high fat (junk food) and sugar containing food (refined carbohydrates) consumption along with amplified consumption of alcohol and smoking. Awareness regarding food choices must be provided and public counseling sessions must be conducted to lessen the rising trend of obesity. Dietary changes like replacing high fat and sugar containing food with high fiber, low sugar and fat diet would impact health status of the individuals in positive way by decreasing risk of chronic diseases. In underdeveloped countries issue of obesity is gaining strength along with under nutrition because of rising poverty in these countries like Pakistan, India, and Bangladesh where most of the population is under poverty line and has staple food from starchy grains [73,74]. A blend of nutrients instead of consuming single group should be preferred. People who belong to high socioeconomic status in these countries must add physical workout in their routine life. Health screening programs must be introduced to address the issues and point out the individuals. Public service massages must be delivered for the awareness of the population via text messages or television commercials. School teachers must be guided to provide information regarding healthy body weight and eating. All mentioned recommendations if implemented could help the community. In this way obesity and its adverse effect on health could be controlled.
Suggestions
On individual level daily physical activity of 30-45 minutes must be included, refined carbohydrates consumption must be reduced. Consumption of high fiber carbohydrates fresh fruits and vegetables must be increased. In youngsters and teenagers time spent on television cartoons, video games must be reduced by parents and child asked to incorporate this time in engaging in outdoor sports. Larges spaces along the roadside must be provided for the pedestrians to walk. Community wise health campaigns must be introduced along with the use of mass media. Improving or creating community access to playgrounds will increase people attraction towards physical activity. Sign boards can be used any other thing which people mostly use like accelerators and elevators must have the message for the people to use stairs. Decreasing the use of energy drinks soda’s cola and other sweetened beverages and encouraging the use of simple water is associated with lower body weight and BMI.
References
- World Health Organization (2015) Obesity and overweight.
- Mathieu P, Pibarot P, Larose E, Poirier P, Marette A, et al. (2008) Visceral obesity and the heart. Int J Biochem Cell Biol 40(5): 821-836.
- Ekpenyong CE, NE U, Akpan EE, Samson TK (2012) Double burden, non-communicable diseases and risk factors evaluation in sub-Saharan Africa: The Nigerian experience. European Journal of Sustainable Development 1(2): 249-270.
- Greenway FL (2015) Physiological adaptations to weight loss and factors favouring weight regain. Int J Obes (Lond) 39(8): 1188-1196.
- Pérusse L, Chagnon YC, Weisnagel J, Bouchard C (1999) The human obesity gene map: the 1998 update. Obes Res 7(1): 111-129.
- Ali O, Cerjak D, Kent JW, James R, Blangero J, et al. (2014) Obesity, central adiposity and cardiometabolic risk factors in children and adolescents: a family‐based study. Pediatr Obes 9(3): e58-e62.
- Bergman RN, Kim SP, Hsu IR, Catalano KJ, Chiu JD, et al. (2007) Abdominal obesity: role in the pathophysiology of metabolic disease and cardiovascular risk. Am J Med 120(2): S3-S8.
- Ng M, Fleming T, Robinson M, Thomson B, Graetz N, et al. (2014) Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 384(9945): 766-781.
- Boutayeb A, Boutayeb S (2005) The burden of non-communicable diseases in developing countries. Int J Equity Health 4(1): 2.
- Islam SMS, Purnat TD, Phuong NTA, Mwingira U, Schacht K, et al. (2014) Non‐Communicable Diseases (NCDs) in developing countries: a symposium report. Global Health 10(1): 81.
- World Health Organization (2000) The Asia-Pacific perspective: redefining obesity and its treatment. Health Communications Australia, Sydney, Austarlia.
- Ahmad N, Adam SIM, Nawi AM, Hassan MR, Ghazi HF (2016) Abdominal obesity indicators: Waist circumference or waist-to-hip ratio in Malaysian adults population. Int J Prev Med 7: 82.
- Hu FB (2008) Measurements of adiposity and body composition. Obesity Epidemiology pp. 53-83.
- Després JP, Lemieux I, Prud'Homme D (2001) Treatment of obesity: need to focus on high risk abdominally obese patients. BMJ 322(7288): 716-720.
- Bygbjerg IC (2012) Double burden of noncommunicable and infectious diseases in developing countries. Science 337(6101): 1499-1501.
- Dinsa GD, Goryakin Y, Fumagalli E, Suhrcke M (2012) Obesity and socioeconomic status in developing countries: a systematic review. Obes Rev 13(11): 1067-1079.
- Spiegelman BM, Flier JS (2001) Obesity and the regulation of energy balance. Cell 104(4): 531-543.
- Faith MS, Kral TV (2006) Social environmental and genetic influences on obesity and obesity-promoting behaviors: fostering research integration. In Genes, behavior, and the social environment: Moving beyond the nature/nurture debate. National Academies Press, USA.
- ALNohair S (2014) Obesity in gulf countries. International Journal of Health Sciences 8(1): 79.
- Berg C, Lappas G, Wolk A, Strandhagen E, Torén K, et al. (2009) Eating patterns and portion size associated with obesity in a Swedish population. Appetite 52(1): 21-26.
- Robertson A (2014) Obesity and inequities. Guidance for addressing inequities in overweight and obesity.
- Mohd SS, Lekhraj R, Foo CN (2021) Prevalence, associated factors and psychological determinants of obesity among adults in selangor, Malaysia. Int J Environ Res Public Health 18(3): 868.
- Chaput JP, Tremblay A (2012) Insufficient sleep as a contributor to weight gain: an update. Current Obesity Reports 1(4): 245-256.
- Lyytikäinen P, Rahkonen O, Lahelma E, Lallukka T (2011) Association of sleep duration with weight and weight gain: a prospective follow‐up study. J Sleep Res 20(2): 298-302.
- Kulkarni SK, Kaur G (2001) Pharmacodynamics of drug-induced weight gain. Drugs Today (Barc) 37(8): 559-571.
- Mertens IL, Van Gaal LF (2000) Overweight, obesity, and blood pressure: the effects of modest weight reduction. Obesity Research 8(3): 270-278.
- Saeed S, Ali A, Khawaja R, Shaikh IA, Shah I, et al. (2013) Relationship between BMI and blood pressure among students of 3rd year at Institute of Medical Technology (Duhs). Medical Channel 19(4).
- Hall ME, do Carmo JM, da Silva AA, Juncos LA, Wang Z, et al. (2014) Obesity, hypertension, and chronic kidney disease. Int J Nephrol Renovasc Dis 7: 75-88.
- Azizi A, Abasi MR, Abdoli GH (2008) The prevalence of hypertension and its association with age, sex and BMI in a population being educated using community-based medicine in Kermanshah: 2003. Iranian Journal of Endocrinology and Metabolism 10(4): 323-329.
- Mayfield JA (1998) Diagnosis and classification of diabetes mellitus: new criteria. Am Fam Physician 58(6): 1355-1362.
- Ozougwu JC, Obimba KC, Belonwu CD, Unakalamba CB (2013) The pathogenesis and pathophysiology of type 1 and type 2 diabetes mellitus. Journal of Physiology and Pathophysiology 4(4): 46-57.
- Martins IJ (2013) Increased risk for obesity and diabetes with neurodegeneration in developing countries. Journal of Molecular and Genetic Medicine. S1: 001.
- Hu E, Liang P, Spiegelman BM (1996) AdipoQ is a novel adipose-specific gene dysregulated in obesity. J Biol Chem 271(18): 10697-10703.
- Fruebis J, Tsao TS, Javorschi S, Ebbets RD, Erickson MRS, et al. (2001) Proteolytic cleavage product of 30-kDa adipocyte complement-related protein increases fatty acid oxidation in muscle and causes weight loss in mice. Proceedings of the National Academy of Sciences 98(4): 2005-2010.
- Tataranni PA (2002) Pathophysiology of obesity-induced insulin resistance and type 2 diabetes mellitus. Eur Rev Med Pharmacol Sci 6(2-3): 27-32.
- Kusminski CM, Shetty S, Orci L, Unger RH, Scherer PE (2009) Diabetes and apoptosis: lipotoxicity. Apoptosis 14(12): 1484-1495.
- Nandipati KC, Subramanian S, Agrawal DK (2017) Protein kinases: mechanisms and downstream targets in inflammation-mediated obesity and insulin resistance. Mol Cell Biochem 426(1-2): 27-45.
- Pessin JE, Kwon H (2013) Adipokines mediate inflammation and insulin resistance. Front Endocrinol (Lausanne) 4 :71.
- Shi H, Kokoeva MV, Inouye K, Tzameli I, Yin H, et al. (2006) TLR4 links innate immunity and fatty acid–induced insulin resistance. J Clin Invest 116(11): 3015-3025.
- Furukawa S, Fujita T, Shimabukuro M, Iwaki M, Yamada Y, et al. (2017) Increased oxidative stress in obesity and its impact on metabolic syndrome. J Clin Invest 114(12): 1752-1761.
- Parkin DM, Pisani P, Ferlay J (1999) Global cancer statistics. CA Cancer J Clin 49(1): 33-64.
- Fruh SM (2017) Obesity: Risk factors, complications, and strategies for sustainable long-term weight management. J Am Assoc Nurse Pract 29(S1): S3-S14.
- Engels EA, Pfeiffer RM, Ricker W, Wheeler W, Parsons R, et al. (2011) Use of surveillance, epidemiology, and end results-medicare data to conduct case-control studies of cancer among the US elderly. Am J Epidemiol 174(7): 860-870.
- Flegal KM, Carroll MD, Kit BK, Ogden CL (2012) Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA 307(5): 491-497.
- Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, et al. (2011) National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9·1 million participants. Lancet 377(9765): 557-567.
- Xu H, Barnes GT, Yang Q, Tan G, Yang D, et al. (2003) Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J Clin Invest 112(12): 1821-1830.
- Liu S, Umezu GM, Murph M, Lu Y, Liu W, et al. (2009) Expression of autotaxin and lysophosphatidic acid receptors increases mammary tumorigenesis, invasion, and metastases. Cancer Cell 15(6): 539-550.
- Skurk T, Alberti HC, Herder C, Hauner H (2007) Relationship between adipocyte size and adipokine expression and secretion. J Clin Endocrinol Metab 92(3): 1023-1033.
- Zhang Y, Daquinag AC, Amaya MF, Sirin O, Tseng C, et al. (2012) Stromal progenitor cells from endogenous adipose tissue contribute to pericytes and adipocytes that populate the tumor microenvironment. Cancer Res 72(20): 5198-5208.
- Zoncu R, Efeyan A, Sabatini DM (2011) mTOR: from growth signal integration to cancer, diabetes and ageing. Nat Rev Mol Cell Biol 12 (1): 21-35.
- Oskouian B, Sooriyakumaran P, Borowsky AD, Crans A, Dillard Telm L, et al. (2006) Sphingosine-1-phosphate lyase potentiates apoptosis via p53-and p38-dependent pathways and is down-regulated in colon cancer. Proc Natl Acad Sci U S A 103(46): 17384-17389.
- Liu Z, Yan R, Al Salman A, Shen Y, Bu Y, et al. (2012) Epidermal growth factor induces tumour marker AKR1B10 expression through activator protein-1 signalling in hepatocellular carcinoma cells. Biochem J 442(2): 273-282.
- Malik S, Wong ND, Franklin SS, Kamath TV, L’Italien GJ, et al. (2004) Impact of the metabolic syndrome on mortality from coronary heart disease, cardiovascular disease, and all causes in United States adults. Circulation 110(10): 1245-1250.
- Kern PA, Saghizadeh M, Ong JM, Bosch RJ, Deem R, et al. (1995) The expression of tumor necrosis factor in human adipose tissue. Regulation by obesity, weight loss, and relationship to lipoprotein lipase. J Clin Invest 95(5): 2111-2119.
- Rajendran P, Rengarajan T, Thangavel J, Nishigaki Y, Sakthisekaran D, et al. (2013) The vascular endothelium and human diseases. Int J Biol Sci 9(10): 1057-1069.
- Abel ED, Litwin SE, Sweeney G (2008) Cardiac remodeling in obesity. Physiological Reviews 88(2): 389-419.
- Poirier P, Giles TD, Bray GA, Hong Y, Stern JS, et al. (2006) Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation 113(6): 898-918.
- Zhou YT, Grayburn P, Karim A, Shimabukuro M, Higa M, et al. (2000) Lipotoxic heart disease in obese rats: implications for human obesity. Proceedings of the National Academy of Sciences 97(4): 1784-1789.
- Wolk R, Shamsuzzaman AS, Somers VK (2003) Obesity, sleep apnea, and hypertension. Hypertension 42(6): 1067-1074.
- Rudnick EF, Walsh JS, Hampton MC, Mitchell RB (2007) Prevalence and ethnicity of sleep-disordered breathing and obesity in children. Otolaryngol Head Neck Surg 137(6): 878-882.
- Romero Corral A, Caples SM, Lopez JF, Somers VK (2010) Interactions between obesity and obstructive sleep apnea: implications for treatment. Chest 137(3): 711-719.
- Parameswaran K, Todd DC, Soth M (2006) Altered respiratory physiology in obesity. Can Respir J 13(4): 203-210.
- Kritikou I, Basta M, Tappouni R, Pejovic S, Fernandez MJ, et al. (2013) Sleep apnoea and visceral adiposity in middle-aged male and female subjects. European Respiratory Journal 41(3): 601-609.
- Spiegel K, Tasali E, Penev P, Van Cauter E (2004) Brief communication: sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med 141(11): 846-850.
- Besselink MG, Venneman NG, Go PM, Broeders IA, Siersema PD, et al. (2009) Is complicated gallstone disease preceded by biliary colic? J Gastrointest Surg 13(2): 312-317.
- Noble F, Johnson C (2015) Gallstones. Medicine 43(11): 689-693.
- Pantasri T, Norman RJ (2014) The effects of being overweight and obese on female reproduction: a review. Gynecol Endocrinol 30(2): 90-94.
- Akamine EH, Marçal AC, Camporez JP, Hoshida MS, Caperuto LC, et al. (2010) Obesity induced by high-fat diet promotes insulin resistance in the ovary. J Endocrinol 206(1): 65-74.
- Lecke SB, Morsch DM, Spritzer PM (2011) Leptin and adiponectin in the female life course. Brazilian Journal of Medical and Biological Research 44(5): 381-387.
- Purcell SH, Moley KH (2011) The impact of obesity on egg quality. Journal of Assisted Reproduction and Genetics 28(6): 517-524.
- MacDonald A, Herbison GP, Showell M, Farquhar CM (2009) The impact of body mass index on semen parameters and reproductive hormones in human males: a systematic review with meta-analysis. Hum Reprod Update 16(3): 293-311.
- Catalano PM (2010) Obesity, insulin resistance, and pregnancy outcome. Reproduction 140(3): 365-371.
- WHO EC (2004) Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 363(9403): 157-163.
- World Health Organization (2003) Global strategy on diet, physical activity and health WHO, Geneva, Switzerland.
© 2021 Qamar Abbas Syed. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






