- Submissions

Full Text
Investigations in Gynecology Research & Womens Health
Integrating CERVICO-Vaginal Smear into the Overall Management of Women Living with Human Immunodeficiency Virus (HIV) at the Day Hospital of the Infectious Diseases Department at the University Hospital Mohammed VI in Marrakesh
HE Hassan1, F Etoughe1, YB Komba1, M Rateib1, Z Talibi1, F Ihbibane1, L Boukhani2, H Rais3 and N Tassi1
1Department of infectious diseases University Hospital Mohammed VI, Marrakesh, Morocco
2Department of gynecology University Hospital Mohammed VI, Marrakesh, Morocco
3Department of pathology University Hospital Mohammed VI, Marrakesh, Morocco
*Corresponding author: Hassan HE, Department of infectious diseases University Hospital Mohammed VI, Marrakesh, Morocco
Submission: February 04, 2021;Published: February 26, 2021

ISSN: 2577-2015 Volume4 Issue1
Abstract
Objective:
integrated the implementation of the cervico-vaginal smear into the activity of the infectious diseases department.Materials and Methods: This is a prospective study conducted within the department of infectious diseases since January 2019. The cervico-vaginal smear was proposed and carried out in women living with HIV and followed at the day hospital.
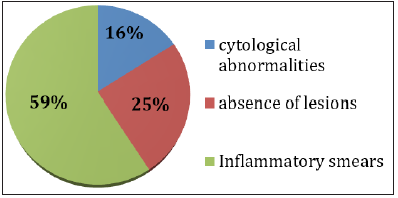
Results: Fifty-five patients were collected. The average age was 37 years [19-65 years]. Smoking was found in 8 patients. The average age of first sexual intercourse was 20 years with extremes ranging from 16 to 32 years. At the time of the smear, the average CD4 was 729 /mm2. A total of 14 (25.4%) patients had a CD4 < 500. Of the 55 smears performed, the result was as follows: in 4 patients the smear was poorly preserved ,7 patients pauci-cellularity. For the rest the cervico-vaginal-smear was normal in 11 patients (25%), inflammatory in 26 patients (59%), seven (16%) patients had cytological abnormalities of Atypical squamous cells of unknown significance (ASCUS). Colposcopy was performed in 2 patients with TAG I, one of whom had a biopsy. At the biopsy there was polyploid ectropion altered by a severe chronic inflammatory lesion, without signs of specificity or malignancy.
Conclusion: This work has allowed us to integrate and facilitate the adhesion of women living with HIVto the cervico-vaginal smear, as well as a close collaboration between infectiologist and gynecologist for better management.
Keywords: Pap smear; Cervical cancer; HIV
Introduction
Cervical cancer is the fourth leading cause of cancer and cancer death among women worldwide [1]. According to the International Agency for Research on Cancer (IARC) in 2018, the global incidence is estimated at 570,000 new cases per year, of which more than 80% occur in developing countries [1]. In Morocco, the cervical cancer represents a major public health problem. It ranks second, after breast cancer in Moroccan women [2]. The incidence of cervical cancer remains high among women living with HIV. However, many studies have shown that this population has an increased risk of developing intraepithelial cervical neoplasia [3]. In the fight against cervical cancer, Morocco has a national cancer control programme under the aegis of the LALLA SALMA Foundation since 2006, thus enabling the creation of reference centers for screening and diagnosis of cervical cancer [4]. Women living with HIV often escape this program because of fear of stigmatization and disclosure of their HIV status. It is in this perspective that we have integrated the implementation of the cervico-vaginal smear (Pap smear) into the activity of the infectious diseases department for early detection in order to make recommendations regarding management.
Materials and Methods
This is a prospective study conducted within the department
of infectious diseases since January 2019. The Pap smear was
proposed and carried out for women living with HIV and followed
at the day hospital of the department of infectious diseases of Arrazi
hospital. A total of 55 Pap smear were completed after the patients
consent. The infect ologists benefited from a training provided
by the Obstetrics and gynecology Department of the University
Hospital Mohammed VI concerning the realization of Pap smears.
The samples were taken in a room dedicated within the department
of infectious diseases and equipped with a gynecological table with
the necessary materials such as disposable speculums, swabs, clean
gloves, surgical masks and a lamp post.
The Pap smear was offered to all HIV positive women who
have been followed for at least one year and who have attended
the day hospital. Once accepted before implementation, all
contraindications were ruled out including menstruation, genital
infectious, sexual intercourse least than 48 hours.
For all patients, the following information were collected:
epidemiological data, risk factors, age of first sexual intercourse,
parity, unprotected sex, occupation, smoking), the anti-retroviral
treatment received, and the results of the immuno-virological
assessment. Once the samples were collected, they were sent to the
histo-pathology department of the Arrazi Hospital. The Pap smear
was conducted in accordance with a number of recommendations,
from ANAES 2002 [5]. The cytological diagnosis was based on the
Bethesda classification [6].
Result
During this period, 70 patients were offered Pap smear among
which 55(78.5%) agreed and 15 patients refused (21.4%). None
of our patients had a subsequent Pap smear. The average age was
37years with extremes ranging from 19 to 65years. The average age
of first sexual intercourse was 20 years with extremes ranging from
16 to 32 years. The socio-professional categories are as follows:
10 housewives (18%), 6 waitresses (11%), 8 sex workers (15.5%)
and one civil servant. According to marital status 26 were married
(47.2%), 13 divorced (26.6%), 10 single (18%) and 6 widows
(11%).
The risk factors for the cervical cancer were: multiparity, use of
oral contraceptives, and smoking was found in 8 patients (14.5%).
At the time of the smear, the average CD4 was 729/mm3. A total
of 14(25.4%) patients had a CD4 < 500/mm3. Regarding the antiretroviral
treatment all our patients were on treatment. Of the 55
smears performed, the result was as follows: for 4 patients the
smear was poorly preserved, 7 patients pauci-cellularity. For the
rest of the patients the distribution is shown in Figure 1. Seven
(16%) patients had cytological abnormalities of Atypical squamous
cells of unknown significance (ASCUS). Colposcopy was performed
in 2 patients with atypical transformation grade 1, one patient had biopsy, who reveled polyploid ectropion altered by a severe chronic
inflammatory lesion, without signs of specificity or malignancy.
Figure 1: Distribution of women according to Cervico-vaginal smear results.
Discussion
Women living with HIV have an increased risk of developing
intraepithelial cervical neoplasia. Screening represents a major
therapeutic axis and must be systematic in HIV positive patients
to prevent progression to dysplastic lesions. Cervical cancer is one
of the easiest forms of cancer to prevent and cure, for a reason
vaccination to HPV, early screening and treatment. In a cohort in
Morocco, the prevalence of HPV among women living with HIV
was 39.3% [7] and HPV vaccines were introduced in 2008 and
recommended for girls before the beginning of sexual activity [4].
However, the cost of available HPV vaccines remains high and is not
affordable for the majority of the population. Early detection by
Pap smear has proven its effectiveness. For women living with HIV,
cervical-uterine cytology testing for cervical cancer is recommended
when HIV is discovered. The frequency of monitoring according to
Morlat reports is as follows: In the absence of a prior intra-epithelial
squamous lesion, cytology will be monitored annually for 3 years.
After three normal consecutive cytologies, subject to a
controlled HIV load and a CD4 level of > 500/mm 3, cytology is
performed every 3 years at the same rate as the general population.
In other situations, cytology should be monitored annually [8].
In Morocco, this population often escapes the screening program
because for the fear of discrimination and disclosure of their HIV
status. With this in mind, we conducted a national pilot study on the
integration of the Pap smear into the overall management practice
of patients followed in our day hospital. During this experiment
the Pap smear was proposed in 70 patients, we recorded 16% of
refusals due largely to lack of awareness of cervical cancer and
screening methods, lack of symptoms, lack of awareness of cervical
cancer risk factors and fear of testing [9,10]. This work allowed us
to join women living with HIVin the cervico-vaginal smear as none
of our patients had a subsequent Pap smear. Of the 55 cervicovaginal
smears in our study, 7 had cytological abnormalities and
were referred to the gynecology department for colposcopy. One of
the major difficulties encountered during the study was the refusal
of some patients to perform the exam, nevertheless we hope and aim to convince more and more of them over time. Knowledge of
risk factors and the target population is essential for prevention.
Several risk factors have been identified in the literature: persistent
HPV infection, the multiplicity of sexual partners, smoking, the use
of oral contraceptives, lack of hygiene, immunodeficiency [2,11-13].
Conclusion
This work has allowed us to integrate and facilitate the
adhesion of women living with HIV to the Pap smear, as well as a
close collaboration between infectiologist and gynecologist for a
better management.
However more actions are needed:
1. National HIV awareness
2. HPV typing
3. Promoting HPV vaccination.
References
- Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, et al. (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6): 394-424.
- CO/IARC (2019) Human papillomavirus and related diseases report in Morocco. Information center on HPV and Cervical Cancer (HPV Information Centre).
- Seck AC, Faye MA, Critchlow CW, Mbaye AD (1994) Cervical intraepithelial neoplasia and human papillomavirus infection among Senegalese women seropositive for HIV-1 or HIV-2 or seronegative for HIV. Int J STD Sida 5(3): 189-193.
- Belglaiaa E, Mougin C (2019) Cervical cancer: Current situation and management in Morocco. Bulletin du Cancer 106(11): 1008-1022.
- ANAES (2002) Recommandation pour la pratique clinique. Conduite à tenir devant une patiente ayant un frottis cervico-utérin anormal. Actualisation.
- Solomon D, Davey D, Kurman R, Moriarty A, Connor DO, et al. (2002) The 2001 bethesda system: terminology for reporting results of cervical cytology. JAMA 287(16): 2114-2119.
- Belglaiaa E, Elannaz H, Mouaouya B, Aksim M, Mercier M, et al. (2015) Human papillomavirus genotypes among women with or without HIV infection: an epidemiological study of Moroccan women from the Souss area. Infect Agent Cancer 10: 44.
- Blanc A, Bonnet F, Vezinet F, Costagliola D, Dabis F, et al. (2017) Groupe d'experts pour la prise en charge du VIH. P. 26.
- Phan AB, Moreau A, Colin C, Poitrine FC, Schott P, et al. (2012) Obstacles au dépistage du cancer du col de l'utérus rencontrés par les médecins généralistes chez les femmes âgées de 50 à 65 ans. Prat Org Soins 43: 261-268.
- Nani S, Benallal M, Hassoune S, Kissi D, Maaroufi A (2013) Involvement of general practitioners in the province Benimellal (Morocco) in screening for cervical cancer. Pan Afr Med J 14: 152.
- WHO/IARC (2012) Biological agents. Volume 100 B. A review of human carcinogens. IARC Monogr Eval Carcinog Risks Hum 100(Pt B): 1-441.
- Chaouki N, Bosch FX, Muñoz N, Meijer CJ, El Gueddari B, et al. (1998) The viral origin of cervical cancer in Rabat, Morocco. Int J Cancer 75(4): 546-554.
- Gnaoui N, Benchakroun N, Benider A, Hassar M, Saile R, et al. (2009) Typing of human papillomavirus and evaluation of risk factors associated with cervical cancer in Morocco. Eur J Sci Res 31: 229-236.
© 2021 Hassan HE. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






