- Submissions

Full Text
Intervention in Obesity & Diabetes
Low Carbohydrate Lifestyle Reduces Significantly Insulin Need in Type 2 Diabetes Patients
Verkoelen H1*, Govers E2, Maas H3 and Koek GH4,5
1Primary Care Dietitian, Diabetes Nurse Specialist, The Netherlands.
2Primary Care Dietitian, President of Dutch Knowledge Centre for Overweight & Obesity, The Netherlands
3Department of Human Movement Sciences, Faculty of Behavioural and Movement Sciences, The Netherlands
4The Department of Internal Medicine, Division of Gastroenterology/Hepatology, The Netherlands
5School of Nutrition and Translational Research in Metabolism (NUTRIM), The Netherlands
*Corresponding author: Harriet Verkoelen, Primary Care Dietitian, Diabetes Nurse Specialist, Ridder Alartlaan 33, 4116 EH Buren, The Netherlands
Submission:July 31, 2020;Published: August 17, 2020

ISSN 2591-0263Volume4 Issue4
Abstract
Background
A low carbohydrate diet is suggested to be effective in type 2 diabetes to reduce or stop glucose lowering medication. To prove the effectiveness of this dietary change, a low carbohydrate diet was studied in patients with type 2 diabetes on the amount of insulin, HbA1c values and weight loss.
Methods
An observational study in one dietitian practice on the treatment of patients with type 2 diabetes, all on an insulin regimen, with a low carbohydrate diet. Two HbA1c values prior to, and after six months of the dietary intervention were measured. All patients received a dietary advice to consume 30 grams carbohydrates per day in a day menu schedule. Patients visited the outpatient clinic to discuss their results, experiences, and questions. The online treatment group received feedback every week and extra support per mail.
Results
We included 37 overweight type 2 diabetes patients on insulin treatment and evaluated 35 patients after 6 months. The consumption of carbohydrates was 31±10 grams per day. Insulin use was reduced significantly (p<0.001) from 62.6±46.4 IU to 1.4±6.4 IU per day. For 92% of the participants, insulin injections could be stopped completely. Patients lost a mean of 13.3±6.3 kg of weight and the mean HbA1c level declined from 63.4±11.0mmol/mol to 56.9±13.0mmol/mol (p<0.001).
Conclusion
A low carbohydrate dietary lifestyle is effective in improving HbA1c and weight loss and leads to a significant reduction of insulin need.
Abbreviations: HbA1c: Glycated Hemoglobin; IR: Insulin Resistance; T2DM: Type 2 Diabetes Mellitus; CH: Carbohydrate(s); NAFLD: Non-Alcoholic Fatty Liver Disease; NASH: Non-Alcoholic Steatosis Hepatitis; IU: International Units; LCHF: Low Carb High Fat
Introduction
The Western lifestyle, characterized by high caloric intake and reduced physical activity, is responsible for the increase of overweight and obesity. To date, more than 50% [1] of the adult Dutch population is overweight and this is an important factor in the development of the metabolic syndrome. The progressive fat accumulation in the visceral compartment and the liver causes insulin resistance (IR) leading to a reactive overproduction of insulin. This is the central driver in the aetiology and progression of type 2 diabetes (T2DM). It also leads to a low grade systemic inflammation that plays an important role in atherogenesis developing cardiovascular diseases [2-4] and non-alcoholic steatohepatitis (NASH) [5,6]. In the Netherlands, over 1.2 million persons have diabetes and in a growing number of patients, insulin is often added to the oral drug therapy. Diabetes has a serious impact on quality of life and health care costs. Prevention is an important issue and challenge, in which lifestyle interventions are crucial. Most diabetes guidelines primarily recommend starting with nutritional and physical activity lifestyle changes to reduce weight [7,8] and secondly if this fails, starting pharmacotherapy. In daily practice, more than 73% of the patients start with pharmacotherapy [9] because they fail to make changes in lifestyle and diet, and do not achieve weight loss.
Insulin is added to oral medication in a considerable number of patients (24%) [9] with T2DM because oral glucose lowering drugs do not lead to acceptable glucose and HbA1c levels. However, treating blood glucose levels is not going to prevent the development of vascular pathology in diabetes. This was confirmed in seven multinational, multi-center, randomized controlled trials of tight blood glucose control with medications (ACCORD, ADVANCE, VADT, ORIGIN, ELIXA, TECOS and SAVOR) [10-16]. They all failed to demonstrate reductions in heart disease, the major cause of death of persons with diabetes [17]. The 18-country observational Prospective Rural Urban Epidemiology (PURE) Study concluded that the total fat intake and types of fat (saturated, mono-unsaturated, poly-unsaturated) in a diet were not associated with cardiovascular disease, myocardial infarction, or cardiovascular disease mortality [18]. The biggest problem of diabetes pharmacotherapy with sulphonylureas and insulin is that it causes weight gain [19]. Weight gain is undesirable because 90% of patients with T2DM are overweight or obese already [19]. Weight gain and the development of atherogenesis is caused by the physiological role of insulin as an anabolic hormone. It plays a role in the conversion of carbohydrates (CH) into body fat. The more carbohydrates T2DM patients eat, the more fat synthesis insulin gives especially in those who are insulin resistant which is characterized by hyperinsulinemia. Guidelines advise patients to eat on average 150-250 grams of CH a day [20,21]. Because CH promotes insulin release, which causes fat storage, the advised amount of CH might not be ideal and even be counterproductive. Studies in which the amount of CH intake was reduced showed an improvement of T2DM [22-29]. Reducing CH intake is not only causing weight loss but also a decrease in IR. The hypothesis is that by introducing a CH low lifestyle in T2DM patients, glucose levels normalize, and weight loss will be achieved, resulting in a diminishing need for exogenous insulin. Therefore the aims of this study were to investigate the effects of a low carbohydrate diet on insulin need, HbA1c levels and bodyweight in patients with T2DM treated with oral medication and insulin therapy.
Methods
Study design
An analysis of retrospectively collected data from a group of T2DM patients taking a low CH diet that were on oral and insulin therapy. The data was collected from one dietary practice (Prima Vita, Buren, the Netherlands) that is specialized in the treatment of patients with T2DM during the period January 2016 to April 2017. The dietitian also has more than 25 years of experience as a trained nurse diabetes specialist.
Selection participants
We included 37 participants who met the inclusion criteria of: age between 18 to 75 years, T2DM on oral and insulin treatment, overweight (BMI>25kg/m2) and/or an abdominal circumference of ≧80cm in females and ≧102cm in males. Exclusion criteria were pregnancy and renal failure defined as calculated serum glomerular filtration rate under 30ml/min. Cardiac patients with heart failure and psychiatric patients with lithium medication were also excluded.
Dietary intervention
For motivation to join the low CH diet, all participants were informed about the relationship between carbohydrates, IR and the effects on metabolism, the amount of insulin needed and weight loss, that was found in scientific publications [23-29]. All patients had previously followed a low fat, high CH diet without improvement of the T2DM or weight loss. In a shared decision setting, patients freely chose to start with the low CH diet. Then, participants were instructed how to follow a low CH diet and encouraged to keep the CH intake between 30 and 50 grams a day, preferably around 30 grams a day. To achieve this, they were instructed to leave out products rich in CH like rice, pasta, potatoes, fruits and replace normal bread with low carb bread. They were advised to take a zero CH breakfast or up to 5 grams CH maximum. This was achieved by eating, for example, eggs, cheese and vegetables. Patients received a dietary advice in the form of a day menu. Furthermore, booklets with background information were provided. They were encouraged to ask questions to support them on the diet.
Tapering off T2DM medication
On the same day patients started making the dietary changes, the insulin dosage was stopped completely if the total amount of insulin was up to 30 IU. Insulin was lowered by half if the total amount of insulin was over 30 IU and lowered according to the scheme (Figure 1). In the first two days after tapering off or stopping insulin injections, the serum glucose levels were communicated by phone and if necessary, the medication was adjusted. Thereafter, a weekly based follow up by phone or email was organized. More frequently, when participants had questions or were uncertain about their serum glucose levels, a quick answer was provided. The first target was to stop the long term insulin therapy because this has most side effects on weight gain. Every one to two weeks, insulin therapy was lowered, and this was repeated until all insulin finally could be stopped when 10 or less IU daily therapy was achieved (Figure 1). For patients, seeing the result of using less or no insulin was a big motivational factor to continue with the low CH diet. For this reason, it was chosen to start the low carbohydrate diet from one day to another instead of lowering carbohydrates in phases. As soon as weight loss stagnated, or hypoglycemic episodes occurred, insulin was also lowered again. Next, when still on sulphonylureas, we started to taper and stop these oral drugs after stopping insulin also.
Monitoring
For follow-up, some of the participants visited the dietitian practice on a frequent basis, but most of them were monitored online via the dietitian’s own website, where they had an account [30]. They stayed in touch with their own physicians or diabetes nurses for their regularly scheduled check-ups. We measured weight, BMI, waist circumference, HbA1C and the amount of insulin used at baseline and after six months. All therapy changes and additional information was reported in participants files.
Statistical analysis
Changes in insulin, HbA1C, body weight and carbohydrate intake were analysed using paired t-tests. Differences were considered significant at p<0.05. Values reported are mean ± SD.
Figure 1:Abbreviations: S: <30gr CH/day. M: 30-50gr CH/day. L: 50-100gr CH/day.
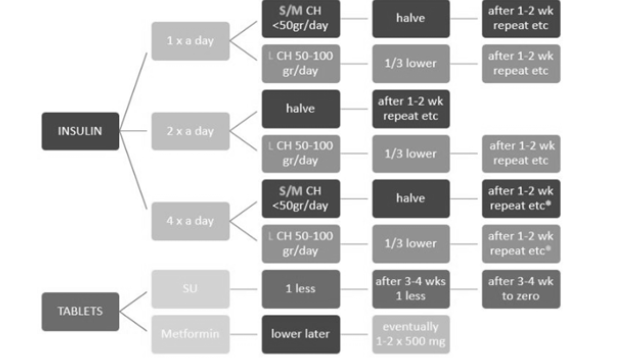
*In case of insulin four times a day: reduce everything by half (S/M) or reduce by 1/3 (L). After that, phase out the long term insulin, followed by the short lasting insulin. In case 8 IU or less are left then you can stop insulin totally after a few days. Goal is to stop all SU medication and insulin.
Results
Patient characteristics are summarized in (Table 1). Carbohydrate intake in all participants during the study period was 31±10g/day. Patients did not significantly change their physical activity during the diet period.
Table 1:Abbreviations: CH: Carbohydrates; IU: International Units; HbA1c; Glycated Hemoglobin, *=Significant p<0.05. Baseline and 6 month follow up characteristics of the T2DM study cohort using insulin therapy.
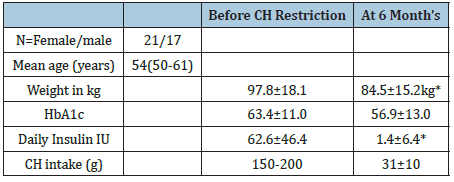
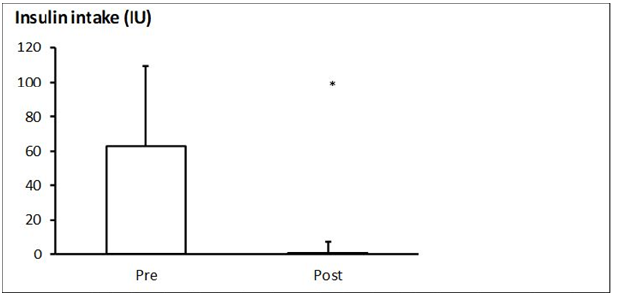
Insulin
Out of 37 T2DM patients, 35 could stop the insulin treatment after 1 to 12 weeks. Insulin intake decreased significantly (p<0.001) from 62.6±46.4 IU to 1.4±6.4 IU (Figure 1). Insulin intake could be stopped immediately in most participants, meaning the first day of starting the low CH diet. Within 3 months, all 35 patients stopped insulin. In the other two participants, the amount of insulin was substantially reduced. Stopping long term insulin first was our first goal [31]. One participant stopped insulin after using it for 25 years. At start, this person injected 250 IU per day and the HbA1c was 73mmol/mol. After 6 months HbA1c was 45mmol/mol. Body weight decreased from 102kg to 85kg. The patient has completely stopped injecting insulin for more than 3 years now.
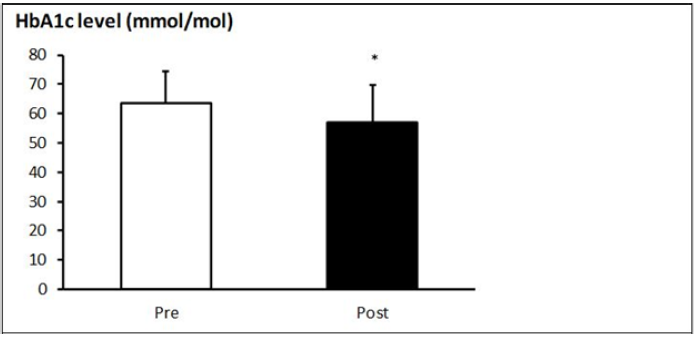
HbA1c
The HbA1c levels were decreased significantly (p<0.001) from 63.4±11.0 at start, to 56.9±13.0mmol/mol after six months (Figure 2). In 29 out of 37 patients, a decrease was found; in four patients, the levels were unchanged and in six, levels increased.
Figure 2:Insulin intake at baseline (pre) and 6 months after (post) the dietary intervention. Values are mean + SD (n=37). *Significant reduction.
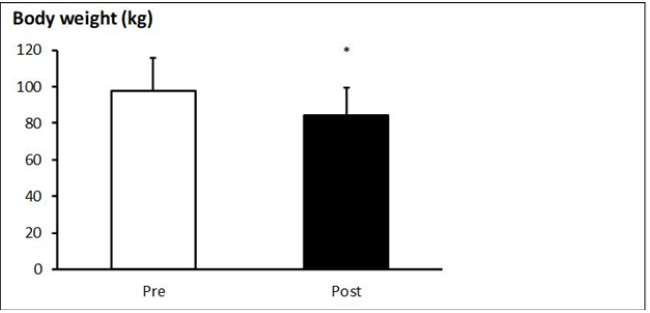
Body weight
Mean body weight of the participants decreased from 97.8±18.1 to 84.5±15.2kg (p<0.001). This is a mean weight loss of 13.3kg (-13.5%). In 3 participants, body weight after six months was unknown (Figure 3).
Figure 3:HbA1c levels at baseline (pre) and 6 months after (post) the dietary intervention. Values are mean + SD (n=37). *Significant reduction.
Carbohydrate intake
Carbohydrate intake in all participants during the study was 31±10g/day. There were participants who themselves lowered the carbohydrate intake to 15-20g/day.
Discussion
This observational study showed that a low CH diet in T2DM patients on oral and insulin therapy was able to reduce insulin need significantly. In 92% of the participants, patients stopped their insulin injections completely by lowering the CH intake to <40 grams. On average, this was achieved within a few weeks. This is remarkable because usually insulin doses are adjusted 2,4 to 6 units at a time. A complete stop of insulin injections hardly ever occurs in conventional diabetes treatment. The rationale behind this is the carbohydrate-insulin model of obesity, stated by Hall (2017) [32]. It theorizes that high-carbohydrate diets are fattening due to the elevation of insulin secretion following the high CH ingestion. Insulin, an anabolic hormone, directs the energy toward storage as fat in adipose tissue and prevents the oxidation by active tissues. In response, hunger and appetite increase and metabolism is suppressed. This leads to the development of overweight and obesity. However, there is debate if the reduction of insulin is due to weight loss and not due to the CH diet. It is obvious that weight reduction is essential for diminishing insulin resistance-an important factor in T2DM development associated with overweight and obesity. This study showed that already after start of the CH reduction, insulin need decreased even before weight loss was achieved. We chose to lower the CH intake rapidly instead of a gradual decrease over weeks or months. We advocate a quick reduction in carbohydrate intake, and we promote a low CH lifestyle because it motivates patients seeing the rapid effect in decreasing insulin need. Our findings are confirmed by the study of Avenell showing that low CH diets of less than 50 grams per day were more successful in lowering HbA1c after three months [29], and by the findings of the review by Sainsbury [26] who found similar results.
To monitor the rapid insulin decrease, avoiding complications, a close monitoring was organized in the beginning of the dietary change. An individualized approach was drawn up before the start in which short term insulin was stopped in a slower tempo of every three to four weeks then the once daily dose. Weekly contact with the dietitian was mainly web-based or on demand per mail or phone. This way, a safe situation could be created for every patient, which resulted in no complications, like severe hypoglycemia, occurring. A significant weight loss with a mean of minus 13.5% was achieved in 34 documented patients. Interestingly, the overall number of patients in this study had tried different weight loss strategies without success in the past. Nearly all patients previously followed a high CH low fat diet that resulted in weight gain mainly due to the increase of the abdominal fat compartment. This led to an increase in IR and thereby a higher need for more insulin. We suspect that T2DM patients are CH intolerant because of insulin resistance (IR). Weight loss is crucial for a better T2DM management because it decreases IR. The decrease in IR also has a positive effect on lowering the systemic inflammation that plays a role in comorbidities like cardiovascular disease, hypertension, dyslipidemia, kidney failure and NAFLD [5,6,29]. Taken together, lowering CH intake and stopping insulin injections while losing weight, improves T2DM more than sticking to guidelines that advise eating high CH [21,22] and adding diabetes medication. Considering the fact that most of our patients reached that objective, we argue that treatment of these patients, of whom 90% were overweight or obese, include lowering or stopping weight promoting medication, supported by a low CH lifestyle.
Another aspect in the management of T2DM is the long term control by measuring HbA1c. From experience over a long period of diabetes care, HbA1c and glycaemia improved when insulin dose increased, resulting in weight gain. In this study, a significant reduction of the HbA1c levels (Figure 3) was documented, although the study period of 6 months was rather short to evaluate the long term effect on glucose blood levels and diabetes control. Patients did not experience hyperglycemia complaints but did have a better health and much more energy. These results indicate that a change in the diabetes type 2 treating protocol should be considered. We should reconsider what should be treated: blood sugar levels and thus only symptoms, as we are doing now in conventional diabetes treating protocols, or the metabolic aspects. The results of our short time, small study, are similar to results of Virta Health [27]). They found that after 1 year, compliance to a very low CH lifestyle (less than 30 grams a day), was 85 %. This is higher than pharmacotherapy compliance with T2DM medication [7,9,23]. This study clearly shows the effects of a real life situation from one diabetes care center motivating patients to follow the low carbohydrate lifestyle. The long time experience of the diabetes healthcare worker being a dietitian and diabetes nurse at the same time made it possible to initiate, motivate and safely monitor T2DM patients on insulin therapy. The study is an observational report and not intended to be a randomized controlled trial. An important factor of the intervention was that was advised to the patients and not randomly selected. Only patients strongly motivated to stop their insulin injections, chose the low carbohydrate lifestyle because they experienced so many diets without success in the past. A lot of interesting data like for example lipid metabolism parameters, insulin levels, liver enzymes and caloric intake changes were not collected but will be interesting to study in future research.
However, this observational intervention study in a small group of diabetes patients clearly demonstrates the potential effects of a low CH diet on T2DM treatment and brings about the question if more focus should be put on dietary interventions and individualized therapy. The Western lifestyle is the main leading cause of the increase of overweight and obesity going hand in hand with an increase in the number of T2DM patients. Therefore, significant improvements could be achieved by a closer cooperation between dietitians, doctors and diabetes nurses to put more attention on demedicalisation by changing dietary habits as decreasing CH intake (Figure 1). A limitation of this study is the small number of patients included. Future studies should include larger populations. Most diabetes patients from this study stuck to the low CH lifestyle for they feel and understand the benefits every day. However, they experience challenging conditions when moments of stress or illnesses occur on special occasions like vacations. A difficulty in maintaining the low CH lifestyle is the abundance of carbohydrate rich processed foods that are marketed in a way that it is hard to resist them. This makes it probably harder to keep the diet for many years. More is needed to raise the awareness in policy makers and the food industry that large quantities of carbohydrates are not only on individual level but also in society unwanted and harmful. Long term studies are necessary to proof the effect on the long run and how it affects the general metabolic health of patients and society. The lowering carbohydrate approach will certainly decrease health care costs and improve quality of life (Figure 4). Therefore, future studies should be initiating measuring a broad range of consequences related to a low CH lifestyle like metabolic, psychological, healthcare, quality of life and costs aspects. Since hyperinsulinemia is the central driver of fat storage in insulin resistance and the development of comorbidities that goes along with hyperinsulinemia, measuring endogenous insulin should be part of diagnosing diabetes type 2, to hopefully prevent them from getting on insulin therapy in the first place.
Figure 4:Body weight at baseline (pre) and 6 months after (post) the dietary intervention. Values are mean + SD (n=34). *Significant reduction.
Conclusion
This study showed that a low carbohydrate dietary lifestyle of 31±10 g per day is effective in significantly improving HbA1c, weight loss and insulin need in T2DM patients on oral and insulin treatment. The Mindshift of not treating hyperglycemia but focusing on treating hyperinsulinemia was key. Applying this on a larger scale would result in more healthy patients and lower health care costs. These results indicate that more research, regarding this treatment method, has to be done on a larger scale, considering the impact it could have on the way diabetes type 2 is treated in modern society.
Acknowledgement
Harriet Verkoelen works as a primary care dietitian, also has a working experience as a diabetes nurse for 25 years and has no conflict of interest. Elisabeth Govers is president of KDOO (Kenniscentrum Diëtisten Obesitas en Overgewicht), a specialist network of obesity dietitians, and has no conflict of interest. Ger Koek is a gastroenterologist and hepatologist working in the field of NAFLD and has no conflict of interest concerning this study.
References
- Public Health Care.info. Summarized Overweight. Overweight> Figures & Context> Summary.
- Zarvaroni I, Bonora E, Pagliara M, Dall Aglio E, Luchetti L, et al. (1989) Risk factor for coronary artery disease in healthy persons with hyperinsulinemia and normal glucose tolerance. N Engl J Med 320(11): 702-706.
- Kraft JR (2011) Diabetes Epidemic & You.
- Reaven GM (1993) Role of insulin resistance in human disease (syndrome X): An expanded definition. Annu Rev Med 44: 121-131.
- Ahn J, Jun DW, Lee HY, Moon JH (2019) Critical appraisal for low-carbohydrate diet in NAFLD: Review and meta-analyses. Clin Nutr 38(5): 2023-2030.
- Mardinoglu A, Wu H, Bjornson E, Zhang C, Hakkarainen A, et al. (2018) An integrated understanding of the rapid metabolic benefits of a carbohydrate-restricted diet on hepatic steatosis in humans. Cell Metab 27(3): 559-571.
- NDF (2015) Standard of Care Diabetes.
- NHG (2018) Diabetes Mellitus Type 2.
- TNO (2017) Lifestyle as Medicine. Business Case for Type 2 Diabetes.
- Gerstein HC, Miller ME, Byington RP, Goff DC, Bigger JT, et al. (2008) Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 358(24): 2545-2559.
- Heller SR (2009) A summary of the ADVANCE trial. Diabetes Care 32(2): S357-S361.
- Duckworth W, Abraira C, Moritz T, Reda D, Emauele N, et al. (2009) Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med 360(2): 129-139.
- Hanefeld M, Bramlage P (2013) Insulin use early in the course of type 2 diabetes mellitus: The ORIGIN trial. Curr Diab Rep 13(3): 342-349.
- Seferovic JP, Bentley Lewis R, Claggett B, Diaz R, Gerstein HC, et al. (2013) Retinopathy, neuropathy, and subsequent cardiovascular events in patients with type 2 diabetes and acute coronary syndrome in the ELIXA: The importance of disease duration. Curr Diab Rep 13: 342-349.
- Bethel MA, Engel SS, Stevens SR, Lokhnygina Y, Ding J, et al. (2018) Progression of glucose-lowering diabetes therapy in TECOS. Endocrinol Diabetes Metab 2(1): e00053.
- Singh AK, Singh R (2017) SAVOR-TIMI to SUSTAIN-6: A critical comparison of cardiovascular outcome trials of antidiabetic drugs. SAVOR Expert Rev Clin Pharmacol 10(4): 429-442.
- Tim N (2017) Diabetes Unpacked. ISBN 9781907797583.
- Denghan M, Mente A, Zhang X, Swaminathan S, Li W, et al. (2017) Associations of fats and carbohydrate intake with cardiovascular disease and mortality in 18 countries from five continents (PURE): A prospective cohort study. Lancet 390(10107): 2050-2062.
- De Wit H, Vervoort G, Jansen H, Grauw WJC, Galan BE, et al. (2014) Liraglutide reverses pronounced insulin-associated weight gain, improves glycemic control, and decreases insulin dose in patients with type 2 diabetes (973-P). NED TIJDSCHR DIABET 12: 29.
- Reaven GM (2005) The metabolic syndrome: Requiescat in pace. Clinical Chemistry 51(6): 931-938.
- The Nutrition Center. Healthy Eating, Wheel of Five.
- Health Council of the Netherlands (2015) The Advice in Short.
- McKenzie A, Bhanpuri N, McCarter J (2017) Clinial trial update: 6 month outcomes in patients with type 2 diabetes. Virta.
- Unwin D, Guthbertson D, Feinman R, Sprung V (2015) A pilot study to explore the role of a low-carbohydrate intervention to improve GGT levels and HbA1c. Diabesity in practice 4(3): 102-108.
- Nielsen J, Joensson E (2018) Low-carbohydrate diet in type 2 diabetes: Stable improvement of bodyweight and glycemic control during 44 months follow-up control. Nutrition & Metablolism 5(14).
- Sainsbury E, Kizirian NV, Partridge SR, Gill T, Colagiuri S, et al. (2018) Effect of dietary carbohydrate restriction on glycemic control in adults with diabetes: A systematic review and meta-analysis. Diabetes Research and Clinical Practice 139: 239-252.
- Virta Health. The Virta Treatment is founded on decades of research and supported by ongoing clinical studies.
- Pot GK, Battjes Fries MC, Patijn ON, Pijl H, Witkamp RF, et al. (2019) Nutrition and lifestyle intervention in type 2 diabetes: pilot study in the Netherlands showing improved glucose control and reduction in glucose lowering medication. BMJ Nutrition, Prevention & Health.
- Avenell A, Brown TJ, McGee MA, Campbell MK, Grant AM, et al. (2014) What are the long‐term benefits of weight reducing diets in adults? A systematic review of randomized controlled trials. Journal of Human Nutrition and Dietetics 17(4): 317-335.
- Verkoelen H (2019) Viewed 16 December.
- Ryan DH, Yockey SR (2017) Weight loss and improvement in comorbidity: Differences at 5%, 10%, 15%, and over. Curr Obes Rep 6(2): 187-194.
- Hall KD (2018) A review of the carbohydrate-insulin model of obesity. Eur J Clin Nutr 72(3): 323-326.
© 2020 Verkoelen H. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






