- Submissions

Full Text
Interventions in Obesity & Diabetes
Perspectives of Nursing in the Care of the Patient with Diabetes Mellitus
Belkis Gelvez1, Maribel Osorio2, Freddy Contreras3* and Manuel Velasco4
1Professor Physiopathology EE-UCV, Central University of Venezuela, Venezuela
2Associate Professor of Educational Sciences, Central University of Venezuela, Venezuela
3Associate Professor of Physiopathology, Central University of Venezuela, Venezuela
4Professor of Pharmacology, Central University of Venezuela, Venezuela
*Corresponding author: Freddy Contreras, Associate Professor Physiopathology, Central University of Venezuela, Venezuela
Submission: January 30, 2018; Published: February 23, 2018

ISSN: 2578-0263Volume1 Issue2
Abstract
Individuals suffering diabetes mellitus should participate actively in educational interventions, focused on self-care, that is, caring for and taking care of it-self. These actions ought to include caregivers and family group, and should be given by health professionals trained in therapeutic education in diabetes. Objective: To review the different models of care in people with diabetes. Conclusion: In order to achieve effective and effective selfmanagement in the management of diabetes, it is imperative that all caregivers adopt the chronic care model, (MCC) in order to achieve the goals of metabolic control, adherence and quality of life. MCC appears to be a most effective option for offering high quality comprehensive care, based on evidence.
Keywords: Diabetes mellitus; Health care; Self-care; Self-management; Chronic care models; Education
Introduction
According to the World Health Organization (WHO) [1] in its first world report on diabetes in 2016, the number of people with diabetes and its prevalence is rising worldwide. In 2014 there were 422 million adults (8.5% of population) with diabetes, in comparison to 108 million (4.7%) in 1980; world prevalence normalized by ages has almost duplicated since then, going from 4.7% to 8.5% in adult people. In Venezuela, diabetes mellitus type 2 (DMT2) represents one of the main causes for morbidity and mortality, with serious repercussions on lifestyle, closely associated to nourishment habits, stress handling, and sedentary lifestyle, among other conditioning features [2].
For a person with diabetes mellitus (DM) condition it is necessary to carry out activities with rigor and care due to the high frequency of complications that cause a significant morbidity and mortality rate. Hence, education constitutes an indispensable tool in order to promote activities that he/she must perform individually to keep health and well-being. Daily care has in itself an intrinsic value, for it is essential to survival and has a universal character, related to daily life activities.
Health education is estimated as a requirement by WHO (1998) [3] with a view to develop therapeutic education as a strategy that will allow people with DM and their families access to knowledge, tools and skills that translate into positive and healthy behaviour, as well as alternative practices of satisfactory care for this clinical condition, since evidence shows this kind of help improves psychosocial and sanitary results, especially in the short term [4-6].
Facing an evident increase in the prevalence of non- communicable diseases (NCD) [7] and particularly DM, it's imperative to review the different models of nursing care, in order to promote a praxis approach that will ensure adherence to selfcare or self-handling of this clinical entity.
Methods
A documentary study of transectional and retrospective cut was designed by means of the systematic review of primary articles in scientific journals between 1995 and 2015. Research was carried out in bibliographic databases encompassed electronic journals in health sciences: Medline (Pubmed), Proquest, EBSCO, Virtual Health Library and SciELO, for which the following descriptors were determined: diabetes, nursing care, models of care and therapeutic education in diabetes. The criteria for the inclusion of reviewed articles were: original studies of primary information or previous reviews, contents of scientific importance on the subject, methodological quality and effectiveness and reliability of the information published in spanish or english.
Results
Diabetes Education (DE)
The 2014 WHO's report 7, points out that NCD are long term diseases of generally slow progression, like heart diseases, cancer, respiratory diseases and DM. They are responsible of 63% of deaths every year. That means 38 million people. The risk of death caused by NCD is increased by tobacco smoking, physical inactivity, harmful use of alcohol and unhealthy diets [8].
According to Holman [9], as a result of the increase in human's life expectancy, it is now required to spend more time, resources, and specialized professionals in the care of NCD. NCD care methods are leaving behind the traditional relationship between the care requestor and the health professional, with the former playing a central role in its own care.
Among NCD, DM stands out, as a group of metabolic disorders characterized by chronic hyperglycemia with disturbances in carbohydrate, fats and protein metabolism, attributable to defects in the secretion or action of insulin. There are many pathophysiological processes involved in its appearance spanning from autoimmune destruction of p cells from the pancreas to insulin resistance [10,11].
It is usually hard for patients to deal with many chores of their care: face the symptoms, watching over physic indicators; follow drug regimens; keeping an adequate degree of nutrition, calories intake and exercise and adapting to psychosocial and social expectations. This requires some hard adjustments in lifestyle and calls for setting up efficient interactions with health care givers, modifying both health professional and patient's current vision in order to secure a better quality of life.
One of the reasons that influence unsatisfactory results in the evolution of the disease is the lack of efficient participation by the people with DM in the control of their own condition, which actually means scarce education received from health professionals. Following through a complex regime of life requires a great motivation by the person to adhere both to the different therapeutic modalities (nutritional, exercise, pharmacological, psychological and educational) and to knowledge related to the disease. Even though there is ample evidence that backs this idea, just a minority of people receive adequate therapeutic education [12].
In this sense, success of any therapeutic indication will depend on the patient's degree of understanding, practical skills and motivation to face the requirements of the daily care. This means that every contact with the person with diabetes has then an educational objective, whether it is explicit or implicit, a reason why late 20th century diabetology assumed the clear idea that there is no successful DM treatment without training and education for every individual [13].
An educational program aimed at people with DM, carried out by a multidisciplinary group that work together, fulfill guidelines, objectives and common goals, will accomplish the goal of getting patients to improve their metabolic control, adhere to the established treatment, nourishment changes and physical activity [14]. Additionally, it imposes the need to consider behavioral type factors that may be modified through education as an indispensable part of the treatment [15].
Consensus exists on considering diabetology education as one of the most important supports in the DM treatment [15]. The American Diabetes Association (ADA) and the Latin-American Diabetes Association (ALAD) have manifested that "Education is a right to every person with DM" and must be part of the treatment in every health system, both public and private.
To achieve effectiveness and efficiency in DE' management [16,17] people must be included in a long term therapeutic alliance in which self-management and glycemic control (individualized metabolic control goals) can positively affect life quality and reduce the risk of condition-related complications.
For this it is necessary to carry out the following actions:
1. Theoretical preparation for the person with risk and diagnosis of diabetes mellitus, its family group, caregivers and community members.
2. To administer a structured educational program based on the knowledge referred to DM:
2.1 Requirements for the satisfaction of basic needs according to the health situation.
2.2 Adjust an agenda for self-care compliance with proposals and commitment to change.
2.3 Improve lifestyle and risk factors (promote healthy habits and lay off toxic habits).
2.4 Availability for individual and group support.
3. Improvement of healthy and self-fulfilling alternative behaviors:
3.1 Train and instruct, through educational didactics, on the skills and abilities to be executed as self-care activities (diet, exercise, and capillary glycaemia monitoring and medication adherence: insulin and hypoglycemic agents).
3.2 Controlling and verifying conditions of the skin, feet and oral hygiene.
3.3 Early recognition of signs and symptoms of hypoglycemia and hyperglycemia.
3.4 Periodic return to medical, nutritional, psychological and educational consultation.
4. Periodic evaluation as a strategy to verify the impact of self-management practices on the health of the person by monitoring biochemical indicators (HbAlc, total cholesterol, LDL and HDL cholesterol, triglycerides, microalbuminuria), anthropometric (BMI, waist circumference and percentage of body fat) and non-invasive hemodynamics (systolic and diastolic blood pressure).
Nursing Care in Diabetes Mellitus
Care is an activity all health professionals perform in one way or another when providing their services in different areas for the prevention, diagnosis, treatment and rehabilitation of health. However, nursing is the one that allocates the most effort, time and dedication to care. To Urra [18], care, as an eminently human practice, is influenced by two dimensions: the cultural, where individual and collective practices are found; and the other, morality, where care is assigned a value, an asset that legitimizes acting. It is moral practice to take care of the most precious asset of society, health [19].
Caring is the most primitive and survival act and its nature of being in relation is evident to Barrera [20]. It is the condition from which one is born, grows and learns in relation to his fellow folk, to the environment that surrounds him and to himself. In order to learn to take care of oneself, the educational relationship that is established with others is a fundamental need.
Professional nursing care is structured, formalized and designed to meet the needs of the human being with the purpose of promoting, maintaining or recovering health [15]. To have a theoretical and philosophical foundation conceptual models and theories are necessary, that will outline a mental construction of concrete reality and will guide professional practice.
Therefore, the advantages of the implementation of a conceptual model consistent with the care of the person with DM as indicated by Rodriguez [21] & Benavent [22], include: define the field of nursing action, showing what is essential , establish care in a coherent way, humanize care by individualizing the needs of the person, use of a common language, and finally, evidence the contribution of nursing care in the field of health and the development of guidelines for practice, research, administration and teaching in nursing.
Thus, nursing theories and models developed in recent decades have been a theoretical contribution to care, such as the health promotion model proposed by Pender, which allows understanding human behaviors related to health and, in turn, guide towards the generation of healthy behaviors. The author exposes the primordial elements that influence the modification of the behavior of human beings to promote health [23].
The preponderant role of culture in the education of the sick person was established by Lenninger in his theory by including multiple holistic factors that are universally found in cultures and define the way in which people take care of themselves, including cosmovision, social structure, language and social context, among others that should be considered when educating people, families and communities to assume healthy behaviours [24].
Orem [25] & Kozier [26], give priority to education, pointing out that the central axis of self-care is the knowledge that the person must possess about the disease they suffer, its evolution, pharmacological treatment, as well as the risks and benefits of each action in themselves. For the understanding and compliance of contributions, it is essential that the nurse is acquainted with the person: culture, religion, beliefs, social relationships, and the role they play in the family group and in society, their economic conditions and what is the meaning of the disease and the relationships with its environment.
Figure 1: Theories of Nursing Care [22-24]. Designed and adapted by the authors (2017).
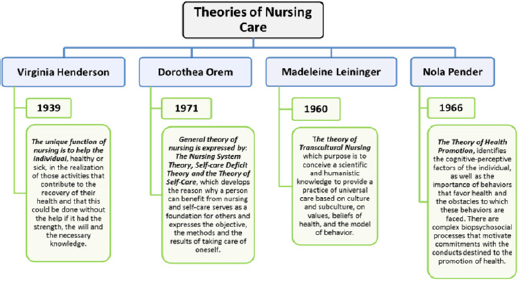
For Henderson, the fundamental guide of nursing is the Nursing Process, through which the needs of the person will be assessed through a theoretical model that guides the objective and subjective data that should be collected and the way to organize them, with a view to establishing whether the person in care presents a situation of dependence in relation to the basic needs established in the model. This will allow orienting actions to overcome the sources of difficulty (psychological, physical, social or educational) to promote the autonomy of the person [21,24].
Care originates and fosters practices, customs or habits that arise from the way in which human beings apprehend and appropriate their reality, which is the source of rites and beliefs [27]. Therefore, besides intervening in the individual dimension, all educational practice should consider the cultural aspect as a possibility to generate favorable changes in health, something that calls for essential social support. It is necessary to highlight the contribution that nursing professionals have had in care, being pioneers in the research and promotion of this practice as a human need, which is the guide of their actions and the means to maintain and/or restore health in people [22-24].
When analyzing some of the nursing theories, it is evident that care of patients with NCDs such as DM can be improved by means of educational action (Figure 1). For the person with DM, educational support is vital because they need help in decision making, acquisition of skills and abilities as well as counsel for the control of positive and encouraging behaviors, incorporating them into their self-care, which guarantees therapeutic adherence [17]. However, recent studies seem to suggest that there is a gap between knowledge, attitude and practice, so that even if theoretical knowledge exists, the attitude of people and health professionals may influence positively of neutralize the carrying out of practice changes that improve the quality of life. The interaction of all those interested in behavioral changes can have a positive long-term influence on the results of the treatment of people with DM [28].
Self-Care
For someone with DM, everything related to care represents a complex situation that must be managed to maintain and preserve health and keep a life free of complications. Thus, it is important to incorporate, as a priority in their daily work, the term caring [18], that etymologically means to put diligence, attention and consideration in the execution of something; to assist, to help, to conserve, be it objects or persons; it is also about seeking one's own health, achieving a good life for oneself, and also, to design a living beware of some risks. In this case, it is understood that you care and take care of yourself. Thus, self-care consists in carrying out actions to provide the minimum requirements that allow the organism to maintain balance (homeostasis).
Under the light of the importance of self-care in diabetes, different instruments or scales have been developed to assess selfcare in diverse populations. One of the most successful has been the Scale Assessment of Self-Care Agency (ASA) [29], product of the first collaborative work, which began in 1983, at the University of Maastricht; this instrument has been validated and applied in Europe and Latin America (Mexico-Colombia) with remarkable success in the self-care of these people.
Self-Management
In a general sense, self-management is defined as the daily attention, carried out by the people themselves, in the course of chronic diseases [9,29,30]. Although it is a term that is often used as a synonym for others, such as self-care, self-management has evolved, no longer being simply the practice of providing information and increasing the knowledge of people [31]. However, these concepts are interrelated; self-management is considered by many authors [30,32,33] as those tasks that healthy people perform at home to prevent illness, instead of just dealing with an existing disease.
The conceptual and theoretical descriptions of selfmanagement in relation to components, processes, and outcomes have expanded and evolved since the 1980s, when Corbin and Strauss [34] identified three sets of activities associated with having a chronic disease, namely: medical care, behavior management and emotional management. Subsequently, nursing scientists described five central processes of self-management that consist on the ability to solve problems, make decisions, use resources, associate with health care providers and act [9].
Within the framework of the theory of individual and family self-management, it was proposed that self-management has three dimensions: context, process and results, with contextual factors that influence the process and results of self-management practices [32]. This theory also expanded the specificity of the processes to include knowledge, beliefs, aptitudes, self-regulation capacities, and social facilitation, and classified the results into proximal and distal [32].
The education program for self-management of diabetes includes the following topics:
a) How and when to control blood glucose;
b) Insulin self-control skills
c) What you need to know about oral medications;
d) Advice on nutrition, which includes carbohydrate counting and heart-healthy eating;
e) Recommendations on exercise, stress management and diabetes;
f) Prevention of long-term complications, foot care and behavior disorders.
Figure 2: Self-management in DM

On the other hand, the health professional committed to the person with DM and its family can select the method or system to guide and educate them, in order to obtain desirable and successful behaviors, as Corbin [34,35] explains (Figure 2).
The programs of self-management of chronic diseases were designed to meet the needs of daily treatment, maintain the activities of daily life, and have been effective in improving behaviors with respect to health status, which has led to fewer hospitalizations in general [31]. These results demonstrated the feasibility of selfmanagement intervention programs that encompass a variety of chronic diseases, which have led to positive health outcomes, many of which persist for years, with the added benefit of reduced health care costs.
Two of the most effective and recognized self-management programs are the self-management program for joint rheumatism and the diabetes self-management program, developed by two pioneers in this field (Holman & Lorig) [9] with the support of the National Institute of research in Nursing and the National Institute of Health [32]. Self-management has evolved from a simple practice of providing information and increasing knowledge to people. All these programs aim to increase the cognitive and practical capacity of people to improve their health status, regardless of the point where they are in the spectrum that goes from health to disease.
Self-management can be seen as the unifying force behind the three levels of prevention-primary, secondary and tertiary prevention-that aim to maintain well-being, control symptoms and the progression of the disease.
Chronic Care Model (CCM)
The Chronic Care Model (CCM) and other similar models emphasize primary health care (PHC) and the recognition of the best clinical outcomes that can be obtained when all components are interconnected and function in a coordinated manner [33]. Likewise, they adopt models that are highly consistent with the approaches of the Pan American Health Organization (PAHO) to strengthen health systems, which are based on PHC and integrated health service networks (IHSDN).
According to the characteristics of the CCM, attention to people with chronic diseases requires moving from a reactive model, centered on the disease, to a proactive and planned model, centered on the person and its context; that guarantees quality of care, facilitates longitudinal follow-up, favors active participation and promotes adherence to treatment and self-control [34,35].
Which characteristics include:
a) Design of the care system,
b) Self-control support for people affected by NCDs,
c) Decision support,
d) Clinical information system,
e) Community and political resources,
f) Health systems.
In this sense Bodenheimer [36], referring to the CCM, emphasizes the action of six elements in this model that allow it to efficiently reach quality care for people with chronic diseases, namely:
a) Promotion of self-help, and self-management, in the participation of the person, family in all their care and monitoring.
b) Support for professional decision making, through the integration of clinical guidelines based on evidence in daily clinical practice and other methods.
c) Improvements to clinical care, focused on team work and extensive professional practice.
d) Electronic information systems for the follow-up, attention and evaluation of the person and to provide relevant data.
e) Changes in the organization (plan including measurable objectives to improve the quality of care)
f) Community participation to mobilize non-health resources.
The bases that sustain the attention of the CCM, to provide quality care focused on innovation consist of [37]:
a) Education for self-management, nutrition, physical activity, quit smoking
b) Counseling to develop self-control skills in people (for example, the management of health, role and emotions related to chronic diseases).
c) Psychosocial care/Ensure self-reward (reinforcement of the individual's behavior with immediate, personal and desirable rewards), medications, vaccines, organize social support.
It is also important in the educational process for the patient to use the 5 A approach during routine clinical encounters [38,39]: ask (knowledge, beliefs and behaviors); advise (provide specific information about the health risk and the potential benefits for the change); agree (establish objectives in collaboration with the person, taking into account their preferences); assist (provide a positive approach to problem solving, identify potential barriers and strategies or resources to overcome them); arrange (design a tracking plan).
The Chronic Care Model has been effective in the selfmanagement of diabetes, based on changes in behavior and lifestyle, the commitment of the person, and the evaluation of the level of preparation for self-care.
For its part, the American Diabetes Association (ADA) recommends in Standards of Medical Care in Diabetes 2016 [40], self-management, education and support:
1. All people with diabetes should be provided with therapeutic education to provide the knowledge, tools and skills necessary for the self-management of diabetes, from the diagnosis and during its evolution.
2. Effective self-management improves clinical outcomes, health status, and quality of life, decreases costs and hospitalizations, allows a healthier adaptation, better adherence to treatment and must be monitored as part of disease control.
3. Diabetological education for self-management should focus on the person, placing them together with their families, at the center of the care model, respecting individuality and ensuring that their values guide the decision-making process.
4. In the first diagnosis, education allows the person to initiate an effective self-management and helps him/her to manage the situation. Continuous support helps maintain it throughout a lifetime, while facing new challenges.
Limitations of Care In DM
Since most chronic diseases are related to lifestyle, selfmanagement represents an opportunity to intervene directly at an individual level; this can achieve favorable effects on health and behaviors with respect to way of living. An approach that emphasizes self-management, adapted to various disorders, population groups and circumstances, could be effective across the spectrum of prevention by establishing healthy guidelines in childhood (primary prevention) and providing strategies to mitigate diseases and address them better in a later stage of life (secondary and tertiary prevention).
The barriers or limitations for self-care are basically related to the human sphere: the human factor, defined generically as "resistance to change". According to this, professionals feel safe and comfortable with what they do, resisting applying a new or unknown methodology that implies a certain degree of initial uncertainty. In addition, lack of empathy and emotional attachment and belonging to the project of the patient and their caregiver, the degree of individual competence in computer environments and/ or the skills necessary to develop safely, the previous opinions on self-care, the workload that involves putting this type of programs in the current environment, the different interests, concerns and priorities of people, caregivers and professionals.
The person with DM has a challenge: to take care of their health and their life, to avoid the progression of acute and chronic complications and to obtain quality of life. Therefore, the unavoidable commitment to itself demands empowering personal care to provide the body with the necessary requirements, and comply with a diet, constant physical activity, and pharmacological treatment, medical and metabolic controls, together with the support of the family or the caregiver in order to preserve and achieve a good quality life in diabetes.
Conclusion
Nursing sciences play an important role in research, application and clinical practice of self-management, and will continue to enlighten the evidence base in favor of innovative and effective practices. As one of the largest and most trusted groups in the field of health professions, nurses are the ones who occupy a unique place to bring self-management to people and the population in general, either to address a chronic illness or to maintain well-being, by acting as a bridge between research and practice. In this way, they bring the practical skills of self-management to communities, not only to survive, but also to thrive with the best possible state of health and well-being.
To achieve effective and efficient self-management in the management of diabetes, it is imperative that all caregivers adopt the CCM model of chronic care, given the synergistic effects demonstrated, where the whole is superior to the sum of its parts. That is, the multidimensional intervention package, which includes several components of the CCM, seems to be more effective, providing a high-quality comprehensive care based on the most advanced evidence, which translates into effective and efficient care for all people and not only for those in chronic conditions.
Therapeutic education is a practice exercised by professionals, people and family supported by the different models of health care aimed at achieving the goals of metabolic control, greater adherence and quality of life.
References
- Informe Mundial sobre la Diabetes (2016) World Health Organization.
- Camejo M, García A, Rodríguez E, Carrizales ME, Chique J (2012) Visión epidemiológica de la diabetes mellitus: situación en Venezuela: registro epidemiológico y propuesta de registro. Rev Venez Endocrinol Metab 10(Suppl 1): 2-6.
- World health Organization Region Office for Europe (1998) Therapeutic patient programmers for healthcare providers in the field of prevention of chronic diseases. Report of a WHO working group. Copenhagen, Denmark, Europe.
- Barlow J, Wright C, Sheasby J, Turner A, Hainsworth J (2002) Selfmanagement approaches for people with chronic conditions: Review. Patient Educ Couns 48(2): 177-187.
- Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM (2002) Selfmanagement education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care 25(7): 1159-1171.
- Davies MJ, Heller S, Skinner TC (2008) Effectiveness of the diabetes education and self management for ongoing and newly diagnosed (DESMOND) programmed for people with newly diagnosed type 2 diabetes: cluster randomized controlled trial. BMJ 336(7642): 491-495.
- OMS (2014) Informe sobre la situación mundial de las enfermedades no transmisibles.
- OMS (2016) Reunión Regional sobre Diabetes- Apura el paso, Gánale a la Diabetes.
- Holman H, Lorig K (2000) Patients as partners in managing chronic disease. Partnership is a prerequisite for effective and efficient health care. BMJ 320(7234): 526-527.
- (2013) Asociación Latinoamericana de Diabetes, guías ALAD sobre el Diagnóstico, Control y Tratamiento de la Diabetes Mellitus Tipo 2 con Medicina Basada en Evidencia, Edición, pp. 39-45.
- American Diabetes Association (2014) Standards of Medical Care in Diabetes- 2014. Diabetes Care 37(Suppl 1): S14-S80.
- Grupo de Trabajo Guías Clínicas y Consensos de la Sociedad Española de Diabetes (2012) Perfil profesional del educador de personas con diabetes. Avances en Diabetologia 28(2): 38-47.
- Contreras F, Hernández C, Hernández P y Díaz L (2015) Diseño e implementación de un Diplomado en Educación Terapéutica en Diabetes (ETD) dirigido a profesionales de la salud en Venezuela. Rev Vitae 64: 1-12.
- Toro MI (2014) El autocuidado y empoderamiento de la enfermedad, ¿hacen la diferencia en la diabetes? Acta Médica Colombiana 39(3): 224227.
- Galindo RM (2015) Educación terapéutica y autocuidado...en España: resultados del estudio observacional transversal Diabetes Attitudes, Wishes and Needs 2 (DAWN2) en España Rev. Endocrinología y Nutrición 62(8): 391-399.
- Mendoza I, Torres J, Herrera A y Colina W (2012) Capitulo XII Educación diabetologica y su proyección a la comunidad. Revista Venezolana de Endocrinología y Metabolismo 10(Suppl 1): 138-142
- Contreras F, Sánchez M, Martínez MS, Chávez M, Mindiola A, et al. (2017) Management and Education in Patients with Diabetes Mellitus. Rev. Medical & Clinical Reviews 3: 2-7.
- Urra E, Jana A, García M (2011) Algunos aspectos esenciales del pensamiento de Jean Watson y su teoría de cuidados transpersonales. Ciencia y Enfermería 17(3): 11-22.
- Feito L (2009) Ética y Enfermería. Madrid: San Pablo.
- Barrera M (2005) Comunicación y antropología. Caracas: Quirón, p. 12.
- Rodríguez JB, Carrión MR, Espina MA, Jiménez JP, Oliver MC, et al. (2005) Marco conceptual, proceso enfermero en EPES. Empresa Pública de Emergencias Sanitarias, Málaga.
- Benavent MA, Francisco C, Ferrer E (2009) Desde el origen de la enfermería hasta la disciplina enfermera. Los modelos de cuidados. En Fundamentos de Enfermería. Colección Enfermería siglo 21. Madrid: DAE;
- Aristizábal G, Blanco B, Sánchez A, Ostiguín R (2011) El modelo de promoción de la salud de Nola Pender: Una reflexión en torno a su comprensión. Enferm Univ 8(4): 16-23.
- Raile M, Marriner Tomey (2011) Modelos y teorías de enfermería. (7th edn), Elsevier. Mosby. Barcelona.
- Orem D (1997) Teoría General de la Enfermería de Orem. En: Teoría y modelos de enfermería de Wesley. McGraw-Hill Interamericana, Mexico, p. 81-86.
- Kozier B, Erb G, Olivieri R (1993) Enfermería fundamental. (4th edn), Tomo I: Editorial Interamericana mcgraw-hill. España. p. 71-72
- Colliere MF (1997) Origen de las prácticas de cuidados, su in-fluencia en la práctica de la enfermería. En: Promover la vida. Madrid: McGraw-Hill Interamericana. (1st edn), Reimpresión, p. 5-17.
- Jacobs S, Serrano Gil M (2010) Engaging and empowering patients to manage their type 2 diabetes, Part II: Initiatives for success. Adv Ther 27(10): 665-680.
- Gast H, Denyes M, Campbell J, Hartweg D, Schott-Baer D, et al. (1989) Self-care agency: Conceptualizations and operationalizations. ANS Adv Nurs Sci 12(1): 26-38.
- Clark NM, Becker MH, Janz NK, Lorig K, Rakowski W, et al. (1991) Selfmanagement of chronic disease by older adults: a review and questions for research. J Aging Health 3(1): 3-27.
- Grady PA, Gough LL (2014) Self-Management: A Comprehensive Approach to Management of Chronic Conditions. Am J Public Health 104(8): e25-e31.
- Ryan P, Sawin KJ (2009) The individual and family self-management theory: background and perspectives on context, process, and outcomes. Nurs Outlook 57(4): 217-225.
- Barlow J, Wright C, Sheasby J, Turner A, Hainsworth J (2002) Selfmanagement approaches for people with chronic conditions: a review. Patient Educ Couns 48(2): 177-187.
- Corbin J, Strauss A (1985) Managing chronic illness at home: three lines of work. Qual Sociol 8(3): 224-247.
- American Association of Diabetes Educators, Covey S, and compliments of Bayer Diabetes Care.
- Bodenheimer T, Wagner EH, Grumbach K (2002) Improving primary care for patients with chronic illness. JAMA 288(14): 1775-1779.
- OPS (2013) Cuidados innovadores para las condiciones crónicas: Organización y prestación de atención de alta calidad a las enfermedades crónicas no transmisibles en las Américas. Washington, USA.
- Whitlock EP, Orleans CT, Pender N, Allan J (2002) Evaluating primary care behavioral counseling interventions: an evidence-based approach. Am J Prev Med 22(4): 267-284.
- Glasgow RE, Davis CL, Funnell MM, Beck A (2003) Implementing practical interventions to support chronic illness self-management. Jt Comm J Qual Saf 29(11): 563-574.
- American Diabetes Association (2016) Standards of Medical Care in Diabetes-Diabetes Care 39(Suppl 1): S14-S80.
© 2018 Freddy Contreras, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






