- Submissions

Full Text
Intervention in Obesity & Diabetes
The Effect of Eating Habits on Sleep Quality in 19-24 Years Old Young Adult Women
Nazlı Nur Aslan Çin*, Hülya Yardimci and Ayşe Özfer Özçelik
Department of Nutrition and Dietetics, Turkey
*Corresponding author:Nazlı Nur Aslan Çin, Department of Nutrition and Dietetics, Ankara, Turkey
Submission:February 12, 2020;Published: March 02, 2020

ISSN 2578-0263Volume3 Issue5
Abstract
Objective: Having enough and quality sleep is important factors in all age periods. It is known that changes in eating habits have an influence on sleep quality in young adults. This study intends to investigate the impact of eating habits on sleep quality in women aged between 19 and 24.
Methods: The study was carried out with 412 university students staying in dormitory. The questionnaire involved general information about students, their eating habits, sleep duration, and Pittsburgh Sleep Quality Index (PSQI). The data was evaluated with appropriate statistical methods.
Result: The mean age was 20.7±1.4 years and BMI was 21.8±3.4kg/m2. 52.9% of the individuals skipped one of the main meals, the most frequently skipped main meal was lunch (65.5%). The most common reason why the subjects skipped breakfast, lunch, or dinner was found to be reluctance. 39.6% of those who woke up at night consumed any food or drink. The mean PSQI total score of the individuals was 7.86±2.75. While the sleep quality of 20.6% of the participants was good, 79.4% had poor sleep quality. There was statistically significant difference between sleep quality and the number of main meals and eating at night wake-up (p<0.05). While a positively significant correlation was determined between the sleep quality of participants and their BMI (p=0.03;r=0.11), a negatively correlation no significant difference was found between sleep duration and BMI (p=0.09;r=-0.08).
Conclusion: A significant portion of the students attending university and staying in dormitory was found to have sleeping disorders. The eating habits of students should be improved, and educational programs should be implemented to ensure adequate and balanced nutrition.
Keywords:Sleep duration; Sleep quality; Women; BMI; Nutrition habits
Introduction
The transition period to university is one of the critical stages in terms of gaining weight and fat since it also covers the adolescence period [1,2]. The students in this period are at risk in relation to nutrition and health [3]. This is due to some nutritional changes during this stage as a result of leaving the family, changing the settlement, and starting an independent life [4,5]. Most university students cannot afford the recommended dietary intake, and this results in unwanted weight gains [2,6]. The weight gain and changing eating habits during this period might lead to undesirable consequences in the later stages of life in terms of the development of certain diet related chronic diseases (obesity, cardiovascular diseases and type 2 diabetes) [7]. Increasing metabolic diseases and obesity prevalence cause significant reduction in sleep duration [8]. Sleep is a vital part of health affecting the life quality and wellbeing of individuals [9]. Most adults need 7-8 hours of sleep a day [8]. However, need for sleep may show variability depending on such individual and environmental factors as age, gender, physical activity, history of disease, emotional state, and lifestyle [10]. Sleep affects eating times as well as eating structure [11]. In addition, duration and quality of sleep is among the causes responsible for food consumption and weight gain. In a recent study, it has been determined that sleep duration is also affected by food consumption [12] and stated that a healthy diet could correct sleep deprivation [8]. One of the reasons for the increase in food consumption is inadequate or excessive sleep duration. Both of these conditions can adversely affect sleep quality [13]. Additionally, it has been stated that poor sleep quality might lead to weight gain, obesity, diabetes, cardiovascular diseases, physical diseases and decreased performance [14]. The relationship between decreased sleep duration and weight gain can be explained by a decrease in leptin hormone level activating the satiety signal and an increase in appetite-stimulating ghrelin hormone levels as a result of decreased sleep duration [13]. Some studies have indicated a significant relationship between both short and long sleep duration and body mass index (BMI) [15,16]. Sleeping less than six hours has an impact on obesity development by resulting in more adipose tissue development and weight gain [8,17]. Consuming energy rich food (high fat or refined carbohydrate-containing foods), skipping meals, and consuming inadequate vegetables may lead to less sleep duration [8]. It has been found in a study conducted in Japan that individuals who eat high fat, skip breakfast, eat mainly fast food, and usually eat out have shorter sleep durations [18]. Unfavorable conditions stemming from school exams, course schedules, and social circles in hostels and dorms may cause university students to experience sleep problems. Many recent studies have shown that eating habits have an effect on sleep durations. However, there are few studies in Turkey investigating the relationship between eating habits and sleep quality. For this reason, this study aims to investigate the effect of eating habits on sleep quality in young adult women aged between 19 and 24.
Materials and Methods
This study was carried out on 412 female university students aged between 19 and 24 staying in dormitories in Ankara province between December 2015 and May 2016. The Helsinki Declaration principles were followed in the study. The students were informed about the purpose of the study, and those who volunteered to participate were involved in the study. The data of the study were collected through face-to-face interviews using questionnaires prepared by the researchers. The questionnaire form consisted of general information about students, their height, body weight, eating habits, and the Pittsburg Sleep Quality Index (PSQI). The body weight (kg) and height (cm) measurements of the individuals were collected by the researches in accordance with general practices. Body Mass Index (BMI: kg/m2) was calculated for all individuals. According to the World Health Organization (WHO), BMI is classified as “thin” for less than 18.5kg/m2, “normal” for 18.5-24.9kg/m2, “overweight” for 25.0-29.9kg/m2, and “obese” for ≥30kg/m2. Later, 25.0-29.9kg/m2 and ≥30 kg/m2 categories were combined to make a single category as “pre-obese/obese” for ≥25kg/m2 [19].
PSQI was used for the evaluation of individuals’ sleep quality. PSQI was developed by Buysee et al. [20]. It is an index evaluating sleep quality and disorders in the last one month. The index consists of 19 items and 7 units. These units are subjective sleep quality, sleep latency, sleep duration, usual sleep activity, sleep disorders, use of sleeping pills, and daytime functions. The items are scored between 0 and 3. Each of the seven unit headings is first evaluated in its circles, and then the scores of the 7 components are totaled. A total score of 5 or less is considered “good sleep quality” and over 5 “poor sleep quality” [20]. The validity and reliability study of the index was also conducted in Turkey and it was found to be suitable for Turkish society [21]. In addition to this, the sleeping durations of the individuals were also questioned in the questionnaire. Based on the standard classification, the durations were classified as follows: less than 7 hours, “inadequate”; 7-9 hours, “normal”; and over 9 hours, “oversleeping” [22]. The data of the study were evaluated and statistically analyzed using SPSS software. Absolute and percentage, arithmetic mean, and standard deviation values were obtained for each question determined by counting. The following analyses were employed in data analysis: Chi-square test for the estimation of qualitative data; parametric Independent t-test for normal distributions in two independent groups; one-way analysis of variance (ANOVA) for normal distributions in more than two independent groups; and Sperman correlation analysis for intergroup correlation. The findings were evaluated based on 95% confidence interval and p<0.05, p<0.01 significance levels.
Results
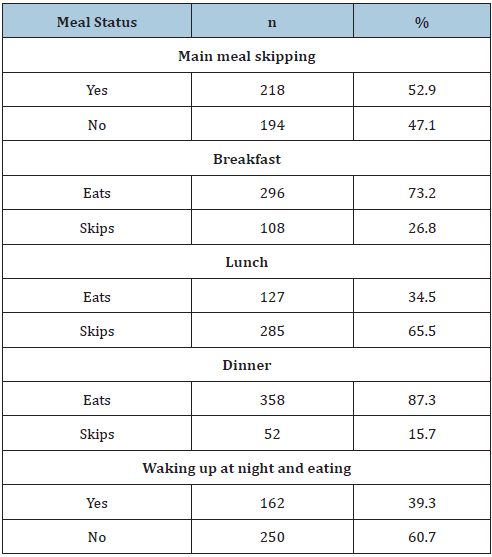
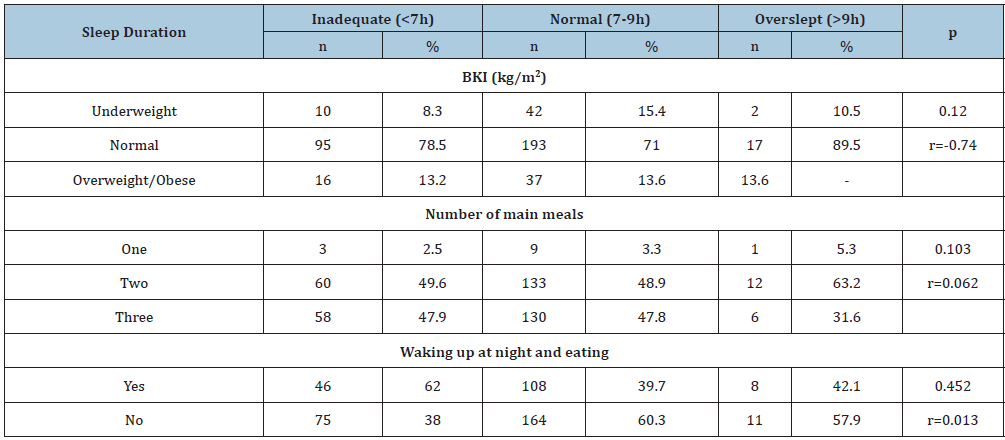
Mean age, height, body weight, and BMI of the individuals participating in the study were 20.7±1.4 years; 163.4±5.8cm, 58.3±10.0kg, and 21.8±3.4kg/m2 respectively (Table 1). 13.1% of the subjects were thin (n=54), 74.0% normal weight (n=305), and 12.9% pre-obese/obese (n=53). Table 2 presents consumption of main meals and eating at night. Accordingly, it was determined that the subjects skipped a main meal (52.9 %), the most frequent skipped meal was lunch (65.5%), and that 39.3% woke up at night and consumed food or drink. While the most frequent reasons for skipping breakfast were getting up late (22.4%) and lack of time (22.4%), the most common reason for skipping lunch (24.6%) and dinner (35.2%) was reluctance to eat. The first three foods preferred by those who woke up at night were fruit (50.8%), chocolatewafer (42.7%), and biscuits-crackers (31.5%), while drinks were tea-coffee (33.8%), ayran-milk (20.7%), and herbal tea (8.3%) respectively. The total PSQI score of the individuals participating in the study was 7.86±2.75. 79.4% of them had “poor sleep quality” and 20.6% had “good sleep quality”. It was determined based on BMI that 15.6% of those having poor sleep quality and only 2.4% of those having good sleep quality were pre-obese/obese. It was found that there was a positively significant correlation between sleep quality and BMI, and between the number of main meals and poor sleep quality (p<0.01, r=0.640; p<0.01; r=0.242 respectively). On the other hand, there was a negatively significant correlation between waking up at night and eating and sleep quality (p<0.01; r=0.118). The mean sleep duration of the participants was 7.0±1.3. Of the women, 29.4% had inadequate sleep (<7 hours), 66% had normal sleep (7-9 hours), and 4.6% overslept (>9 hours). While the rate of those sleeping less than 7 hours in subjects with good sleep quality was 18.8%, this rate was 32.1% in those who had poor sleep quality. There was a significant relationship between PSQI sleep quality and sleep duration (p<0.05). 78.5% of the women with normal BMI slept less than 7 hours, 71% slept 7-9 hours, and 89.5% slept more than 9 hours. As BMI increased, sleep duration decreased. There was a strong negative but insignificant difference between BMI and sleep duration (p>0.05; r:-0.74). The rate of sleeping 9 hours or over in individuals consuming two main meals was higher (63.2%). The number of those with inadequate sleep in subjects stating they ate at night was higher (62.0%). There was no significant relationship between the number of main meals and eating at night, and sleep duration (p>0.05).
Table 1:Mean and standard deviation values of some anthropometric measurements of women.
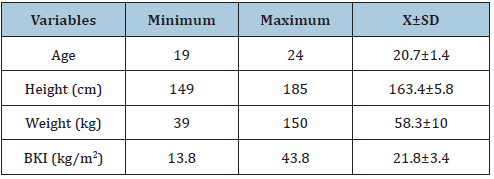
Table 2: Mean and standard deviation values of some anthropometric measurements of women.
Discussion
This study was carried out to investigate the effect of eating
habits on sleep quality in young adult women aged 19-24. Some
studies reported that the relationship between decrease in
sleep duration and high BMI was related to changing peripheral
concentrations of appetite stimulating hormone ghrelin and leptin
hormone suppressing the appetite [23,24]. It was found in another
study that poor sleep quality was related to increase in appetite
and emotional eating behavior [25]. Inadequate sleep, on the other
hand, increased the likelihood of metabolic disorders and obesity
as well as affecting food choice [26]. In the study, mean age, height,
body weight, and BMI were determined to be 20.7±1.4 years;
163.4±5.8cm, 58.3±10kg, and 21.8±3.4kg/m2 respectively. The
mean age, height, body weight, and BMI of university students in a
study by Vassigh [27] were found to be 21.6±2.7 years, 160±6.1 cm,
56.9±8.0 kg, and 20.9±2.6 kg/m² respectively. Erçim & Pekcan [28]
determined height, body weight, and mean BMI of 268 women aged
19-24 as 161.0±5.6cm, 58.1±9.7kg, and 22.4±3.5kg/m2 respectively
[27,28]. The results obtained from these studies are similar to those
of this study.
Pre-obesity and obesity during childhood may lead to the
development of health problems in adolescence and adulthood
(hypertension, type II diabetes, musculoskeletal problems, liver
diseases, cardiovascular diseases, and some types of cancer)
[29,30]. The age-related increase in BMI is important in early
detection of risk factors developing based on obesity in the coming
years and in taking measures [31]. 12.9% of the individuals in this
study were determined to be pre-obese/obese. In other studies
conducted in our country, 16.0% of female students, 12.3%, and
6.0% of female university students were found pre-obese/obese
by Akca et al. [31-33], respectively. In a study conducted on young
female university students in Poland by Suliga et al. [34], the
frequency of pre-obesity/obesity was found 21.8% [34], while
Eittah [35] determined it 28.0% in a study carried out in Egypt. In
general, the prevalence of obesity in recent years necessitates taking
the necessary measures more seriously. It is known that skipping
meals and irregular eating habits is common among university
students, and this can particularly cause obesity. When the eating
habits of young adult women were examined, it was determined
that 52.9% were in the habit of skipping meals, and that the most
frequently skipped meal was lunch (65.5%). Onurlubaş et al. [36]
found in their study investigating university students that 68.5% of
the students skipped meals and that the most frequently skipped
meal was lunch (52.3%) [36]. On the other hand, Yildiz et al. [37]
found that 69.7% of students skipped meals, and that breakfast was
the most skipped meal with 74.1%, The most common reason for
skipping breakfast, the main meal of the day, was waking up late
(22.4%) or lack of time (22.4%), while skipping lunch and dinner
stemmed from “reluctance to eat” (24.6% and 35.2% respectively).
Ozdogan et al. [32] found that 59.6% skipped breakfast due to
getting up late, and that 35.3% skipped lunch because they did not
feel hungry. In another study, lack of time (40.0%) and reluctance to
eat (30.0%) were found to be the reasons for skipping meals among
students [38]. The main reasons why students skipped breakfast
may be due to early lessons or getting up late. Overlapping lunch
and course hours or reluctance to eat due to late breakfast may be
factors in skipping lunch. 39.6% of the students included in this
study stated they woke up at midnight and ate. It was determined
in a study that 25.0% of the students woke up at night and ate, and
that the rate of female students eating at night was 17.1% [39]. One
of the reasons why students wake up at night and eat may be that
they stay up late and study.
Sleep disorders are generally common among university
students. The mean total PSQI score of the women was 7.86±2.75.
In other studies conducted in our country the total PSQI scores were
determined to be 7.89±2.36, 6.9±2.4 and 6.15±1.90 respectively,
and they are in parallel with our finding [40-42]. According to the
results obtained from the same scores, 79.4% of the participants
had “poor sleep quality” and 20.6% “good sleep quality” [43]. The
rates of students having poor sleep quality in other studies carried out in Turkey were reported to be 54.4% and 59.0%.41,43 Studies
conducted in other countries yielded the following results. Cheng et
al. [44] found the rate for poor sleep quality in students 53.0%, and
Lemma et al. [45] found it 57.5%. It is possible to say that the rate
for poor sleep quality in students staying in dormitories was more
than fifty per cent in both other studies and ours. On the other hand,
there are also some studies that found poor sleep quality 26-35%
[46,47]. The reason why poor sleep quality was higher in our study
compared to those of others may have stemmed from inappropriate
physical dormitory conditions, too many students staying in a
room, and different studying hours. Another reason, the effects
of insomnia and irregular eating on obesity and chronic diseases
in these university students are possibly linked to inactivation of
the anti-aging gene Sirtuin 1 (Sirt 1) [48]. Sirt 1 is involved in the
regulation of the sleep-wake cycle, appetite control, obesity and
chronic diseases [49]. The disturbed sleeping patterns, unhealthy
diets and lifestyles may inactivate Sirt 1 with relevance to obesity
and chronic diseases in these university students. Increase in body
weight in university students can frequently occur due to reasons
such as insufficient and unbalanced nutrition, and inability to reach
necessary amount of food. The changes occurring in BMI as a result
of this also affect sleep quality. Cheng et al. [44] determined in their
study conducted on 4318 first year university students that 70.5%
of the students having poor sleep quality had normal BMI, however
that there was no significant relationship between sleep quality and
BMI (p>0.05) [44]. However, 84.4% of the individuals with poor
sleep quality in our study had normal BMI, whereas there found
to be a positively significant correlation between sleep quality and
BMI (p<0.05; r=0.64). Sleep disorders increased significantly as
BMI increased. While a positively significant correlation was found
in our study between main meals and sleep quality score (p<0.05;
r=0.24), a negatively significant correlation was determined
between waking up and eating at night and sleep quality (p<0.05;
r=-0.11) (Table 3). Sleep duration varies by age, and according to
normal sleep classification, people aged between 19 and 24 should
sleep 6-9 hours a day [8]. The average sleep duration in our study
was found 7.04±1.34 hours. 66.0% of the individuals participating
in the study sleep for a sufficient period of time (7-9h). In the study,
78.5% of the individuals sleeping less than 7 hours, 71 % of those
sleeping 7-9 hours, and 89.5% of those sleeping over 9 hours had
normal BMI. There was no negatively significant difference between
BMI and sleep duration (p>0.05; r=-0.74) (Table 4). Aysan et al.
[42] determined in their study that 64.7% of the students slept 6-7
hours, and that sleep quality was poor in students with short (4-5h)
and excess (>9) sleep durations [42]. It was found in another study
that obesity was more frequently observed in women with short
(<7h) and excess (>9h) sleep durations than women with normal
(7-9h) sleep durations, and that there was a significant relationship
between sleep duration and increasing body weight (p<0.05) [50].
Another study conducted on women with normal BMI found that
every one-hour increase in sleep duration in individuals with an
average 7.8h/day sleep increased the obesity risk 26.0% [51]. Nagai
et al. [52] determined that long-term decrease in sleep duration in
individuals with normal body weight increased the prevalence of
obesity by raising the amount of energy intake. Additionally, they
found that extending sleep duration in obese individuals led to 5kg
or more increase in body weight in these individuals [52].
Table 3:Relationship between sleep quality of women and BMI, main meal and night eating situations.
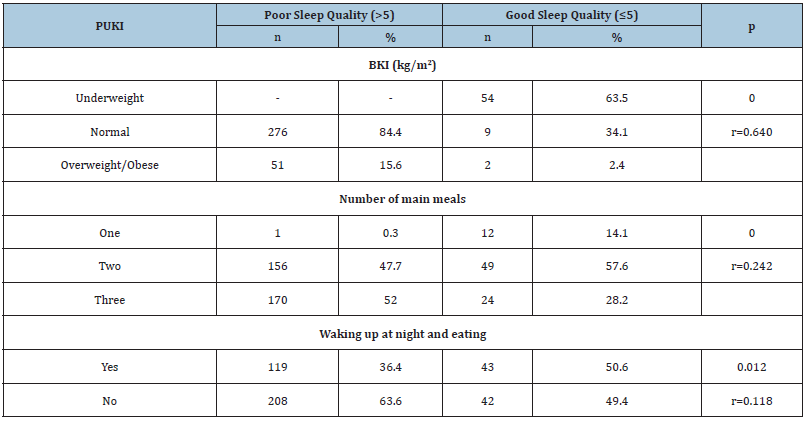
Table 4:Relationship between sleep duration of women and BMI, main meal and night eating situations.
Limitations of the Study
Several limitations of the study should be noted. First, the random selection of participants means that the results are not necessarily generalizable to the entire population. Second, the paucity of data on eating habits in Turkey reduces the possibilities for domestic comparison of our results. In the light of contradictory results from different studies, further research on this topic is indicated. Accordingly, our results should be interpreted within the framework of the study.
Conclusion
The majority of university students have problems with sleep duration and quality. Staying in a dormitory and studying during the night along university life is likely to cause insomnia and irregular eating. Such unfavorable behaviors can result in pre-obesity/ obesity and this, in turn, can increase the prevalence of some chronic diseases in the future. It is recommended that students should be made aware of how to adapt adequate and balanced nutrition matching their daily schedule so that their eating habits can be improved.
Acknowledgement
We would like to thank our students Ayşenur VAR, Çağla DALBAY, and Elif YILMAZ, who spent valuable efforts during data collection process in the study. No financial support from any organization.
References
- Deliens T, Clarys P, Van Hecke L, De Bourdeaudhuij I, Deforche B (2013) Changes in weight and body composition during the first semester at university. A prospective explanatory study. Appetite 65(1): 111-116.
- Fedewa MV, Das BM, Evans EM, Dishman RK (2014) Change in weight and adiposity in college students: A systematic review and meta-analysis. American J Prev Med 47(5): 641-652.
- Ayhan DE, Günaydın E, Gönlüaçık E, Arslan U, Çetinkaya F, et al. (2012) Nutritional habits of Uludağ University Medical Faculty students and the factors affecting them. Journal of Uludağ University Faculty of Medicine 38(2): 97-104.
- Nelson M, Story M, Larson N, Sztainer DN, Lytle LA (2008) Emerging adulthood and college-aged youth: An overlooked age for weight-related behavior change. Obesity 16(10): 2205-2211.
- Laska MN, Pelletier JE, Larson NI, Story M (2012) Interventions for weight gain prevention during the transition to young adulthood: A review of the literature. J Adolesc Health 50(4): 324-333.
- Vella Zarb RA, Elgar FJ (2005) The ’freshman 5’: A meta-analysis of weight gain in the freshman year of college. Journal of American College Health 58(2): 161-166.
- Roger VL, Go AS, Lloyd Jones DM, Benjamin EJ, Berry JD, et al. (2012) Executive summary: heart disease and stroke statistics-2012 update: a report from the American Heart Association. Circulation 125(1): 188-197.
- Peuhkuri K, Sihlova N, Riitta K (2012) Diet promotes sleep duration and quality. Nutrition Research 32(5): 309-319.
- Karagözoğlu Ş, Çabuk S, Tahta Y, Temel F (2007) Some factors influencing the sleep of hospitalized adult patients. Toraks Dergisi 8(4): 234-240.
- Mei Yen C, Edward KW, Yi Jong J (2006) Adequate sleep among adolescents is positively associated with health status and health-related behaviors. BMC Public Health 6: 59.
- Ma Y, Bertone ER, Stanek EJ, Reed GW, Hebert JR, et al. (2003) Association between eating patterns and obesity in a free-living US adult population. Am J Epidemiol 158 (1): 85-92.
- Patel SR, Hu FB (2008) Short sleep duration and weight gain: A systematic review. Obesity (Silver Spring) 16(3): 643-653.
- Spiegel K, Tasali E, Penev P, Van Cauter E (2004) Brief communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Annals of Internal Medicine 141(11): 846-850.
- Grandner MA, Drummond SP (2007) Who are the long sleepers? Towards an understanding of the mortality relationship. Sleep Medicine Reviews 11(5): 341-360.
- Grandner MA, Patel NP, Gehrman PR, Perlis ML, Pack AI (2010) Problems associated with short sleep: bridging the gap between laboratory and epidemiological studies. Sleep Medicine Reviews 14(4): 239-247.
- Cappuccio FP, Taggart FM, Kandala NB, Currie A, Peile E, et al. (2008) Meta-analysis of short sleep duration and obesity in children and adults. Sleep 31(5): 619-626.
- Grander M, Jackson N, Gerstner JR, Knutson KL (2013) Dietary nutrients associated with short and long sleep duration. Data from a nationally representative sample. Appetite 64: 71-80.
- Sato Mito N, Sasaki S, Murakami K, Okubo H, Takahashi Y, et al. (2011) The midpoint of sleep is associated with dietary intake and dietary behavior among young Japanese women. Sleep Med 12(3): 289-294.
- WHO expert consultation (2004) Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 363(9403): 157-163.
- Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Research 28(2): 193-213.
- Ağargün MY, Kara H, Anlar Ö (1996) Validity and reliability of the Pittsburgh sleep quality index. Turkish Journal of Psychiatry 7(2): 107-115.
- Gildner TE, Liebert MA, Kowal P, Chatterji S, Snodgrass JJ (2014) Associations between sleep duration, sleep quality, and cognitive test performance among older adults from six middle income countries: Results from the study on global ageing and adult health (SAGE). J Clin Sleep Med 10(6): 613-621.
- St Onge MP (2013) The role of sleep duration in the regulation of energy balance: effects on energy intake and expenditure. Journal of Clinical Sleep Medicine 9(1): 73-80.
- Kilkus JM, Booth JN, Bromley LE, Darukhanavala AP, Imperial JG, et al. (2012) Sleep and eating behaviour in adults at risk for type 2 diabetes. Obesity (Silver Spring) 20(1): 112-117.
- Beccuti G, Pannain S (2011) Sleep and obesity. Current Opinion in Clinical Nutrition & Metabolic Care 14(4): 402-412.
- Chaput JP, Despres JP, Bouchard C, Tremblay A (2007) Short sleep duration is associated with reduced leptin levels and increased adiposity: Results from the quebec family study. Obesity (Silver Spring) 15(1): 253-261.
- Vassigh G (2012) Evaluation of university students' physical activity status and healthy nutrition index. Master Thesis, Hacettepe University, Department of Nutrition and Dietetics, Ankara, Turkey.
- Erçim RE, Pekcan G (2014) Evaluation of nutrition status of young adults using healthy eating index-2005. Journal of Nutrition and Dietetics 42(2): 91-98
- Falconer CL, Park MH, Croker H, Kessel AS, Saxena S, et al. (2014) Can the relationship between ethnicity and obesity-related behaviours among school-aged children be explained by deprivation? A cross sectional study. BMJ Open 4: e003949.
- Robertson W, Murphy M, Johnson R (2016) Evidence base for the prevention and management of child obesity. Paediatrics and Child Health 26(5): 212-218.
- Akça SÖ, Selen F (2015) The effect of university students meal skipping and daily physical activities on body mass index (BMI). TAF Preventive Medicine Bulletin 14(5): 394-400.
- Özdoğan Y, Özçelik AÖ, Yardım H (2012) Nutritional habits of university students residing in the dormitory. Blacksea-Blacksea-Black Sea 4(15): 139-149.
- Rakıcıoğlu N, Yıldız Akal E (2011) Energy and nutrient intake and food patterns among Turkish university students. Nutrition research and practice 5(2): 117-123.
- Suliga E, Wronka I, Pawlińska Chmara R (2012) Nutritional habits of female university students in relation to self-perception of body. Biomedical Human Kinetics 4: 98-102.
- Eittah HFA (2014) Effect of breakfast skipping on young females menstruation. Health Sci J 8(4): 469-484.
- Onurlubaş E, Doğan HG, Demirkıran S (2015) Nutritional habits of university students. Gaziosmanpaşa University Faculty of Agriculture Journal 32(3): 61-69.
- Yildiz Akal E, Demirduzen SE, Dogan VB, Duman SD, Turkmen ND, et al. (2011) Evaluation of the dietary habits, body images and BMI of Turkish University students who live in dormitory. Pakistan J Med Sci 27(1): 85-89.
- Deepika D, Vinti D (2015) Food preference and dietary intake of college students in Haryana College. Rev Res J 4(8): ROR-1543.
- Likus W, Milka D, Bajor G, Jachacz Lopata M, Dorzak B (2013) Dietary habits and physical activity in students from the Medical University of Silesia in Poland. Roc Panstw Zakl Hig 64(4): 317-324.
- Kuçukgoncu S, Aktar E, Erginbas E, Bestepe EE, Calıkuşu C, et al. (2010) Relationship between dissociative experiences, abnormal sleep experiences, and sleep quality in undergraduate students. Dusunen Adam Journal of Psychiatry and Neurological Sciences 23(2): 77-84.
- Saygılı S, Akıncı AÇ, Arıkan H, Dereli E (2011) Sleep quality and fatigue in university students. Electronic Journal of Vocational Colleges 1(1).
- Aysan E, Karaköse S, Zaybak A, Günay İsmailoğlu E (2014) Sleep quality and affecting factors in university students. Dokuz Eylul University School of Nursing Electronics Journal 7(3): 193-198.
- Altintas H, Sevencan F, Aslan T, Cinel M, Celik E, et al. (2006) Assessment of sleep disorders and sleepiness states of the four students of HÜTF term with epworth sleepiness scale. Sted 15(7): 114-120.
- Cheng SH, Shih CC, Lee IH, Hou YW, Chen KC, et al. (2012) A study on the sleep quality of incoming university students. Psychiatry research 197(3): 270-274.
- Lemma S, Patel SV, Tarekegn YA, Tadesse MG, Berhane Y, et al. (2012) The epidemiology of sleep quality, sleep patterns, consumption of caffeinated beverages, and that use among Ethiopian college students. Sleep disorders 2012: 583510.
- Stein MB, Belik SL, Jacobi F, Sareen J (2008) Impairment associated with sleep problems in the community: relationship to physical and mental health comorbidity. Psychosomatic Medicine 70(8): 913-919.
- Yao KW, Yu S, Cheng SP, Chen IJ (2008) Relationships between personal, depression and social network factors and sleep quality in community-dwelling older adults. Journal of Nursing Research 16(2): 131-139.
- Martins IJ (2016) Anti-aging genes improve appetite regulation and reverse cell senescence and apoptosis in global populations. Advances in Aging Research 5(1): 9-26.
- Martins IJ (2014) Induction of NAFLD with increased risk of obesity and chronic diseases in developed countries. Open Journal Of Endocrine And Metabolic Diseases 4(4): 90-110.
- Theorell Haglöw J, Berglund L, Berne C, Lindberg E (2014) Both habitual short sleepers and long sleepers are at greater risk of obesity: A population-based 10-year follow-up in women. Sleep medicine 15(10): 1204-1211.
- Sun W, Huang Y, Wang Z, Yu Y, Lau A, et al. (2015) Sleep duration associated with body mass index among Chinese adults. Sleep medicine 16(5): 612-616.
- Nagai M, Tomata Y, Watanabe T, Kakizaki M, Tsuji I (2013) Association between sleep duration, weight gain, and obesity for long period. Sleep medicine 14(2): 206-210.
© 2020 Nazlı Nur Aslan Çin. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






