- Submissions

Full Text
Intervention in Obesity & Diabetes
Indigenous Plants of Odisha having Anti-Diabetic Activity: A Database
Pramathesh Mishra NT1, Mishra MK*2 and Mohapatra L3
1Mahatma Gandhi Institute of Pharmacy, Junabganj, Lucknow, Uttar Pradesh-227101, India
2Shambhunath Institute of Pharmacy, Jhalwa, Prayagraj, Uttar Pradesh-211015, India
3Amity Institute of Pharmacy, Lucknow, Amity University Uttar Pradesh, Noida -226010, India
*Corresponding author:Manoj Kumar Mishra, Shambhunath Institute of Pharmacy, Jhalwa, Prayagraj, Uttar Pradesh-211015, India
Submission:April 07, 2021;Published: May 03, 2021

ISSN 2578-0263Volume5 Issue2
Abstract
Diabetes mellitus consists of a group of syndromes characterized by hyperglycemia; altered metabolism of lipids, carbohydrates, and proteins; and an increased risk of complications from vascular disease. Diabetes mellitus, is associated with an increase in the blood sugar level beyond the threshold (hyperglycemia) and overflow in of excess sugar into urine (glycosuria). diabetes is the damage to micro capillaries (small blood vessels) of two vital organs-eyes & kidneys, leading to impaired vision and diseases of kidney. In this present review we are providing a brief descriptive data of various indigenous anti-diabetic plants grown at Odisha state, India.
Keywords:Diabetes mellitus; Hyperglycemia; Indigenous plants; Odisha; Antidiabetic
Introduction
Diabetes mellitus (“Madhumeha”) consists of a group of syndromes characterized by hyperglycemia; altered metabolism of lipids, carbohydrates, and proteins; and an increased risk of complications from vascular disease. The ancient Ayurveda documentation had a detailed record of this clinical syndrome with its suggested control and cure since three thousand years. Diabetes is of two types: Diabetes insipidus & Diabetes mellitus; both associated with excess and frequent urination (polyuria), nonetheless vary with regards to the causal mechanism. The former type is due to the deficient secretion of the Anti-Diuretic Hormone (ADH) resulting in passage of a very large volume of very dilute urine. ADH is secreted from the posterior lobe of the pituitary gland and it controls the secretion of urine by the kidney and thus regulates the water and electrolyte balance of the body fluids. The more common form of Diabetes, otherwise named as Diabetes mellitus, is associated with an increase in the blood sugar level beyond the threshold (hyperglycemia) and overflow in of excess sugar into urine (glycosuria). The term diabetes mellitus hails its origin from a Greek word “diabainess” which means “to pass through” and a Latin word “mellitus” meaning “sweetened with honey”. This disorder is due to the metabolic deficiency of insulin production in the body. The hormone insulin, which is a soluble protein with a molecular weight in solution of 48,000, is secreted from the β cells of Langerhans in the pancreas. It regulates the glucose concentration in the blood by (1) increasing the withdrawal of glucose from the body fluid and (2) decreasing the rate of addition of glucose to the body fluids. The possible causes of diabetes may be due to one or more of the followings:
a.Sedentary lifestyle
b.lack of regular physical exercises
c.rich food habit
d.obesity etc.
The primary detectable effect (symptoms) is the increase volume of urine (to discharge glucose) causing excessive thirst. Nevertheless, the secondary effects on body chemistry are more serious and severe. Because glucose is not available for oxidation, fat is burnt as fuel instead for giving energy and hence the patient loses weight. Glucose is not being burnt; fat combustion (oxidation) stops halfway resulting in accumulation of intermediate products (ketone bodies) in sufficient amount to become poisonous. This causes severe acidosis and finally coma leading to mortality. Besides, body proteins, like fats, are also burnt for energy as a result of which muscles and other tissues are weakened. Another dangerous effect of diabetes is the damage to micro capillaries (small blood vessels) of two vital organs–eyes & kidneys, leading to impaired vision and a form of Bright’s disease of the kidney. Interference with blood supply may account for the degeneration of nerves of the limbs causing pain, tingling and numbness. Another common complication is a sharp drop in the body’s resistance to combat diseases due to microbial infections.
Acacia farnesiana
Acacia farnesiana is commonly known as sweet acacia, Farnese wattle, dead finish, mimosa wattle, mimosa bush, prickly mimosa bush, prickly Moses, needle bush, north-west curara, sheep’s briar, sponge wattle, sweet acacia, thorny acacia, thorny feather wattle, wild briar, huisache, cassie, cascalotte, cassic, mealy wattle, popinac, sweet briar, Texas huisache, aroma, cashia, opoponax, sashaw, Aroma amarilla, suntich, sassie-flower, iron wood, cassie flower, honey-ball, casha tree, casha, cassia, Ellington’s curse, cushuh, huizache (Figure 1). The Components include anisaldehyde, benzaldehyde, cumin aldehyde, benzyl alcohol, cuminyl alcohol, farnesol, methyl salicylate, geranial, geraniol, geranyl acetate, linalool, linalyl acetate, a-terpineol, nerolidol, 3-methyldec-3-enol, 3-methyldec-4-enol, o-ionone, B-ionone, nonadecane, and myrcene. Acacia farnesiana possess anti-inflammatory and antinociceptive properties. It belongs to the family Fabaceae. Its local name is Bilati-babul. The bark part of this plant contents tannin. It is used by the decoction of bark (5g)+2 black pepper seeds once in a day for 5 days. (Anonis, 1988; Demole et al., 1969; EI-Hamidi and Sidrak, 1970; Lawrence, 1984).The AF increased glucose uptake by isolated hemidiaphragm at a relatively higher concentration (40μg/ml). These results suggest a direct stimulatory effect of the fraction on glucose uptake without the involvement of insulin [1].
Figure 1: Acacia farnesiana.

Achyranthes aspera
Achyranthes aspera is commonly known as prickly chaff flower, devil’s horsewhip, apamarga. It is a species of plant in the Amaranthaceae family (Figure 2). It contents 27-Cyclohexylheptacosan-7-ol and 16-hydroxy-26- methylheptacosan-2-one 83 and 17- pentatriacontanol 84, β-sitosterol83,85, spinasterol a85, 3-Acetoxy-6 benzoyloxyapangamide 79, Strigmasta-5, 22- dien-3-β-ol, trans- 13-docasenoic acid, n-hexacosanylndecaniate, n-hexacos-17- enoic acid and n-hexacos-11- enoic acid and a new aliphatic acid, n-hexacos-14-enoic acid86, a new aliphatic dihydroxyketone, characterized as 36,47-dihydroxyhenpentacontan-4-one and tritriacontanol87, 4 methylheptatriacont-1-en-10-ol and tetracontanol-2 88, hexatriacontane, 10-octacosanone, 10- triacosanone and 4-triacontanone89, betain, betalaine and achyranthine90-94, flavonoids and alkaloids95, oleanolic acid96- 97, a number of oleanolic acid based saponins98-100 , saponin A and saponin B characterized as α-Lrhamnopyranosyl (1→4)-β-Dglucopyranosyl (1→4)-β-Dglucuronopyranosyl(1→3)-oleanolic acid and β-Dgalactoyranosyl (1→28) ester of saponin A101, β-Dglucopyranosyl ester of α-L-rhamnopyranosyl (1→4)-β-Dglucuronopyranosyl (1→3)-oleanolic acid and β-Dglucopyranosyl ester of α -L-rhamnopyranosyl (1→4)-β-D-glucopyranosyl (1→4) β-D-glucuronopyranosyl (1→3)-oleanolic acid, saponins102-103, sapogenin104, alkaloids105 and saponins106, bisdesmosidic triterpenoid saponins like β-d-glucopyranosyl-3β-[O-α-lrhamnopyranosyl-( 1→3)-Oβ-D-glucopyranuronosyloxy] machaerinate and β-dglucopyranosyl 3β-[O-β-d-galactopyranosyl- (1→2)-O-α-dglucopyranuronosyloxy]machaerinate107, ecdysterone108- 110, cardiac glycosides111 from different organs like leaves, shoots, roots, fruits, seeds The root part of the plant Achyranthes aspera contains triterpenoid saponins. It is used by the Paste of root (5g) before breakfast for 7 days (Abhijit Dey, July – August 2011).
Figure 2: Achyranthes aspera.

Aegle marmelose
Aegle marmelos L., commonly known as bael, also Bengal quince, golden apple, Japanese bitter orange, stone apple or wood apple. Bael is the monotypic genus Aegle (Figure 3). It is a deciduous shrub or small, upto 13m tall with slender drooping branches and rather shabby crown. The bael tree contains furocoumarins, xanthotoxol, methyl ester of alloimperatorin, flavonoids, rutin marmesin, essential oils [2-5]. Aegeline is a constituent that can be extracted from bael leaves. The phytochemicals such as lupeol, eugenol, citral, cineole and d-limonene present in A. marmelos possess antineoplastic effects. It is used by tender leaf juice (10ml) +2–3 drops of honey; twice daily on empty stomach. (Shahedur Rahman and Rashida Parvin, 2014 Feb)
Figure 3: Aegle marmelose.

Aervalanata juss
Aervalanata juss. (Amaranthaceae) locally known as ‘bui’. The plant is diuretic, used in lithiasis. The root is demulcent, diuretic, useful in strangury (Figure 4). The roots are used in the treatment of headache. It is valued for cough also as a vermifuge for children. The chemical constituents present in the plant include alkaloids (ervine, methylervine, ervoside, aervine, methylaervine, aervoside, ervolanine, and aervolanine), flavanoids (kaempferol, quercetin, isorhamnetin, persinol, persinosides A and B), methyl grevillate, lupeol, lupeol acetate benzoic acid, β-sitosteryl acetate and tannic acid. Aerva lanata is a rich source of flavanoids such as kaempferol , quercetin , isorhamneti , methyl grevillate , lupeol , lupeol acetate benzoic acid, β-sitosteryl acetate and tannic acid. The Pharmacological effects of this plant are diuretic, anti-inflammatory, hypoglycemic, anti-diabetic, antiparasitic, antimicrobial, hepoprotective, anti-urolithiasis, antiasthmatic, antifertility and hypolipidemic [6-8]. This plant belongs to the family Amaranthaceous. It is used by Root paste (5g); twice daily for 10 days. (Manoj Goyal, Anil Pareek, B. P. Nagori, and D. Sasmal, 2011 Jul-Dec).
Figure 4: Aervalanata juss.

Ailanthus excelsa
Ailanthus excelsa Roxb. (Simaroubiaceae) commonly known as Mahanimb. Different parts of this plant are used widely in traditional medicine for a variety of diseases (Figure 5). The bark is used as bitter, astringent, appetizer, antihelmintic, dysentery, skin disease, troubles of the rectum, and fever due to tridosha and allays thirst. It is also used in gout, rheumatism, dyspepsia, bronchitis and asthma. Ailanthus is used to cure wounds and skin eruptions as mentioned in traditional medicine. Stem bark extracts showed potent antibacterial and antifungal activities. The alcohol extract from leaf and stem bark exhibits remarkably high anti-implantation and early abortifacient activity [9,10]. The plant reported to contain chemical Constituents like Quassinoids, excelsin, glaucarubin, ailanthone, glaucarubinone, Glaucarubilone. Quassinoids. It is used by decoction of bark (20g)+ginger (10g) for 7 days (Shamkuwar PB et al.).
Figure 5: Ailanthus excelsa.

Alangium salvifolium
Alangium salvifolium has been used traditionally for treatment of various ailments. Almost every part of Alangium salvifolium including roots, leaves, stem and bark are used in the Ayurveda and Siddha systems of medicines for the treatment of various diseases (Figure 6). In modern scientific literatures, the plant has been reported to have potential efficacy against diabetes , peptic ulcer, arthritis, inflammation and anthelminthic activities etc. Alangium salvifolium is reported to contain various biologically active phytochemicals such as alangine, ankorine, tubulosine, alangicine, salsoline etc. Alangium salvifolium belongs to the family Alangiaceae. Alangium salvifolium has been used as traditionally laxative, antiepileptic, astringent, antiulcer, pungent, purgative, alleviates spasms, anthelmintic, emetic, antiprotozoa, hypoglycemic agent, skin diseases, leprosy, scabies and as contraceptives for pigs. Stem and root barks of Alangium salvifolium were screened for their helicon bactericidal activity. The root barks of Alangium salvifolium were used externally as an antidote against snake/ scorpion, rabbit, rat, dog bites. It contains primary metabolites like cephaeline, tubulosine, isotobulosine, psychotrine and alangiside in roots. Alkaloids A & B, Alangicine, dimethylpsychotrine, marckine, marckidine, lamarckinine in bark. Alangimarkine, ankorine, deoxytobulosine, alangiside, alangine, sterols and three triterpenoids cepheline, N-methylcephaeline, deoxytobulosine and alangiside in fruits and alangimarine, alamaninalangimaridine, emetine, cephaeline, psychotrine in seeds. Leaf leachate is used (twice daily). (Suresh ShravyaBalakrishnan Nair Vinod Christudas Sunil, December 2017).
Figure 6: Alangium salvifolium.

Allium sativum
Allium sativum is commonly known as Garlic (Rasuna). It belongs to the family Amaryllidaceae. It is having multiple beneficial effects such as antimicrobial, antithrombotic, hypolipidemic, antiarthritic, hypoglycemic and antitumor activity (Figure 7). Garlic’s principal medicinal uses are to lower blood pressure and cholesterol, fight infections, and prevent cancer. The active constituents are sulfurcontaining compounds that are rapidly absorbed and metabolized. Numerous studies suggest that garlic lowers total cholesterol concentrations by approximately 10%, favorably altering HDL/LDL ratios mild antihypertensive, lowering blood pressure by 5-7%, antidiabetic, blood sugar level, prevent some solid tumors. Therefore garlic is also effective in the cancer prevention. The other proposed uses of garlic include the hepatoprotective, antihelmentics, antiinflammatory, antioxidant, antifungal and wound healing. The bulb part is used after boiled in water & drink (twice daily). (Karin Ried and Peter Fakler, 2014 Dec).
Figure 7: Alium sativum.

Allium cepa
Allium cepa is commonly known as Allium ascalonicum L. (onion). It belongs to the family Liliaceae. It contain a good number of phytochemicals, most of which are hydrocarbons and their derivatives (Figure 8). These include: Dipropyl disulphide (which is used as a flavour compound), Allicin (which has antidiabetic, antihypertensive, antibiotic and antithrombotic activities), diathyl sulphide (which is of insecticidal property), Dimethyl disulphide (which is used as a gas odorant and in chemical synthesis), Mercaptopropane or propylmercaptan [11-13]. It contents polyphenols, yellow onions have the highest total flavonoid content. Red onions have considerable content of anthocyanin pigments. It is used by making the Juice of bulb (120gm) & drink twice a day. (Shinkafi SA et al., Sch. J. App. Med. Sci., 2013).
Figure 8: Allium cepa.

Aloe barbadensis
Aloe barbadensis is commonly known as Aloe vera (Gheenkumari). It belongs to the family Aloaceae (Figure 9). The fresh gel mainly consists of water, mesophyll cells, mannose, arabinose, xylose, mannose, galactose, glucose .Mucopolysaccharides are mainly present as acemannan calcium magnesium malic acemannan, isocitrate, raw materials ash content aloin. It is used as psoriasis vulgaris, skin moisturizer, type 2 diabetes, malignancies and immunodeficiency viruses, oral lichen planus infections, angina pectoris, ulcerative colitis, kidney stones, alveolar osteitis. Water extract of 150mg/kg of leaf is used for treatment (Oliver Grundmann, September 2012).
Figure 9: Aloe barbadensis.

Alstonia scholaris
Alstonia scholaris is commony known as Indian devil tree (saptaparna). It belongs to the family Apocyanaceae. The plant contains Iridoids, alkaloids, coumarins, flavonoids, leucoanthocyanins, reducing sugars, simple phenolics, steroids, saponins and tannins. Alstonia scholaris is a traditionally important medicinal plant (Figure 10). This evergreen tree is native to the Indian subcontinent and Southeast Asian countries. The plant is used in traditional, Ayurvedic, Unani, Homoeopathy and Sidhha/ Tamil types of alternative medicinal systems against different ailments such as asthma, malaria, fever, dysentery, diarrhea, epilepsy, skin diseases, snakebite etc. Among the phytochemicals, alkaloids are mostly reported. The plant has been reported extensively as anticancerous, antimicrobial, molluscicidal, anxiolytic and antipsychotic agent. Alstonia scholaris is useful in treating malaria, abdominal disorders, dyspepsia, leprosy, skin diseases, tumors, chronic and foul ulcers, asthma, bronchitis, helminthiasis, agalactia, and debility. Preclinical studies have shown that it possesses anti-microbial, anti-diarrhoeal, anti-plasmodial, anti-oxidant, anti-inflammatory hepatoprotective, nootrophic, anti-stress, anti-fertility, immunomodulatory, analgesic, anti-ulcer, wound healing, anti-cancer, chemopreventive, radiation protection, radiation sensitization, and chemosensitization activities. Its bark is used by decoction of 60gm dried stem bark & 120ml given twice daily. (Khyade and Vaikos, NP November, 2009).
Figure 10: Alstonia scholaris.

Azadiracta indica
Azadiracta indica is commonly known as Melia azadirachta (nimba). It belongs to the family Meliaceae. The plant product or natural products show an important role in diseases prevention and treatment through the enhancement of antioxidant activity, inhibition of bacterial growth, and modulation of genetic pathways (Figure 11). The most important active constituent is azadirachtin and the others are nimbolinin, nimbin, nimbidin, nimbidol, sodium nimbinate, gedunin, salannin, and quercetin. Leaves contain ingredients such as nimbin, nimbanene, 6-desacetylnimbinene, nimbandiol, nimbolide, ascorbic acid, n-hexacosanol and amino acid, 7-desacetyl-7-benzoylazadiradione, 7-desacetyl-7- benzoylgedunin, 17-hydroxyazadiradione, and nimbiol. Quercetin and ß-sitosterol, polyphenolic flavonoids, were purified from neem fresh leaves and were known to have antibacterial and antifungal properties and seeds hold valuable constituents including gedunin and azadirachtin. It’s 7 tender leaves are taken daily by decoction (60gm) of dried stem bark. (Alzohairy MA. 2016 Mar).
Figure 11: Azadiracta indica.

Materials & Method
Study area
Odisha is situated on the coast surrounded by the Bay of Bengal & i.e. 482km stretch of coastline with golden beaches, serpentine rivers, waterfalls, forest-clad blue hills of Eastern Ghats with rich wildlife. Odisha covers an area of 1, 55,707sq.Kms. It is the ninth largest state of India located in the south-eastern fringes of the country. It also houses the largest coastal lake in India-Chilka lake. Odisha has historically been an agricultural state and is a leading producer of agricultural products in India [14-17]. Common plant species in the state include: Azadiracta indica, Curcuma longa, Gymnema sylvestre, Aegle marmelose, Vinca rosea, Murraya koenigii etc.
Ethnobotanical survey
The use of plants in treatment of Diabetes has been noted in many of the ancient Indian literature. In the last few decades, the studies performed on the plants mentioned in the literature or were used traditionally for diabetes have been documented in this paper. A varying degree of anti-glycaemic activity was observed in all of the plants.
Result and Discussion
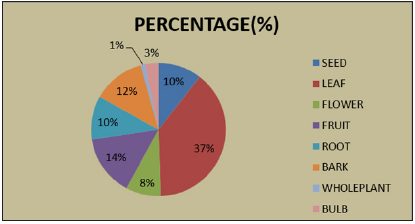
These enumerate the data obtained from different plant parts for Diabetes Mellitus. A total of 49 plant species belonging to 36 families have been recorded in the present study (Table 1). Plants like Aloe vera, Azadirachta indica, Momordica charantia, Gymnema sylvestre etc were more frequently used by the people. Bitter melon has been used in various Asian and African traditional medicine systems for a long time. It was found that Momordica charantia fruit powder is helpful in treating hyperglycemic rats in diabetes mellitus type II. Charantin has been extracted from the plant, which had hypoglycaemic effect on normal and diabetic rabbits. The usage of plant part Leaves -21 , Whole plant - 1, Seed -6 , Fruit -8 , Flower -5 , Bark -7 , Bulb -2are shown in Figure 12. From the data (Figure 12), it could be inferred that for a greater number of remedies are obtained from fresh leaf materials followed by fruits & amp; bark. However, plant parts like Flower, Whole plant and Bulb were less frequently used by the people.
Table 1: Analysis of remedies obtained from different plant parts for Diabetes Mellitus.
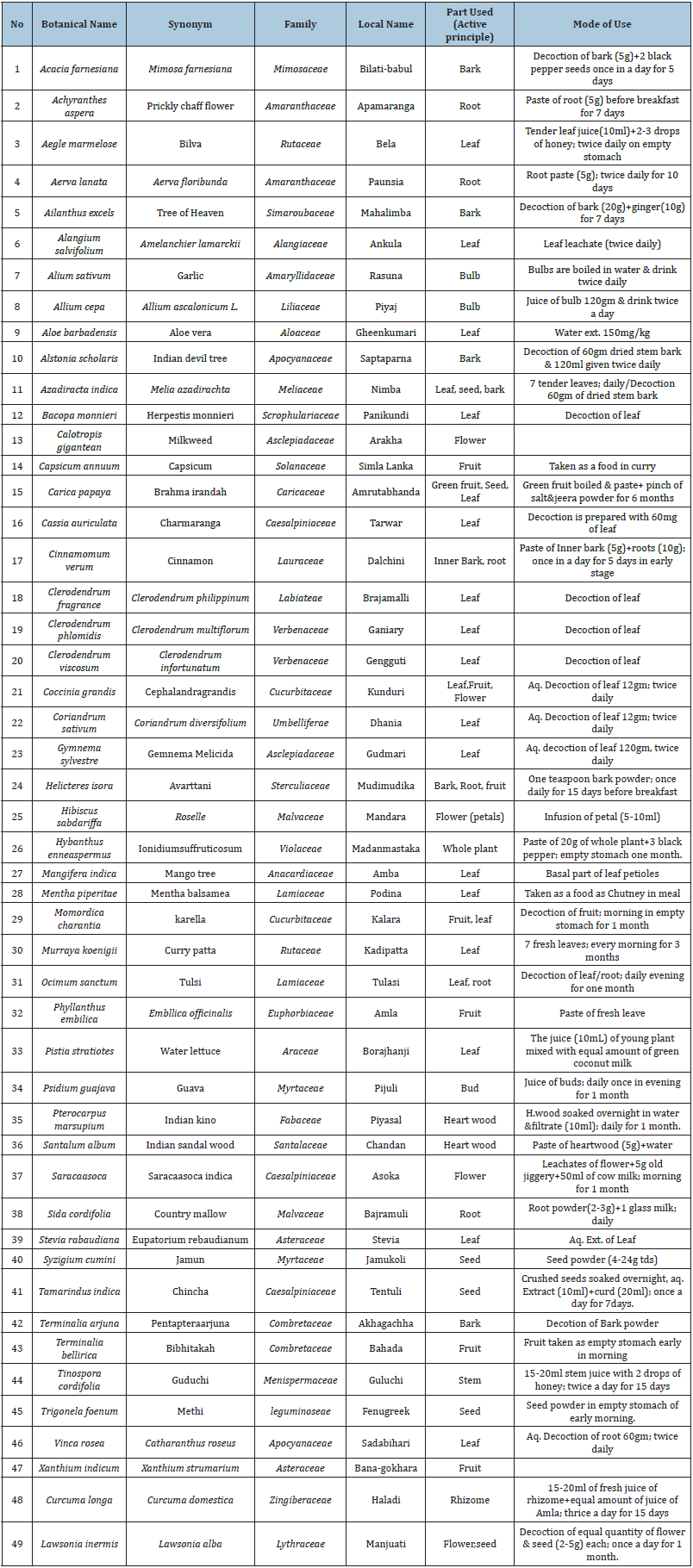
Figure 12: Chart showing the analysis of remedies obtained from different plant parts.
Conclusion
Though many plants have shown promising results as antidiabetic agents, their efficacy varies from patient to patient. As a result, clinical studies must be carried out in large populations (phase III trials) before any plant-based product can be introduced into clinical practice. Studies shall be designed to identify and determine any undesirable side effects that result from their consumption. Given that natural plant extracts are compositionallycomplex , great efforts towards the isolation, identification and purification of bioactive constituents must be undertaken. Other than an improved understanding, such knowledge will help to better identify and potentially predict incompatibilities if being used in combination with synthetic drugs. Finally, the use of plant products as adjutant to, or replacements for, synthetic drugs may substantially help in reducing the costs associated with treatment of DM. The results of our study demonstrated the persistence of folk medicine practices in Odisha , especially in rural people are still dependent on indigenous knowledge for health care that are being influenced by culture and socioeconomic aspects, providing a cheaper and accessible alternative to the high cost pharmaceutical remedies. In spite of the overwhelming influence and our dependence on modern medicine and tremendous advances in synthetic drugs, many people still relyon herbal drugs the reason is that, if the herbal medicines are used properly they don’t have any side effects. Hence, the survey need to be subjected to pharmacological studies in order to discover their true potential, as it is very difficult to judge the effectiveness of the herbal medicine. The main purpose is not to be prescribing any remedies for any of the disease but to be document the use and draw the attention of pharmacologist, botanist, phytochemist and pharmocognosist for further scientific research in the field.
References
- Estrada DE, Ewart HS, Tsakiridis T, Volchuk A, Ramlal T, et al. (1996) Stimulation of glucose uptake by the natural coenzyme alpha-lipoic acid/thioctic acid: participation of elements of the insulin signaling pathway. Diabetes 45(12): 1798-804.
- Bandawane D, Juvekar A, Juvekar M (2011) Antidiabetic and antihyperlipidemic effect of alstonia scholaris linn bark in streptozotocin induced diabetic rats. Indian Journal of Pharmaceutical Education and Research 45(2): 114-120.
- Tembhurne SV, Sakarkar DM (2009) Hypoglycemic effects of fruit juice of Murraya koenigii (L) in alloxan induced diabetic mice. Int J Pharm Tech Res 1(4): 1589-1593.
- Omonkhua AA, Onoagbe IO, Ajileye AF, Aladegboye LO, Adetoboye AR (2013) Long term anti-diabetic, anti-hyperlipidaemic and anti-atherogenic effects of carica papaya leaves in streptozotocin diabetic rats. European Journal of Medicinal Plants 3(4): 508-519.
- Alexiou P, Demopoulos VJ (2010) Medicinal plants used for the treatment of diabetes and its long-term complications. Plants in Traditional and Modern Medicine: Chemistry and Activity 69: 175.
- Anthony OE, Ese AC, Lawrence EO (2013) Regulated effects of Capsicum Frutescens Supplemented Diet (CFSD) on fasting blood glucose level, biochemical parameters and body weight in alloxan induced diabetic wistar rats. Journal of Pharmaceutical Research International 3(3): 496-507.
- Singh SN, Vats P, Suri S, Shyam R, Kumria MM, et al. (2001) Effect of an antidiabetic extract of Catharanthus roseus on enzymic activities in streptozotocin induced diabetic rats. Journal of Ethnopharmacology 76(3): 269-277.
- Aslam TM, Patton N (2004) Methods of assessment of patients for Nd: YAG laser capsulotomy that correlate with final visual improvement. BMC Ophthalmology 4(1): 13.
- Bailey CJ, Day C (1989) Traditional plant medicines as treatments for diabetes. Diabetes care 12(8): 553-564.
- Rai MK (1995) A review on some antidiabetic plants of India. Ancient Science of Life 14(3): 168-180.
- Patel DK, Kumar R, Laloo D, Hemalatha S (2012) Diabetes mellitus: An overview on its pharmacological aspects and reported medicinal plants having antidiabetic activity. Asian Pacific Journal of Tropical Biomedicine 2(5): 411-420.
- Wadkar KA, Magdum CS, Patil SS, Naikwade NS (2008) Anti-diabetic potential and Indian medicinal plants. Journal of Herbal Medicine and Toxicology 2(1): 45-50.
- Bastaki A (2005) Diabetes mellitus and its treatment. International Journal of Diabetes and Metabolism 13(3): 111-134.
- Sheng Ji P (2001) Ethnobotanical approaches of traditional medicine studies: some experiences from Asia. Pharmaceutical Biology 39(1): 74-79.
- Marles RJ, Farnsworth NR (1995) Antidiabetic plants and their active constituents. Phytomedicine 2(2): 137-189.
- Ignacimuthu S, Ayyanar M, Sivaraman SK (2006) Ethnobotanical investigations among tribes in Madurai district of Tamil Nadu (India). Journal of Ethnobiology and Ethnomedicine 2(1): 25.
- Singh SK (2017) Polypeptide-k as phytoinsulin: How much and how far. International Journal of Green Pharmacy 11(02).
© 2021 Mishra MK. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






