- Submissions

Full Text
Investigations in Gynecology Research & Womens Health
Assessment of Fetal Weight Using Johnson’s Formula and Ultra sonographically and its Correlation with Actual Birth Weight
Neha Singh, Brinderjeet Kaur*, Santosh Yadav and Shweta Gupta
Department of Obstetrics and Gynecology, India
*Corresponding author: Brinderjeet Kaur, Department of Obstetrics and Gynecology, India
Submission:August 14, 2020;Published: September 28, 2021

ISSN: 2577-2015 Volume4 Issue3
Abstract
Introduction: The estimation of fetal weight is of paramount importance in the management of labor and delivery. The study was conducted to find usefulness of clinical estimation of fetal weight as it is useful for developing countries where ultrasonography facilities are unavailable in many areas.
Aim: The study aimed at determining accuracy of fetal weight estimation clinically by Johnson’s formula and ultrasonographical by Hadlock’s method.
Material & Methods: A descriptive study in the department of obstetrics and gynecology at a tertiary care hospital in western India was conducted between July 2017-June 2018 on pregnant patients with 37 to 40 weeks gestation after applying inclusion and exclusion criteria.
Results: The study group consists of 260 subjects from urban, rural settings and different socio-economic classes. There was positive correlation between actual birth weight and Johnson’s formula weight (R=0.533, P= 0.000) as well as between actual birth weight and estimated weight by ultrasonography (R= 0.736, P= 0.000). The differences in the estimation of birth weights between the two methods were statistically significant with P value = 0.004. The maximum error in fetal weight measurement was observed with Johnson’s formula (1420gms) as compared to ultrasonography (900gms). The range of percentage error was less than 5% in ultrasound method compared to 31.9% with Johnson’s method therefore ultrasound method has less error compared to Johnson’s method (statistically significant, p value 0.036).
Conclusion: The study highlighted that there was no significant difference between the mean weight obtained through clinical and ultrasound assessments and actual birth weight. Both clinical (Johnson’s formula) and ultrasound methods of foetal weight estimation showed positive correlation with actual birth weight of the foetus after delivery. The clinical method should remain a valuable alternative where ultrasound is unavailable as it also has strong correlation with the actual birth weight.
Keywords: Fetal weight estimation: Johnson’s formula; Hadlock’s method
Introduction
In modern obstetrics accurate estimation of fetal weight is of paramount importance in the management of labor and delivery as it is one of the risk factors which can be anticipated during antenatal period and guides in making decision regarding mode of delivery and in prevention of many intranasal complications, like maternal exhaustion, prolonged labor, atonic and traumatic postpartum hemorrhage. It has been incorporated into the standard routine antepartum evaluation of high-risk pregnancies and deliveries [1,2]. Foetal weight is usually taken as the sole criterion to assess fetal growth. Fetus with a birth weight of less than the 10th percentile of those born at same gestational age or two standard deviations below the population mean, are considered growth restricted. These foetuses fail to achieve its genetic potential and consequently are at risk of increased perinatal morbidity and mortality [3,4] and are more likely to experience poor cognitive development and neurologic impairment during childhood. Delivery of a macrosomia fetus is associated with prolonged labor, intrapartum asphyxia as well as increase maternal risk such as birth canal injuries and post-partum hemorrhage [5-7].
High rate of perinatal mortality is still a major problem for developing countries like India largely attributed to birth weight which remains one of the important parameters that determines neonatal survival [8,9]. Thus, a quick, easy and accurate method for estimating the fetal weight in utero with optimum precision would be of obvious
benefit to the clinical practicing modern obstetrician.
Methods to Measure Fetal Birth Weight
1. Clinical method
a) Tactile assessment of fetal size
b) Johnson’s formula
c) Dare’s formula
d) Dawn’s formula
2. Imaging methods:
A. Ultra-sonographic method
a) Hadlock’s formula
b) Shepherd’s formula
B. Magnetic resonance imaging
Aims and Objectives
The study aimed at determining accuracy of fetal weight estimation clinically by Johnson’s formula and ultrasonographical by Hadlock’s method. This has an important implication for developing countries like India where there is lack of technology but has experienced clinicians. Thus, this study will determine whether clinical method of fetal weight estimation alone can or cannot be helpful in remote areas where ultrasound is not available, to have better maternal and neonatal outcome.
Material and Methods
We conducted a descriptive study in the department of
obstetrics and gynecology at a tertiary care hospital in western
India from July 2017-June 2018 on pregnant patients between 37
to 40 weeks gestation admitted in our hospital.
1) Inclusion criteria:
a) Single fetus with vertex presentation
b) Gestational age between 37 to 40 weeks
c) Those delivered within one week of USG and fundal height
measurement.
d) Consented for study
2) Exclusion criteria
a) Those, who are not sure of her Last Menstrual Period
(LMP) or having irregular periods
b) Those who don’t give consent for study
c) Pregnancy with foetal anomaly
d) Multiple gestation and malpresentations
e) Women with oligohydrominos and polyhydrominos
f) Pregnancy with uterine fibroid or any abdominal mass
The patients were included in the study after applying these
criteria. The Symphysio-fundal height was measured, and fetal
weight was estimated using Johnson’s formula [10]:
Johnson’s formula-Foetal weight (in grams)=(symphysiofundal
height-x) X 155
Where x=13, when presenting part is not engaged
Where x=12, when presenting part at 0 station
Where x=11, when the presenting part is at station+1
For patient more than 91kg, 1cm was subtracted from the
fundal height and for the measurement of the symphysis fundal
height women were asked to empty bladder and lie in supine
position with legs extended. The fundus was defined by placing the
ulnar border of the left hand against the upper border of the uterus.
One end of the non-elastic tape was placed on the upper border
of the pubic symphysis and gently stretched over the midline of
the abdomen and the fundal height was measured in centimeter.
By careful examination the station of the vertex was determined.
Simultaneously fetal weight was estimated ultra-sonographic ally
by Hadlock’s formula.
Hadlock’s Formula
10^ (1.335-(0.0034*AC*FL)+(0.0316*BPD)+(0.0457*AC)+(0.1623*FL)
The formula gave estimated fetal weight in grams when BPD (biparietal diameter), AC (abdominal circumference) and FL (femur length) in centimeters. The liquor volume, absence of any congenital anomaly or multiple gestations, placenta localisation was also ascertained by USG. The patients were followed till delivery. Actual birth weight was noted by weighing machine. Women who did not deliver within 1 week of fetal weight estimation were excluded from the study. All the data were analyzed by using online free statistical calculator. Categorical data was analyzed by Pearson chi2 test. Correlation between two parameters was calculated by Pearson’s correlation. A ‘p’ value of less than 0.05 was considered as the level of significance for all statistical tests.
Results and Observations
A total of 260 patients were included in the study. In the study group, out of 260 subjects 186(71.5%) patients were booked and 74 subjects (28.5%) patients were emergency patients, who were referred from various centers for better management. The majority 162(62.3%) patients belong to urban area while 98 patients (37.7%) were from rural area. Most of the patients were from middle socioeconomic status (60%). As far as age group was concerned majority of subjects were in the age group of 26- 30 years, 131(50.4%) while 88 patients (33.8%) were less than 25 years of age .159(61.2%) were multigravida while 101(38.8%) were primigravida. The frequency of patients was in decreasing order with respect to increasing gravida that is out of 260 subjects 101(38.8%) were primigravida while only 17 subjects (6.6%) were >/= gravida 4. The maternal height distribution showed that 138 patients (53.1%) were between 150-160cm while 87 patients (33.5%) were more than 160cm with only 35 patients (13.5%) less than 150cm. The maternal weight distribution showed 144 (55.4%) were more than 60kgs, 102 (39.2%) were between 51- 60kg and 14(5.4%) were between 40-50kg. 76.9% (200) patients delivered vaginally where as 19.6%(51) patients underwent LSCS for various indication, the difference was not statistically significant (P = 0.635). 121 babies (46.5%) were male while 139 (53.5%) were female. Birth weight wise most of them 46.2% belonged to 2501-3000gm group category. The percentage of low birth weight (<2500gm) was found higher in primi gravida followed by gravida 3 but the finding was statistically insignificant, p value 0.890. In the study the proportion of low birth weight (<2500gm) was found to be higher with maternal weight ranging from 50-60kg (12.3%) compared to women with weight more than 60kg (9.6%), the difference was statistically significant (p value 0.024) (Table 1).
Table 1: Birth weight in relation to maternal weight.
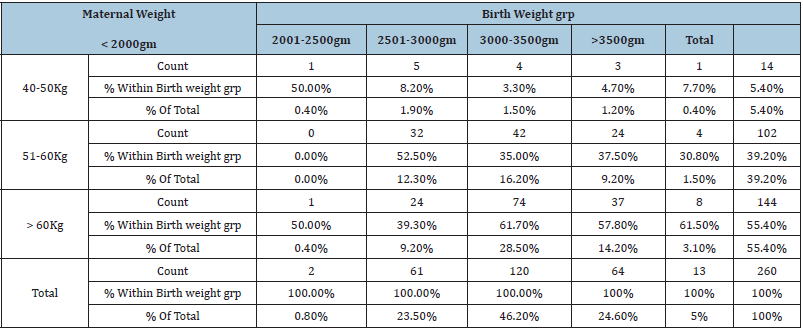
Pearson chi square= 17.609 with degree of freedom 8; P=.024.
There was a positive correlation between actual birth weight and Johnson’s formula weight (R=0.533, P= 0.000) (Figure 1) as well as between actual birth weight and estimated weight by ultrasonography (R=0.736, P= 0.000) (Figure 2). In terms of accuracy the birth weight estimation by ultrasound method was up to 100gms compared to 69 by Johnson’s method and was 200gms by ultrasound compared to Johnson’s method. The accuracy was up to 300gms with ultrasound method compared to Johnson’s method. The differences in the estimation of birth weights between the two methods were statistically significant with P value=0.004 (Table 2). The maximum error in fetal weight measurement was observed with Johnson’s formula (1420gms) as compared to ultrasonography (900gms) (Table 3). The error was least with Johnson method when the birth weight was >3500gms and similarly least error was observed with ultra-sonography when fetal weight was <2000gms. The mean percentage error by Johnson’s method was (11.37) and was higher than ultrasonography (7.67). The mean percentage error by ultrasonography was least in birthweight <2000 grams while maximum in birthweight >3500gm. The Mean percentage error was least in birth weight between 3000-3500gm by Johnson’s method (Table 4) (Statistically significant, p value 0.041). The range of percentage error was less than 5% in ultrasound method compared to 31.9% with Johnson’s method therefore ultrasound method has less error compared to Johnson’s method. (Statistically significant, p value 0.036) (Table 5). Table 6 shows the mean error, standard deviation and Confidence interval of two methods where ultrasonography estimation of birth weight is found to be more accurate as compared to Johnson’s method of birth weight estimation.
Table 2: Correlations of different variables.
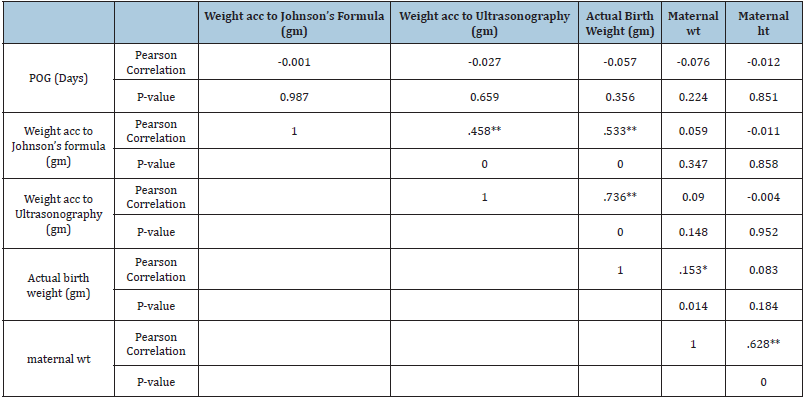
Table 3: Accuracy of birth weight estimated between the clinical and ultrasound methods in terms of grams.
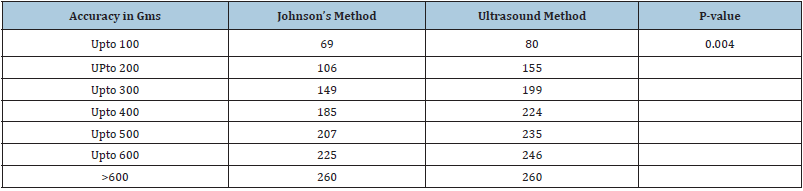
Table 4: Maximum error in various fetal weight group by different method.
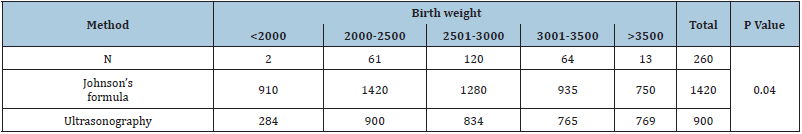
Table 5: Range of percentage error in the various method.
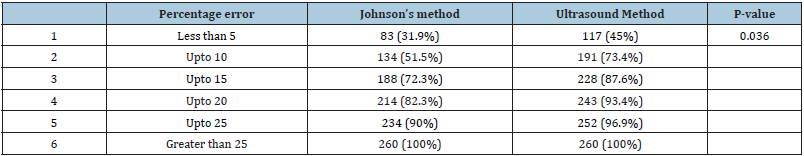
Table 6: Comparison of different method.

Figure 1: Correlation between actual weight & Johnson’s criteria.
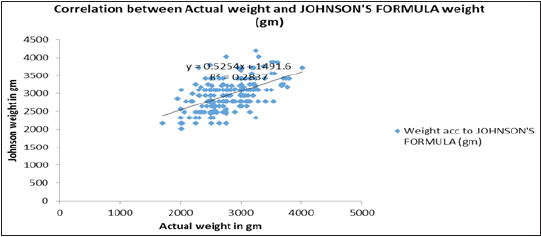
Figure 2: Correlation between actual weight & Ultrasonography weight.

Discussion
Birth weight is an important parameter to predict the neonatal
outcome and its prenatal estimation plays a significant role in
the management of high-risk pregnancies. The estimation of fetal
weight before delivery is of paramount importance considering
the hazards of low birth weight and macrosomia. Both fetal
macrosomia and intrauterine growth restriction increases the risk
of perinatal morbidity and mortality and long term neurologic and
developmental disorders. There are various methods to estimate
the birth weight of foetus at or around the time of delivery like
Johnson’s formula, Dare’s formula and Hadlock’s formula before
delivery.
The present study was undertaken to estimate foetal weight
clinically using Johnson’s formula and ultrasonographic ally and its
correlation with actual birth weight. The study showed a positive
correlation with both Johnson’s formula and ultrasonography (R=
0.533, P= 0.00 and R = 0.736, P = 0.00 respectively) suggesting a
strong positive correlation of actual birth weight with estimated
birth weight by ultrasonography. The findings are well supported
in literature by study by Ugwu et al. [11] who found a strong
positive correlation with both clinical and ultrasound estimated
foetal weight (R= 0.71 P=0.00, and R= 0.69 P=0.00 respectively).
Similarly in their study Annapurna K et al. [12] found that
ultrasonic method of estimation of birth weight was the accuracy
was higher. The maximum error in foetal weight estimation in
current study was found in Johnson’s method (1420gm) compared
to ultrasonography(900gms) and maximum error was least in
birth weight >3500gm by Johnson’s method (750gms) and in birth
weight<2000gms by ultrasonography (284gms). Similarly, Bajaj P
et al. [13] found maximum error in foetal weight estimation to be
most in Johnson’s method (901gms) and least by ultrasonography
(590gms), with maximum error least in birth weight >3000gms by
Johnson’s method and in birth weight <2000gms by ultrasonography
(400gms). Annapurna K et al. [12] also reported that maximum
error in foetal weight estimation was lesser in ultrasound method
(542gms) than clinical method (600gms).
Mean percentage error in current study in foetal weight
estimation was highest by Johnson’s method (11.37%) as compared
to ultrasonography (7.67%). Njoku C et al. [14] and Ugwu EO et al.
[11] in their respective studies found that mean percentage error
in estimation of foetal weight to be higher by clinical method
as compared to ultrasonography. In contrast to present study
Wanjaria DK et al. [15] found mean percentage error in foetal
weight estimation to be equal by ultrasonography and by clinical
method.
In present study range of percentage error was less than 5% in
45% cases by ultrasound as compared to Johnson’s method (31.9%)
and accuracy within 10%of actual birth weight in 73.4% and 51.5%
cases by ultrasonography and Johnson’s method respectively.
Similarly, Njoku C et al. [14] found accuracy within 10% of actual
birth weight in 72% cases by ultrasonography and 69.5% cases
by clinical method. The present study also revealed that there was
no significant difference found between the mean weight obtained
through clinical and ultrasound assessments and actual birth
weight. Both clinical (Johnson’s formula) and ultrasound methods
of foetal weight estimation showed positive correlation with actual birth weight of the foetus after delivery. So, it is clear from this
finding that the clinical assessment of foetal weight is another good
predictor of actual birth weight along with ultrasonic estimation of
foetal weight. This is particularly important in developing country
like ours where Ultrasonography facilities are not available in rural
settings. The clinical method should remain a valuable alternative
where ultrasound is unavailable as it also has strong correlation
with the actual birth weight. The practicing obstetricians may
undertake prospective interventions more confidently than before,
with the aim of minimizing intrapartum and peripartum risks for
both foetuses and mothers.
Conclusion
In a resource limited settings clinical fetal weight estimation should be of paramount importance and essentially be mastered by all health workers as it is capable of giving a bird eye view of the situation where ultra-sonography facility is unavailable. It mandates the policy makers drafting curriculum of health care workers to incorporate this vital assessment tool judiciously.
References
- Sherman DJ, Arieli S, Toybin J, Siegel G, Caspi E, et al. (1998) Comparison of clinical and ultrasound estimation of fetal weight. Obstet Gynecol 91(2): 212-217.
- Chauhan SP, Hendrix NW, Magann EF, Morrison JC, Kenney SP, et al. (1998) Limitations of clinical and sonographic estimates of birth weight: Experience with 1034 parturients. Obstet Gynecol 91(1): 72-77.
- Lubchenco LO, Hansman C, Dressler M, Boyd E (1963) Intrauterine growth as estimated from live born birth-weight data at 24-42 weeks of gestation. Pediatrics 32: 793-800.
- Bernstein IM, Horbar JD, Badger GJ, Ohlsson A, Golan A (2000) Morbidity and mortality among very-low-birth-weight neonates with intrauterine growth restriction. The Vermont Oxford Network. Am J Obstet Gynecol 182(1 Pt 1): 198-206.
- Boulet SL, Alexander GR, Salihu HM, Pass M (2003) Macrosomic births in the United States: determinants, outcomes, and proposed grades of risk. Am JObstet Gynecol 188(5): 1372-1378.
- Ugwa EA, Gaya S, Ashimi A (2015) Estimation of fetal weight before delivery in low-resource setting of North-west Nigeria: can we rely on our clinical skills? J Matern Fetal Neonatal Med 28(8): 949-953.
- Husslein H, Worda C, Leipold H, Szalay S (2012) Accuracy of fetal weight estimation in women with diet controlled gestational diabetes. Geburtshilfe Frauenheilkd 72(2): 144-148.
- Raman S, Urquhart R, Yusof M (1992) Clinical versus ultrasound estimation of fetal weight. Aust N Z J Obstet Gynaecol 32(3): 196-199.
- Watson WJ, Soisson AP, Harlass FE (1988) Estimated weight of the term fetus. Accuracy of ultrasound vs. clinical examination. J Reprod Med 33(4): 369-371.
- Shittu AS, Kuti O, Orji EO, Makinde NO, Ogunniy SO, et al. (2007) Clinical versus sonographic estimation of foetal weight in Southwest Nigeria. J Health Popul Nutr 25(1): 14-23.
- Ugwu EO, Udealor PC, Dim CC, Obi SN, Ozumba BC, et al. (2014) Accuracy of clinical and ultrasound estimation of fetal weight in predicting actual birth weight in Enugu, Southeastern Nigeria. Niger J Clin Pract 17(3): 270-275.
- Annapurna K, Rama C, Ramamani C (2015) A Comparative study of fetal weight estimation at term by clinical method and ultrasound method and after delivery. Ind J Applied Res 5(6): 2249-555X.
- Bajaj P, Kadikar GK, Kannani M, Bhatt M, Shah S (2017) Estimation of foetal birth weight clinically and sonographically and its correlation with its actual birth weight: a prospective and comparative study. Int J Reprod Contracept Obstet Gynecol 6: 3103-3108.
- Njoku C, Emechebe C, Odusolu P, Abeshi S, Chukwu C, et al. (2014) Determination of accuracy of fetal weight using ultrasound and clinical fetal weight estimations in Calabar south, south Nigeria. International Scholarly Research Notices 2014: 970973.
- Wanjaria DK, Kamau K (2017) Accuracy of ultrasound versus clinical fetal weight estimation at term with actual birth weight in Kenyatta national hospital. Europe J Health Sci 1: 22-42.
© 2021 Brinderjeet Kaur. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






