- Submissions

Full Text
Investigations in Gynecology Research & Womens Health
Pseudoaneurysm of the Uterine Artery After Abdominal Bilateral Salpingo-Oophorectomy Caused by Tubo-Ovarian Abscess: A Literature Review
Shin YK, Jeong S, Kim JH and Hye JD*
Department of Obstetrics and Gynecology, Korea
*Corresponding author: Hye JD, Department of Obstetrics and Gynecology, Korea
Submission: October 23, 2019;Published: November 07, 2019

ISSN: 2577-2015 Volume3 Issue2
Abstract
Uterine artery pseudoaneurysms (UAPs) are rare vascular lesions and may be life threatening if not diagnosed and properly treated. Tubo-ovarian abscess (TOA) represents an end stage process of pelvic inflammatory disease and the definitive therapy is surgery. We describe the case of a woman with a UAP after abdominal bilateral sapling-oophorectomy caused by a TOA. Six days later, she presented with sharp abdominal pain, and a Jackson-Pratt drain was filled with 70cc per hour. Selective uterine artery angiography demonstrated a UAP, and embolization was performed successfully. And we reviewed 10 cases of pseudoaneurysm after a gynecological operation, especially the first symptoms and diagnosis methods. In conclusion, UAP suspicion is required in the event of first symptoms such as vaginal spotting, abdominal discomfort/pain, fever, dizziness, etc. And, if it is suspected even slightly, an imaging works up should be conducted in a timely manner to quickly achieve diagnosis and treatment.
Keywords: Uterine artery pseudoaneurysm; Tubo-ovarian abscess; Literature review; CT angiography; Uterine artery embolization
Introduction
A pseudoaneurysm is the result of an incomplete laceration of the arterial wall that enables blood flow to perivascular tissues. In a pseudoaneurysm, there is persistent blood flow that allows communication between the lesion and the parent vessel [1]. Trauma, surgery, or infection can cause vascular injury and enable blood to enter the periarterial tissue, resulting in the development of a pseudoaneurysm [2]. Uterine artery pseudoaneurysms (UAPs) is a rare but serious complication of pelvic surgery that may go unnoticed in the early postoperative period [3]. A tubo-ovarian abscess (TOA) represents an end-stage process of pelvic inflammatory disease (PID) and consists of an encapsulated or confined ‘pocket of pus’ with defined boundaries that form during the infection of a fallopian tube and ovary and cause severe adhesion in the pelvic cavity. Conservative medical therapy with intravenous broadspectrum antibiotics is considered the first-line therapy. However, if the abscess ruptures, it can be a life-threatening surgical emergency and lead to the development of sepsis. Therefore, if fertility is not desired, bilateral sapling-oophorectomy and hysterectomy will provide definitive therapy [4]. In this report, we present a case of uterine artery pseudoaneurysm after abdominal bilateral sapling-oophorectomy in a 50-year-old woman. A PubMed search of the English-language medical literature using the keywords “pseudoaneurysm”,” uterine artery” and” embolization” yielded some cases of pseudoaneurysm after a gynecological operation. In addition, through a review of these cases, the characteristics are identified and will be helpful in similar conditions in the future.
Case Report
A 50-year-old postmenopausal woman, gravida 3, para 0, abortion 3, came to the emergency department because of abdominal pain and fever that occurred two days prior. Transvaginal ultrasound (TVUS) showed an ill-defined, multiseptated bilateral ovarian mass (right: 4.7*4.5cm, Lt: 3.6*3.9cm) in her pelvis. Abdominal-pelvic computed tomography (CT) also showed a multiloculated cystic mass in the bilateral ovary, r/o bilateral TOA. (Figure 1) She was given intravenous antibiotics for 14 days. Follow-up transvaginal ultrasound showed that bilateral ovarian mass had decreased in size but not completely resolved; then, it was decided to perform an operation. Open bilateral sapling-oophorectomy, appendectomy, partial omentectomy, adhesiolysis and bowel serosa 1’ repair was performed, and a Jackson-Pratt (JP) drain was placed in the posterior cul-de sac. Hysterectomy was considered but not performed as it was difficult to remove the posterior uterus, intestine and posterior cul-de sac due to severe adhesion. The operating time was 120 minutes, and the total blood loss was 100mL. The immediate postoperative period was uncomplicated.
Figure 1: Initial CT showing bilateral TOA.

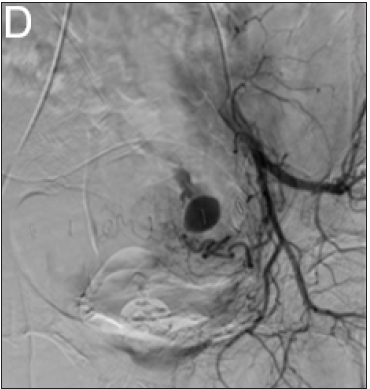
Two days after surgery, the patient presented a tympanic temperature of 38.6 °C but no symptoms other than chills. Then, the fever gradually subsided. At 7 days after surgery, the patient presented a tympanic temperature of 38.0 °C and no improvement in the pain in the lower abdominal and suprapubic area. Abdominalpelvic CT showed less than 5cm of localized air and fluid collection in the pelvic cavity and anterior abdominal wall (Figure 2). After walking back from the CT room, the patient suddenly complained of severe, sharp abdominal pain, and the volume in the JP drain was 70cc for an hour. TVUS did not produce any findings other minimal fluid collection in the cul-de sac. Once again, abdominal CT angiography was performed and revealed a pseudoaneurysm in the left pelvic cavity 1.5 cm in size with related bleeding but no rupture (Figure 3) and (Figure 4). Therefore, pelvic angiography (Figure 3) was performed for definitive diagnosis and treatment. It showed pseudoaneurysm formation at the side wall of the left uterine artery. Embolization was performed and occlusion of the artery was completed. A contralateral angiogram showed no communication with the lesion. Eight days after embolization, the JP drain was removed after, as there had been no fluid in the JP drain for three days, and the patient was discharged. At the 2-week follow-up, the patient was in good health.
Figure 2: Post-op CT before sharp abdominal pain showing post-op change.
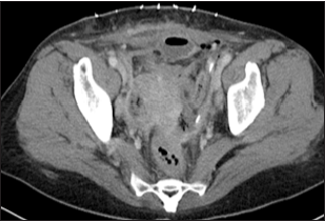
Figure 3: Pre-UAE CT showing a pseudoaneurysm (arrow) close to the left aspect of the uterus.
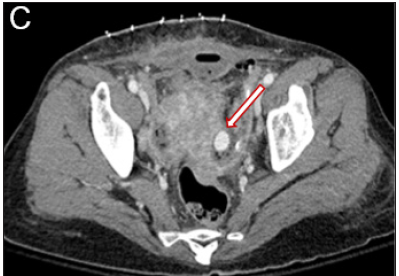
Figure 4: Selective left uterine arteriogram confirming the diagnosis.
Discussion
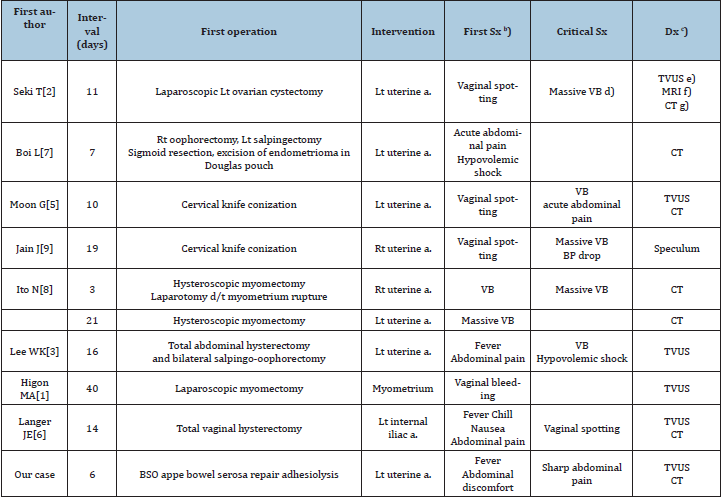
According to the medical literature, various clinical events and procedures responsible for the occurrence of UAPs have been reported. Most pseudoaneurysms occur in obstetric surgery, such as cesarean section, pregnancy-related events, including normal vaginal delivery, instrumental delivery and surgical abortion, and are rare in gynecological surgery, including abdominal, laparoscopic, and hysteroscopic myomectomy and abdominal hysterectomy, laparoscopic dissection of endometriotic lesions, uterine cervical conization, dilatation and curettage [2]. Since UAPs may occur in a procedure that is unlikely to be relevant, the characteristics were reviewed to prepare for similar situations in the future. We reviewed 10 cases of pseudoaneurysm after a gynecological operation (Table 1). First, although there are not many cases, we ranked them according to the first symptoms. Vaginal spotting or bleeding was most frequent, found in 6 of 10 cases, followed by abdominal pain, in 4 cases, and fever, in 3 cases.
Table 1: Review of the cases of pseudoaneurysm after gynecological operationa).
a) A PubMed search from 1991 to 2017 of the printed English using “pseudoaneurysm”, “uterine artery” and “Gynecology
operation” as keywords
b) Sx: Symptom
c) Dx: Diagnosis
d) VB: Vaginal bleeding
e) TVUS: Transvaginal bleeding
f) MRI: Magnetic resonance imaging
g) CT: Computed tomography
Most of the symptomatic course consists of vaginal spotting,
which occurs first and then changes to massive bleeding. Seki et
al. [2] described the case of a 35-year-old woman who had vaginal
spotting 5 days after laparoscopic left ovarian cystectomy for left
ovarian torsion [2]. At that time, TVUS showed a 1.5cm anechoic
space in the uterine cavity, but she was discharged because the
vaginal spotting stopped. At 11 days after surgery, the patient
presented at the hospital with massive vaginal bleeding. She was
examined imaging revealed a pseudoaneurysm. Additionally, Moon
et al. [5] described the case of a 32-year-old woman who had
vaginal spotting 1~2 days after conization for carcinoma in situ and
was observed [5]. At 10 days after conization, the patient presented
with sudden abdominal pain and hypovolemic shock. UAP was
identified from image. In some cases, the patient is suspected of
having a postoperative infection (abscess, urinary tract infection,
etc.) because of complaining of fever and abdominal pain. Langer et
al. [6] described the case of a 40-year-old woman who had fever and
abdominal pain 6 days after total vaginal hysterectomy for uterine
prolapse and urinary retention [6]. At that time, abdominal-pelvic
CT revealed a left-sided pelvic collection with low attenuation,
which was thought to be an abscess.
She was treated with intravenous antibiotics. At 14 days after
surgery, the fever had subsided, but mild lower abdominal guarding
and vaginal spotting were present. Follow-up color Doppler TVUS
revealed a pseudoaneurysm. According to these cases, if a BP drop,
massive vaginal bleeding, or severe abdominal pain occurs from the beginning in the emergency room, a pseudoaneurysm can be
diagnosed quickly with timely imaging and laboratory workups.
However, if there are only common postoperative symptoms,
such as vaginal spotting, abdominal discomfort, and mild fever, it
is difficult to suspect a pseudoaneurysm, and the imaging workup
may be considered an over-diagnosis. Therefore, patients should
be informed that they must visit the emergency room in the case
of such symptoms through warnings and education. Second,
although a definitive diagnosis of a UAP requires angiography,
the usefulness of several noninvasive diagnostic modalities,
including color Doppler ultrasound and CT angiography, has been
reported. CT angiography has some advantages over other imaging
modalities. CT angiography is not as operator-dependent and has
a shorter acquisition time. Although constructing 3D images may
be time consuming, it provides enough diagnostic information to
plan a treatment strategy, such as detection of the feeding artery
[2]. As shown in Table 1, TVUS and CT were not performed in
all cases. Lee et al. [3] reported that only TVUS was performed
because the patient presented with massive vaginal bleeding and
hypovolemic shock, and the UAP was identified by TVUS [3]. In our
case, transvaginal ultrasound imaging was not helpful because the
UAP was too small to identify. However, CT angiography detected
the UAP accurately. Boi et al. [7] reported that only contrastenhanced
CT was performed because the patient presented with
acute abdominal pain and hypovolemic shock, and the UAP was
identified by CT [7]. Additionally, Ito et al. [8] reported that only CT
was performed because of too much massive vaginal bleeding, and
UAP was identified [8]. Jain et al. [9] reported no imaging workup
because the patient presented with too much massive vaginal
bleeding and hypovolemic shock to undergo any imaging workup,
and only a speculum exam showed profuse bleeding from the cervix
[9]. Therefore, a combination of multiple diagnostic modalities is
important to make an early and precise diagnosis and not to miss
the diagnosis. However, if the patient is expected to become worse,
it is important to examine them by any of these modalities rather
than all of them and perform embolization as soon as possible.
Conclusion
Many of these patients come to the hospital complaining of only common postoperative symptoms, such as vaginal spotting, abdominal discomfort, and mild fever, before life-threatening symptoms appear. However, pseudoaneurysms should always be kept in mind. In addition, if a pseudoaneurysm is even slightly suspected, an imaging workup should be conducted in a timely manner to quickly achieve a diagnosis and treatment.
Conflict of Interest
The author(s) have no conflicts of interest relevant to this article.
References
- Higon MA, Domingo S, Bauset C, Martinez J, Pellicer A (2007) Hemorrhage after myomectomy resulting from pseudoaneurysm of the uterine artery. Fertil Steril 87(2): 417.e5-417.e8.
- Seki T, Hamada Y, Ichikawa T, Onota S, Nakata M, et al. (2017) Uterine artery pseudoaneurysm caused by a uterine manipulator. Gynecol Minim Invasive Ther 6(1): 25-27.
- Lee WK, Roche CJ, Duddalwar VA, Buckley AR, Morris DC (2001) Pseudoaneurysm of the uterine artery after abdominal hysterectomy: radiologic diagnosis and management. Am J Obstet Gynecol 185(5): 1269-1272.
- Berek JS, Novak E (2019) Berek & novak's gynecology. Lippincott Williams & Wilkins, Philadelphia, USA.
- Moon G, Jeon S, Nam KH, Choi S, Sunwoo J, et al. (2015) Pseudoaneurysm of uterine artery causing intra-abdominal and vaginal bleeding after cervical conization. Obstet Gynecol Sci 58(3): 256-259.
- Langer JE, Cope C (1999) Ultrasonographic diagnosis of uterine artery pseudoaneurysm after hysterectomy. J Ultrasound Med 18(10): 711-714.
- Boi L, Savastano S, Beghetto M, Acqua JD, Montenegro GM (2017) Embolization of iatrogenic uterine pseudoaneurysm. Gynecol Minim Invasive Ther 6(2): 85-88.
- Ito N, Natimatsu Y, Tsukada J, Sato A, Hasegawa I, et al. (2013) Two cases of postmyomectomy pseudoaneurysm treated by transarterial embolization. Cardiovasc Intervent Radiol 36(6): 1681-1685.
- Jain J, Leary SO, Sarosi M (2014) Uterine artery pseudoaneurysm after uterine cervical conization. Obstet Gynecol 123(2 Pt 2 Suppl 2): 456-458.
© 2019 Hye JD. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






