- Submissions

Full Text
Investigations in Gynecology Research & Womens Health
Obstetrical Management of a Pregnancy with Ehlers-Danlos Syndrome: A Rare Case Report
Asma Batool*, Ioannis Tourountous, Naveed Iqbal, Mussarat Sultana, Nida Faisal and Humaira Jamal
Department of Obstetrics and Gynecology, Maternity and Children Hospital, Saudi Arabia
*Corresponding author:Asma Batool, Department of Obstetrics and Gynecology, Maternity, Saudi Arabia
Submission:November 13, 2023;Published: November 24, 2023

ISSN: 2577-2015 Volume4 Issue4
Abstract
EDS (Ehlers-Danlos syndrome) is a group of connective tissue disorders that has a common genotypic defect, but heterogeneous phenotypic presentations. This case report presents a successful pregnancy outcome in a woman diagnosed with an unknown type of Ehlers-Danlos syndrome. The various types of EDS can result in either no complication to severe complications with pregnancy and delivery. Several studies and a review of the literature suggest that, generally in pregnant women with EDS, maternal and neonatal outcomes are favorable. However, in EDS type IV, pregnancy can be associated with serious maternal complications. Therefore, there is a challenging situation for obstetrician and obstetrical management should be individualized. This study discusses the obstetric management of a patient with EDS unknown type and compares it to other studies in the literature.
Keywords:D Ehlers-Danlos syndrome; Pregnancy outcome; Delivery management
Introduction
The Ehlers Danlos Syndrome (EDS) is a clinically and genetically heterogeneous group of Heritable Connective Tissue Disorders (HCTD). It is characterized by joint hyper mobility, skin hyper elasticity and tissue fragility [1-8]. Its classification is based on clinical findings and mode of inheritance [2]. The new classification recognizes 13 subtypes. The definite diagnosis relies for all subtypes except unknown Ehlers Danlos syndrome (uEDS) hyper mobile on molecular confirmation, with identification of a causative variant in the respective gene. This gives information on pattern, recurrence risk and prognosis (Table 1).
Table 1:Clinical classification of Ehlers Danlos syndrome, inheritance pattern and genetic basis.
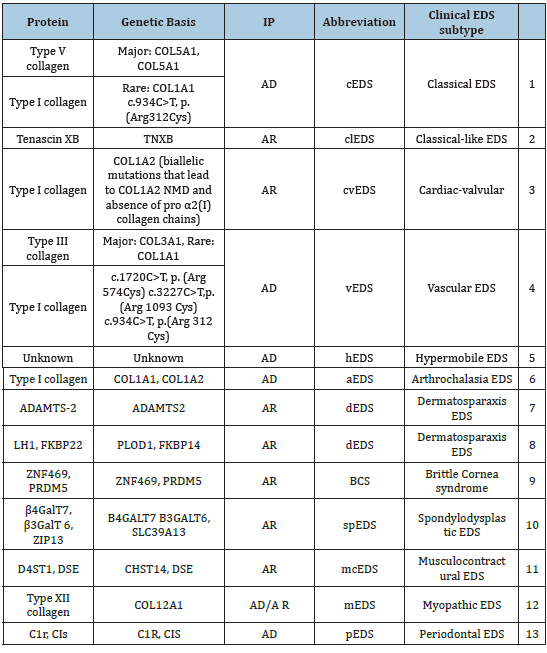
Note: IP: Inheritance Pattern; AD: Autosomal Dominant, AR: Autosomal Recessive, NMD: Nonsense‐Mediated mRNA Decay.
However, the genetic basis of hEDS (Hyper Mobile Ehlers Danlos Syndrome) is still unknown and the diagnosis is based on clinical findings. It is inherited in an autosomal dominant pattern but the causative gene is unidentified. The prevalence was estimated 1:5000 [3] to 1:20000 [4] for all subtypes, but other work suggests a prevalence of 0.75-2% [3]. The incidence of all types of EDS in pregnancy is estimated at 1 in 15,000 [5]. Generally, EDS is considered to remain largely under diagnosed. There is a much greater prevalence of obstetric issues reported by women with Ehlers-Danlos syndrome as compared to general population [6]. Complications related to EDS are frequently seen in obstetric practice. It presents with a range of considerations, which are specific to the classification of type. Some types are associated with severe maternal complications, whereas others are associated with more favorable outcomes [7].
Complications of this syndrome in pregnancy includes, precipitate labour, preterm rupture of membranes, atonic uterus, PPH, vaginal or perineal tears during vaginal birth, wound healing problems like dehiscence and tissue fragility. Stress urinary incontinence can be found in 40-70% 0f women mostly after vaginal delivery. It is associated with weakened pelvic floor, cystocele, bladder distention and pelvic prolapse due to connective tissue abnormalities [4].
Knowledge about this syndrome is important for proper management of this condition. Due to under diagnosis large studies are not available, so presenting this case report to help physicians about the management of this disease. Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Case Report
A patient 36 years old, primigravida admitted in our hospital. She had no antenatal visits and management in our hospital. According to her last menstrual period she was 39 weeks and 2 days on the date of admission. She was diagnosed as EDS since childhood and was followed in a tertiary care hospital in Riyadh. The type of her Ehlers Danlos syndrome was unknown. She also had vitamin D deficiency and received vitamin D supplementation. According to the history she had antenatal care in a private clinic and she had no antenatal complications.
Her parents were healthy and they were first cousins. She had three sisters all with Ehlers Danlos syndrome.
The patient had lax joints, lax skin and scars on her forehead, knees and feet. A picture of keloid and hypertrophic scaring was present (Figure 1). The rest of physical examination was unremarkable. Her vital signs were normal. Her blood investigation was also normal. Her blood group was B positive, Hb-14.4g/dl, liver and renal function tests were normal. The ultrasonography of fetus was normal, longitudinal, cephalic presentation, GA-38weeks, AFI- 10cm, Doppler of UA was also normal (Figure 2).
Figure 1:A picture of keloid and hypertrophic scaring was present.

Figure 2:The rest of physical examination was unremarkable.

Multidisciplinary consultation was asked. Patient refused to be referred to a Fetal medicine center. Due to the potential possible risks of this syndrome and the unknown type of EDS, cesarean section was decided after refusal of the woman for vaginal delivery. Lower segment cesarean section was carried out with general anesthesia with full Preparation of potential intrapartum complications. Abdomen was opened with Pfannenstiel incision, uterus opened at the lower segment. Tissues were markedly fragile and thin and were handled with great delicacy. Baby boy delivered with good APGAR score; birth wt. was 2.7kg. Placenta and membranes were delivered complete. Active management of 3rd stage of delivery was followed. Misoprostol 600microgram was placed per rectal to prevent PPH (post-partum hemorrhage). Uterine incision was closed in two layers by absorbable suture (vicryl no1). Rectus sheath closed with non-absorbable suture proline; mattress stitches applied to the skin. With all these protective measures there was not any intra operative complication. Antibiotics were given for one week to prevent infection.
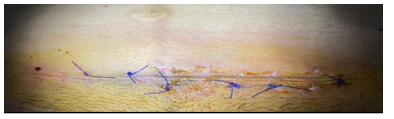
Post operative recovery was normal, uncomplicated and patient was discharged on 3rd post operative day with instructions to come on 7th post op day for evaluation of her condition and healing process of the wound. Figure 3, shows the condition of wound at 7th post operative day. On 7th post operative day wound examined healing was acceptable, alternate stitches were removed, wound was cleaned and advised to come after one week. Antibiotics were given due to the picture of potential mild infection at the upper part of left edge of the wound.
Figure 3:It shows the condition of wound at 7th post operative day.
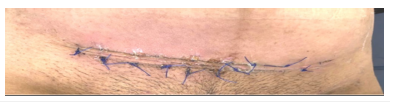
Figure 4, shows the picture of wound after removing the alternate stitches. At the next appointment wound healing was normal, stitches removed. Pt was advised for follow up for reevaluation of her condition after 6 weeks post caesarean section. All the supportive treatment with iron, calcium, LMWH (Low Molecular Weight Heparin) for the post-partum period were given. Patient followed till 6 months postpartum without any problems.
Figure 4:It shows the picture of wound after removing the alternate stitches.
Discussion
Ehlers Danlos syndrome is a rare connective tissue disorder that mainly affects the joints and the skin. It affects the collagen metabolism. Deficiency of the collagen or disordered deposition of collagen takes place. Patients with EDS are high-risk patients and should be followed by a maternal-fetal medicine specialist. Our patient refused to be referred due to some social issues despite of adequate counseling. EDS patients should receive pre-pregnancy counseling [9], planned antenatal care and risk assessment for obstetrical and neonatal complications [10].
The Pre-pregnancy counseling helps to create a management outline of EDS patients to prevent obstetrical complications. In the most common types of EDS, pregnancy is not advised against, but involvement of a geneticist may help the patient to understand the inheritance pattern of their EDS type [11]. In our patient she was diagnosed as Ehlers Danlos Syndrome since childhood but she did not receive any pre-pregnancy or genetic counseling
These patients are at increased risk of having rapid progression of labor and delivery, as well as premature delivery due to cervical insufficiency or premature rupture of membranes. Currently, there are no clear recommendations favoring vaginal versus Cesarean delivery. We have also faced this dilemma that either we should go for vaginal delivery or elective lower segment caesarean section. Decision of elective lower segment caesarean section was made by patient and obstetrician. The risk of pregnancy-related complications is increased in women with vascular Ehlers-Danlos syndrome compared with the general population. Women with vascular Ehlers - Danlos syndrome should be engaged in a shared decision-making process when contemplating pregnancy and pregnancy management [12]. Our patient has unknown Ehlers Danlos Syndrome, we also engaged the patient in a shared decision making for mode of delivery.
Sorokin et al. [13] who presented the largest cases series of obstetrical outcome in hyper mobility type EDS patients, they concluded that this syndrome can result in uneventful pregnancies without an increase in musculoskeletal pain and joint dislocation, leading to successful vaginal deliveries. We also have similar results in our case. The pregnancy was uneventful but contrary to this evidence our patient did not accept vaginal delivery. This may be due to the fact that our patient has unknown EDS and she denied to accept the risk of extended perineal tears.
Another study done by Efrat et al found that there is increased caesarean section rate in pregnant women with EDS [14]. This correlates well with our case. We also carried out lower segment cesarean section in fear of potential risk of perineal tears. Cheulot & Coworkers [15] found that mortality rates are high in patients with vascular Ehlers Danlos Syndrome who became pregnant [15] Castori [16] and coworkers found that delayed wound healing is very common in both abdominal and vaginal deliveries.
They also recommend gentle tissue handling. In our case we also handled the tissues with great delicacy; our patient also had a slightly delayed wound healing. Pelvic organ prolapsed is reported in 15% of women in postpartum period who delivered vaginally [16,17]. Knoepp et al. [18] found that there is no clear advantage of vaginal over caesarian birth or clear evidence to support the routine use of prophylactic interventions. Individual care plans should therefore be formed in partnership with the mother and multidisciplinary teams until further evidence becomes available.
Women with EDS usually have precipitate labour with an increased incidence of perineal tears due to tissue fragility [19]. There is increased risk of traumatic and atonic postpartum hemorrhage due to defective connective tissue and capillary fragility, active management of labour is preferred to prevent postpartum hemorrhage [20]. There is increased resistance to local anesthetic in EDS. The exact mechanism is poorly understood. For caesarean section combined spinal epidural anesthesia is preferred to spinal anesthesia [21]. Our patient refused epidural so general anesthesia was applied with uneventful recovery.
Conclusion
There is no consensus in the literature on the timing and mode of delivery for pregnant women with EDS. Awareness of this condition enables obstetricians to outline the obstetrical management to prevent complications associated with it. The management undertaken in our patient may help obstetricians optimize the perinatal outcome in other women who choose to continue their pregnancy despite the risks of this severe medical condition.
References
- Malfait F, Francomano C, Byers P, Belmont J, Berglund B, et al. (2017) The 2017 international classification of the Ehlers-Danlos syndromes. Am J Med Genet C Semin Med Genet 175(1): 8-26.
- Beighton P, Paepe A, Danks D, Finidori G, Gedde‐Dahl T, et al. (1988) International nosology of heritable disorders of connective tissue, Berlin, 1986. Am J Med Genet 29(3): 581-594.
- Beighton P, Paepe A, Steinmann B, Tsipouras P, Wenstrup RJ (1988) Ehlers-Danlos Syndromes: Revised nosology, Villefranche, 1997. Ehlers-Danlos National Foundation (USA) and Ehlers-Danlos Support Group (UK). Am J Med Genet 77(1): 31-37.
- Volkov N, Nisenblat V, Ohel G, Gonen R (2007) Ehlers-Danlos Syndrome: insights on obstetric aspects. Obstet Gynecol Sur 62(1): 51-57.
- Taylor DJ, Wilcox I Russell JK (1981) Ehlers-Danlos syndrome during pregnancy: A case report and review of the literature. Obstetrical and Gynecological Survey 36(6): 277-281.
- Hurst BS, Lange SS, Kullstam SM, Usadi RS, Matthews ML, et al. (2014) Obstetric and gynecologic challenges in women with Ehlers-Danlos syndrome. Obstet Gynecol 123(3): 506-513.
- Volkov N, Nisenblat V, Ohel G, Gonen R (2007) Ehlers-Danlos syndrome: insights on obstetric aspects, Obstetrical and Gynecological Survey 62(1) 51-57.
- Steinmann B, Royce PM, Superti‐Furga A (1993) The Ehlers-Danlos syndrome. In: Royce PM, B Steinmann (Eds.), Connective tissue and its heritable disorders. (2nd edn), Molecular, Genetic and Medical Aspects, New York, USA, pp. 51-408.
- Palmquist M, Pappas JG, Petrikovsky B, Blakemore K, Roshan D (2009) Successful pregnancy outcome in Ehlers-Danlos syndrome, vascular type. J Matern Fetal Neonatal Med 22(10): 924-927.
- Kang J, Hanif M, Mirza E, Jaleel S (2020) Ehlers-Danlos Syndrome in pregnancy: A review. European Journal of Obstetrics & Gynecology and Reproductive Biology 255: 118-123.
- Pepin M, Schwarze U, Superti-Furga A, Byers PH (2000) Clinical and genetic features of Ehlers-Danlos syndrome type IV, the vascular type. N Engl J Med 342(10): 673-680.
- Murray ML, Pepin M, Peterson S, Byers PH (2014) Pregnancy-related deaths and complications in women with vascular Ehlers-Danlos syndrome. Genet Med 16(12): 874-880.
- Orokin Y, Johnson MP, Rogowski N, Richardson DA, Evans MI (1994) Obstetric and gynecologic dysfunction in the Ehlers-Danlos syndrome. J Reprod Med 39(4): 281-284.
- Efrat S, Laura ND, Nicholas CS, Haim AA (2022) Pregnancy outcomes in women with Ehlers-Danlos Syndrome, The Journal of Maternal-Fetal & Neonatal Medicine 35(9): 1683-1689.
- Cheulot P, Saucedo M, Bouvier-Colle MH, Tharaux CD, Kayem G, et al. (2019) Maternal mortality among women with Marfan syndrome or vascular Ehlers-Danlos syndrome in France, 2001-2012. Gynecol Obstet Fertil Senol 47(1): 30-35.
- Castori M, Morlino S, Dordoni C, Celletti C, Camerota F, et al. (2012) Gynecologic and obstetric implications of the joint hypermobility syndrome (a.k.a. Ehlers-Danlos syndrome hypermobility type) in 82 Italian patients. Am J Med Genet Part Genet A 158A(9): 2176-2182.
- Castori M (2012) Ehlers-Danlos Syndrome, hypermobility type: An under diagnosed hereditary connective tissue disorder with mucocutaneous, articular, and systemic manifestations. ISRN Dermatol 2012: 1-22.
- Knoepp LR, Dermott KC, Munoz A, Blomquist JL, Handa VL (2013) Joint hyper mobility, obstetrical outcomes, and pelvic floor disorders. Int Urogynecol J 24(5): 735-740.
- Georgy MS, Anwar K, Oats SE, Redford DH (1997) Perineal delivery in Ehlers-Danlos syndrome. B Jog: Int J O & G 104(4): 505-506.
- Kaplinsky C, Kenet G, Seligsohn U, Rechavi G (1998) Association between hyperflexibility of the thumb and an unexplained bleeding tendency: is it a rule of thumb? Br J Haematol 101: 260-263.
- Hakim AJ, Grahame R, Norris P, Hopper C (2005) Local anaesthetic failure in joint hypermobility syndrome. J R Soc Med 98(2): 84-85.
© 2023 Asma Batool. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






