- Submissions

Full Text
Investigations in Gynecology Research & Womens Health
Would Oral Vinorelbine Replace the Inconvenient Toxic Methotrexate Intramuscular Injection for the Treatment of Ectopic Pregnancies
Kulvinder Kochar Kaur*, Gautam Nand Allahbadia and Mandeep Singh
Scientific Director, India
*Corresponding author:Kulvinder Kochar Kaur, Scientific Director, Dr Kulvinder Kaur Centre for Human Reproduction 721, GTB. Nagar, Jalandhar-144001, Punjab, India
Submission:December 14, 2023;Published: December 21, 2023

ISSN: 2577-2015 Volume4 Issue4
Introduction
An Ectopic Pregnancy (EP) takes place in case of 1% of the pregnancies as well as is a frequent reasons for hospitalization along with treatment in addition to an important etiology with regards to morbidity in patients in gynaecology practice [1]. Patients who present with ruptured ectopic pregnancies as well as are not stable haemodynamically, patients possessing embryonic or cardiac actions along with patients withβ Human Chorionic Gonadotropins (βhCG), greater than 5000-10,000IU/ml are generally treated by surgery, patients who are haemodynamically stable usually receive medical treatment [1].
Methotrexate has assumed a part of being the choiciest drug in case of haemodynamically stable patients in addition to its utilization having been made considerably in variable treatment protocols (single or multiple doses) which possess great success rates as well as is correlated with minimal inimical sequelae .It represents a Folic Acid (FA) antagonist which is responsible for hampering of the enzyme dihydrofolate reductase, that is implicated in the transformation of FA to tetrahydrofolate that is a cofactor with requirement for DNA in addition to RNA production, which results in apoptosis as well as necrosis of trophoblast, leading to EP disturbance [2] Lipscomb et al. [3], in 1999 described this article which till date works in the form of a hallmark regarding EP treatment.
The substantial success rates which have been displayed for methotrexate has been under observation in view of spontaneous resolution of considerable quantities of EP ‘s thereby avoidance of their treatment [4]. Actually, 60% of patients who are haemodynamically stable would illustrate spontaneous resolution by diminishing βhCG quantities without any requirement of any sort of treatment. This thought regarding spontaneous resolution apart from avoidance of treatment in view of treatment being non imperative once there is resolution of pregnancy on its own; however highlights the apparent success rates of methotrexate need to be queried in view of falsely escalating them. Attempting treatment simply in case of viable pregnancies in addition to holding treatment for these ones of spontaneous resolution would significantly result in reduction of what appears to be the great success rates of methotrexate. For instance, a substantially great success rates (92%) were revealed by Lipscomb et al. [3], for EP having βhCG quantities of 2,000-4,999 IU/ml; while <75% had been demonstrated by Cohen et al. [4], in real viable EPs. Inspite of these beliefs on taking into accountjust real viable EPs success ratesof methotrexate have been substantially great (91%) for EP having βhCG quantities of 1,000-1,500IU/ml.
Methotrexate, delivered in the form of intramuscular injection, possesses the capacity of significantly escalating the inimical sequelae for instance nausea, vomiting stomatitis, hepatocellular injury as well as others. Furthermore, there might be reluctance of the infertility specialist or reproductive endocrinologist in the utilization of methotrexate, in breast feeding women, want conception in a short period or are suffering from hepatic/renal disease. These problems warrant looking for newer efficacious agents.
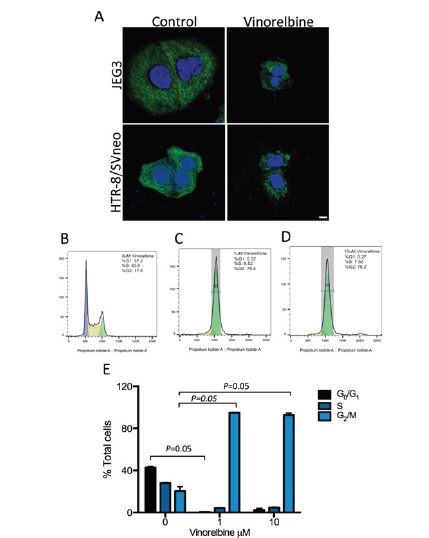
Vinorelbine portrays a semi-synthetic vinca-alkaloid obtained from the Madagascar periwinkle [5]. Initiatially formed in 1979, it is believed to be a well-tolerated chemotherapeutic agent. Vinorelbine stimulates cytotoxicity by binding to tubulin, which disturb mitotic spindle generation as well asleads to arrest of the cell cycle at the metaphase to anaphase transition. This finally results in apoptosis of mitotic cells [6]. Vinorelbine is substantially selective to mitotic instead of axonal microtubules, which possesses preference for it targeting proliferating in addition to considerably proliferative cells [7] (Figure1).
Figure 1:Courtesy ref no -5-Vinorelbine resolves placental mass in xenograft JEG3 model. JEG3 cells were
subcutaneously injected into female SCID mice, and treatment administered intravenously. All mice were treated
(indicated by ↓) three times over two weeks and tumor volume measured every second day. (A-D) Mice treated with
increasing doses of vinorelbine, 1.25mg/kg, 2.5mg/kg, 5mg/kg, or equivalent PBS (n = 8 per group).
(A) Tumor volume (mm3) over time and
(B) tumor volume at time of death is reduced with increasing doses of vinorelbine.
(C) Vinorelbine dose dependently reduced tumor weight and
(D) serum β-hCG levels at time of death. Data are means ±SEM. *p<0.05, **p<0.01, **p<0.001. (e-h) Mice treated
with vinorelbine 2.5mg/kg, methotrexate 2mg/kg, methotrexate 2mg/kg + gefitinib 25mg/kg, or vehicle control (n =
6 per group).
(E) Vinorelbine alone reduced tumor volume over time and
(F) at time of death compared to vehicle control, methotrexate and combination methotrexate and gefitinib.
(G) Tumor weight is reduced by vinorelbine compared to control and methotrexate.
(H) Vinorelbine reduced serum hCG levels below all other treatment groups. Data are means ±SEM.
At present it has received approval for the treatment of nonsmall cell lung cancer, Hodgkin’s lymphoma, breast as well as ovarian cancers [8]. With the acknowledgement that placenta is substantially proliferative at the time of the first trimester however the fallopian tube is not, it is probable plausible vinorelbine might be possessing effectiveness in the context of resolution of ectopic pregnancy whereas minimally impacting the surrounding tube.
Chowdari et al. [9], conducted a phase 1 open label safety as well as tolerability study with regards to vinorelbine which portray an oral chemotherapy agent in the form of an alternate agent for methotrexate, was delivered to patients with EP‘s. Estimation of success rates in addition to inimical sequelae was done. In view of COVID-19 pandemic in Newzealand enrolment was halted/totally stopped with final enrolment of 14 cases. 60mg/m2 of vinorelbine dosage was delivered on days0 as well as, 4. Subsequently assessment of women was performed Clinically (history in addition to General Physical Examination (GPE) o as well as biochemically (full blood count ,urea, electrolytes, Liver Function Tests (LFT) till full resolution of EPs 0,4,7, along with 11 followed by weekly assessment. 50% of patients on this treatment illustrated gastrointestinal upset however none generated neutropenia or LFT aberrations. Mean inclusion (day 0) βhCG quantities were1,117 IU/ ml of which 71.4% patients illustrated successful therapy without any requirement of any kind of surgical management (Figure 2).
Figure 2:Courtesy ref no -9-Individual serum Human Chorionic Gonadotropin (hCG) levels in 14 participants administered vinorelbine at day 0, vs. time in days. Participants requiring surgical management are shown by black lines; patients treated successfully by vinorelbine are shown by bluelines.
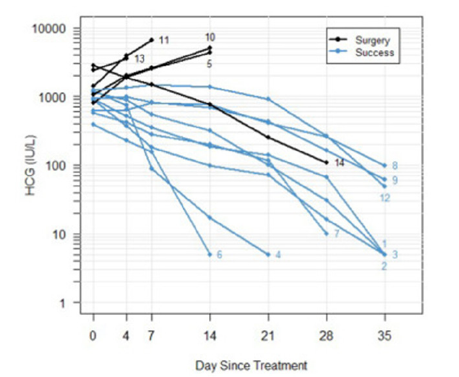
Greater understanding was yielded by thorough examination of every case. Succesful therapy was obtained in 6 patients (patients no-1-4,6 as well as 7) who illustrated rapid reduction in βhCG quantities. Although there was greater temptation of attributing this reduction in βhCG quantities to succesfull vinorelbine therapy it is a pointer of spontaneous resolution of EP. 2ndly viable EPsin general (plateau or escalating βhCG quantities) got successfully treated in case of 3 patients (indicating actual succesfull treatment with vinorelbine. 3) 3rd or failure of treatment was observed in 4 patients (patient number-5,10 ,11as well as 13) where there was requirement of surgical management. 4) 4th patients’ number no14 required to be shifted to the Operating Room in view of rupture in spite of falling βhCG quantities.
Overall if one presumes all were real viable EPs, vinorelbine was successful to a maximal level in 9 (64% success rate) in 14 patients or minimally in just 3 real viable EPs, having a plateauing βhCG quantities patient number-8,9 as well as 12) attaining a 43% success rates. One can presume that the success rates for vinorelbine fluctuated amongst 3%-64% having a mean day 0) βhCG quantities of 1,117 IU/ml .
Ectopic pregnancies substantially influence the patient’s life in addition to her health. There exists a requirement of isolating newer efficacious agents, possessing minimal inimical sequelae. Here Chowdari et al. [9], have aided in provision of an alternative for the methotrexate for the treatment of patients who are haemodynamically stable. The way reasoned previously vinorelbine possessed maximum efficacy in 64% in patients with mean βhCG quantities were1,117IU/ml in contrast to success rates of methotrexate in case of real viable EPs having a plateauing βhCG with akin EP ‘s βhCG quantities having a 90.7% success rates [5].
Greater studies at larger scale need to be performed for evaluating the effectiveness,or instead non inferiority of vinorelbine in contrast to methotrexate. One needs to be cautious to have stringent inclusion criteria where real evolving viable EPs with prior inclusion follow up for detecting reduction, escalating or plateau βhCG quantities in addition to ruling out the ones with spontaneous resolution. These approaches will only aid in decision of the effectiveness of this drug, its superiority along with ease of delivery to finally arrive at conclusions of if vinorelbine is really a magical agent or a plain good one [10].
Conclusion
Previously we reviewed ectopic pregnancies in in the absence of history of Pelvic inflammatory Disease (PID) as well as how Letrozolemight aid in replacingthe toxic methotrexate in cases of early Eps in an endeavour for looking for agents which can replace the inconvenient toxic methotrexate [11,12]. The group of Hastie R had earlierworked on actions of gefitinib,an hampering agent on human placentalcellgrowth in addition tocombined gefitinib as well as methotrexate in case ofnon tubal ectopic pregnancies. Nevertheless, their observation was that vinorelbine possessed 100-1000fold greater robustness in contrast to methotrexate in stimulatingplacental cell demise in vitro, along with possess greater potency in contrast to combination methotrexate in addition to gefitinib (another posited treatment for ectopic pregnancy that isgetting assessed in phase III trials [13,14].
Thus Here Chowdari et al. [9], have aided in provision of an alternative for the methotrexate for the treatment of patients who are haemodynamically stable.The way reasoned previously vinorelbine possessed maximum efficacy in 64% in patients with mean βhCG quantities were1,117 IU/ml in contrast to success rates of methotrexate in case of real viable EPs having a plateauing β hCG with akin EP ‘s βhCG quantities having a 90.7% success rates [5].
Greater studies at larger scale need to be performed for evaluating the effectiveness,or instead non inferiority of vinorelbine in contrast to methotrexate. One needs to be cautious to have stringent inclusion criteria where real evolving viable EPs with prior inclusion follow up for detecting reduction, escalating or plateau βhCG quantities in addition to ruling out the ones with spontaneous resolution. These approaches will only aid in decision of the effectiveness of this drug,its superiority along with ease of delivery to finally arrive at conclusions of if vinorelbine is really a magical agent or a plain good one [10].
References
- Mello NMV, Mol F, Ankum WM, Mol BW, Veen FVD, et al. (2012) Ectopic pregnancy: how the diagnostic and therapeutic management has changed. Fertil Steril 98(5): 1066-1073.
- Gil Y, Zubkov A, Balayla J, Cohen A, Levin I (2023) Apoptosis versus necrosis in tubal ectopic pregnancies following Int J Exp Pathol 104(2): 76-80.
- Lipscomb GH, McCord ML, Stovall TG, Huff G, Portera SG, et al. (1999) Predictors of success of methotrexate treatment in women with tubal ectopic N Engl J Med 341(26): 1974-1978.
- Cohen A, Zakar L, Gil Y, Amer-Alsheik J, Bibi G, et al. (2014) Methotrexate, success rates in progressing ectopic pregnancies: A reappraisal. Am J Obstet Gynaecol 211(2): 128.e1-5.
- Hastie R, Lim E, Sluka P, Campbell L, Horne AW, et al. (2018) Vinorelbine potently induces placental cell death, does not harm fertility and is a potential treatment for ectopic pregnancy. Ebio Medicine 29: 166-76.
- Wang G, Liu XM, Kreis W, Budman DR (1999) The effect of antimicrotubule agents on signal transduction pathways of apoptosis: A Review. Cancer Chemother. Pharmacol 44(5): 355-361.
- Binet S, Fellous A, Lataste H, Krikorian A, Couzinier JP, et al. (1989) In situ analysis of the action of Navelbine on various types of microtubules using immunofluorescence. Semin Oncol 16(2 Suppl 4): 5-8.
- Gregory RK, Smith IE (2000) Vinorelbine--a clinical review. Br J Cancer 82(12): 1907-1913.
- Chowdari P, Hastie R, Lino TU, Middleton A, Capes G, et al. (2023) Oral vinorelbine to treat women with ectopic pregnancy: A phase 1 Clinical safety and tolerability study. Fertil Steril 120(3 Pt 2): 695-696.
- Levin I (2023) Magical bullet or simply nice to have: Safety and tolerability study of oral vinorelbine for ectopic Fertil Steril 120(3 Pt 2): 697-698.
- Kulvinder KK, Allahbadia G, Sing M (2019) Anticipating the occurrence of tubal ectopic pregnancy in the absence of history of pelvic inflammatory disease-a short communication. MOJ Surg 7(2): 23-24.
- Kulvinder K, Allahbadia GN, Singh M (2020) Replacing methotrexate with letrozole in cases of early ectopic pregnancy as an innovative therapy-a short communication. J Gynecol 5(1): 1-3.
- Nilsson UW, Johns TG, Wilmann T, Kaituu LT, Whitehead C, et al. (2013) Effects of gefitinib, an epidermal growth factor receptor inhibitor, on human placental cell growth. Obstet Gynecol 122(4): 737-744.
- Horne AW, Skubisz MM, Tong S, Duncan WC, Neil P, et al. (2014) Combination gefitinib and methotrexate treatment for non-tubal ectopic pregnancies: A case series. Hum Reprod 29(7): 1375-1379.
© 2023 Kulvinder Kochar Kaur. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






