- Submissions

Full Text
Investigations in Gynecology Research & Womens Health
Reliability of Visual Diagnosis of Peritoneal Endometriosis
Hesham Abdel Fattah, Suzan Mohamed Farouk Helal, Tamer Ahmed Hosny* and Soad Mohamed Abbas Basuni
Department of Obstetrics and Gynecology, University of Alexandria, Egypt
*Corresponding author: Tamer Ahmed Hosny, Department of Obstetrics and Gynecology, University of Alexandria, Egypt, Email: dr_tamer_hosny@yahoo.com
Submission: November 15, 2017; Published: December 20, 2017

ISSN: 2577-2015Volume1 Issue4
Abstract
Endometriosis is a benign disease of the female genital system. It is characterized by endometrium-like tissue, consisting of glands and/or stroma, found outside the uterine cavity, the aim of this study to test the efficacy of laparoscopy in diagnoses of endometriosis, the present study was conducted on 69 patients (85 sample) complaining of pain and or infertility aged (14-48) year with exclusion of patient with pregnancy, pelvic malignancy and pelvic inflammatory disease.
Introduction
Endometriosis is described as a benign disease of the female genital system. It is principally characterized by endometriumlike tissue, consisting of glands and/or stroma, found outside the uterine cavity. Although implanted ectopically, this tissue presents histopathological and physiological responses that are similar to the responses of the endometrium [1]. The main symptom of endometriosis is pelvic pain, which is often very intense. Dysmenorrhea and other complaints like dyspareunia and infertility are also seen [2,3]. The diagnostic hypothesis of endometriosis is based on the clinical history, along with the results from gynecological examinations, laboratory tests and transvaginal ultrasound [4,5]. Some clinical characteristics, the physical examination itself, laboratory test results and evidence from imaging examinations may suggest the diagnosis [6]. The greatest difficulty lies in diagnosing minimal and mild lesions. In these cases, the ideal access for confirmation is always laparoscopic, since the complementary examinations available do not offer the necessary specificity [7]. Diagnosis by means of laparoscopy, which is considered the gold standard. However, the definitive diagnosis of the disease can only be obtained through histopathological examination of the biopsy sample [8]. Assessment of the accuracy of laparoscopy for diagnosing endometriosis has demonstrated that it is highly precise in ruling out the disease, thereby informing therapeutic decisions [9]. Studies have shown that endometriosis is principally diagnosed by laparoscopy combined with histopathological examination, although a negative result does not rule out the possibility of the disease [10]. The European Society of Human Reproduction and Embryology guidelines state that visual inspection of the pelvis is the criterion standard for diagnosis of endometriosis [11], and the most recent American Society for Reproductive Medicine (ASRM) guidelines state that "histologic evaluation is warranted whenever the diagnosis is not apparent on visual inspection at surgery" [12]. Although many specialists accepts that visual recognition of lesions alone is usually sufficient [13], the accuracy of visual diagnosis alone has yielded mixed results in numerous studies [14]. This is important because classification of the disease on the basis of rASRM stage mainly heavily on visual scoring [15].
Aim of the Work
The aim ofthe work is to correlate the diagnosis of endometriosis on the basis of visualization at laparoscopy with the hitopathologic diagnosis.
Subject
This study will include 69 patients (85 samples) with chronic pelvic pain or for infertility work up, who will be recruited from the Department of Obstetrics and Gynecology, EL-Shat by University Hospital, Alexandria University Hospital. The criteria for performing laparoscopy were as follows:
a) The subject aged (14 to 48years) and presenting pelvic pain and or infertility and the results from complementary tests such as CA125 determination and ultrasound.
b) Patients with pregnancy, pelvic malignancy and pelvic inflammatory disease were excluded.
c) During the laparoscopy we performed biopsies from lesions suggestive of endometriosis and histopathologically examined after fixation in 10% formalin and processed and embedded in paraffin blocks, sectioned, and stained with hematoxylin-eosin.
Results
Figure 1: Histogram of female age. Distribution was not- normal (D=0.133, p=0.004).
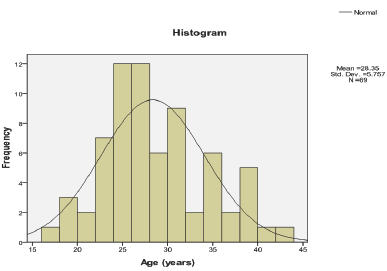
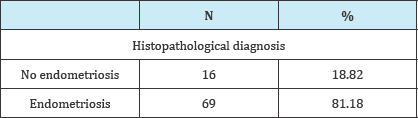
In the present study, female age ranged from 17 to 43 years with a mean of 28.35 ± 5.757 years (95% CI for mean: 26.96-29.76 years). Statistically the age was not normally distributed (D=0.133, p=0.004) so median (27.00) and IQR (25.00-32.00) is better to be used in description (Figure 1). Out of the 69 women, 12 had black colored lesions with median (IQR) age of 27.00(25.00-33.75) years, 20 had white colored lesions with median (IQR) age of 27.50 (25.00-30.00) years, 21 had red colored lesions with median (IQR) age of 27.00(24.50-32.50) years, and 16 had brown colored lesions with median (IQR) age of 27.50 (23.25-36.00) years. Statistically, there was no significant difference in median age among the four subgroups of patients (X2=0.350, p=0.950). In the present study, 40(57.97%) of patient had pain as a presenting complaints. Twenty four (34.78%) were fertile females, 18(26.09%) patients had primary infertility and 27(39.13%) patients had secondary infertility Out of the 85 samples taken in the present study, 14(16.47%) were biopsied from black endometriotic lesions, 28(32.94%) from white endometriotic lesions, 23(27.06%) from red endometriotic lesions, and 20(23.53%) from brown endometriotic lesions (Table 1). In the present study, glands was present in 47(55.3%) out of the 85 endometriotic specimens. Amount of glands were sparse in 29(34.12%) endometriotic specimens, moderate in 17(20.00%) and abundant in only 1(1.18%). In the present study, grade of stroma was present in 47(55.29%) out of the 85 endometriotic specimens. Grade of stroma were sparse in 31 (36.47%) endometriotic specimens, moderate in 15(17.65%) and abundant in only 1(1.18%). Stromal reaction was present in 35(41.18%) out of the 85 endometriotic specimens. Hemosidren deposit was present in 34(40%) out of the 85 endometriotic specimens. Hemosidren deposit was sparse in 21(24.71%) endometriotic specimens, moderate in 12(14.12%) and abundant in only 1(1.18%) Early Inflammatory infiltrate was present in 5(5.89%) out of the 85 endometriotic specimens. Early Inflammatory infiltrate was sparse in 4(4.71%) endometriotic specimens and moderate in only 1(1.18%) Late Inflammatory infiltrate was present in 35(41.18%) out of the 85 endometriotic specimens. Late Inflammatory infiltrate was sparse in 18(21.18%) endometriotic specimens, moderate in 14(16.47%), and extensive in 3(3.53%) Histopathological diagnosis revealed endometriosis in 69(81.18%) of the in endometriotic lesions biopsied (Table 2). In the present study, Laparoscopic diagnosis had 100% sensitivity (68 true positive), 80% positive predictive value, and 80% overall accuracy (p<0.001).
Table 1: Colour of the lesion.
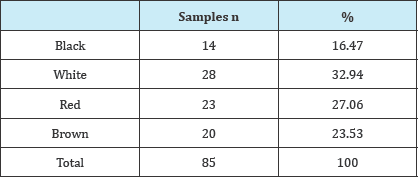
Table 2: Histopathological diagnosis.
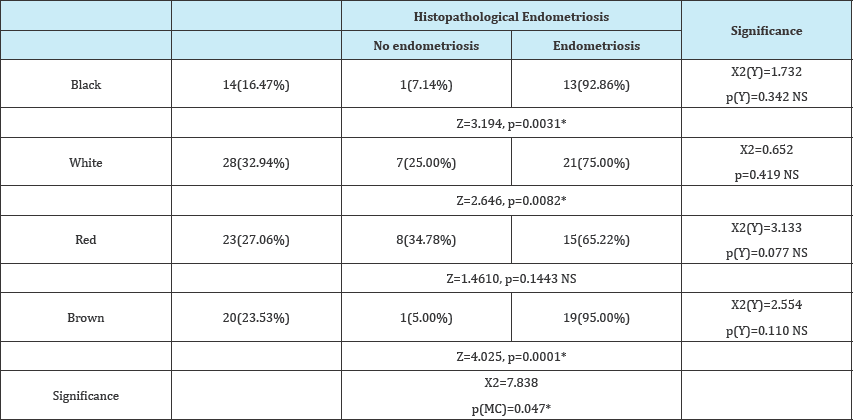
In the present study (Figure 2):
Figure 2: Pie chart of the color of pathological diagnosis of endometriotic lesions biopsied.

a. Regarding black color, there were 14(16.47%) samples with black color out of them 13(15.29%) histopathologically proved to be endometriosis and 1(1.18%) was histopathologically not endometriosis, occurrence of endometriosis in the black spot was statistically significant Z=3.194, p=0.0031.
b. Regarding white color, there were 28(32.94%) samples with white color out of them 21(75%) histopathologically proved to be endometriosis and 7(25.00%) was histopathologically not endometriosis, occurrence of endometriosis in the white spot was statistically significant Z=2.646, p=0.0082.
c. Regarding red color, there were 23(27.06%) samples with red color out of them 15(65.22%) histopathologically proved to be endometriosis and 8(34.78%) was histopathologically not endometriosis, occurrence of endometriosis in the red spot was statistically not significant Z=1.4610, p=0.1443.
d. Regarding brown color, there were 20(23.53%) samples with red color out of them 19 (95.00%) histopathologically proved to be endometriosis and 1(5.00%) was histopathologically not endometriosis, occurrence of endometriosis in the brown spot was statistically significant Z=4.025, p=0.0001.
Overall statistical test showed that There association between any color with endometriosis was significant X2=7.838, p(MC)=0.047 But there was no statistically significant that increase the probability of having positive histopathologically endometriosis among different color of peritoneal spots (Table 3).
Table 3: MC: Monte Carlo correction for p value of Pearson Chi square, (Y): Yate’s (continuity correction) for Pearson’s Chi-Square and p value.
Discussion
Early and accurate diagnosis of endometriosis may improve the quality of life of patients and provide cost-effective and long-lasting treatment [16]. Laparoscopy is the standard method for visually identifying the endometriotic lesions under magnification within and outside the minor pelvis, and for performing targeted biopsies for histologic corroboration [17,18].
The visual appearance of endometriosis is important because every intellectual and therapeutic process begins with a surgeon identifying disease. Inaccurate identification of disease can introduce selection bias at a first-order level and confound all conclusions, leading to inaccurate concepts of epidemiology, natural history, disease origin and treatment. The history of study of endometriosis is distinguished over the years by the recognition at surgery of progressively subtle manifestations of disease. Although awareness of the peritoneal and frequently subtle visual manifestations has increased irregularly among clinicians, application of this awareness toward greater understanding and better therapy has lagged. The numerical importance of atypical, subtle, non-hemorrhagic disease has recently been shown: at least two-thirds of patients have a visual appearance of disease that many clinicians have not been trained to recognize, while up to 40% have only such disease [19]. The aim of this study was to correlate the diagnosis of endometriosis on the basis of visualization at laparoscopy with the histologic diagnosis. The laparoscopic diagnosis of endometriosis as described in the literature varies widely because of the presence of a wide range of presumably characteristic lesions [17,18,20] . The promptness and accuracy of diagnosis is an important contribution to the application of early treatment and the prevention of scarring and adhesion and compromise of fertility [16] In the present study, laparoscopic was performed for 85suspected endometriosis patients, 69(81.18%) histopathologically confirmed to be endometriosis. This finding is in accordance with various published reports that have shown that the presence of endometriosis observed at laparoscopy or laparotomy could be confirmed histologically in the majority of cases [18,20,21]. Yet, the drawbacks of performing a laparoscopic diagnosis derive from the diversity of endometriotic appearances according to the site of the endometriotic lesion. For example, in a frozen pelvis, adhesions may completely cover endometriotic lesions [16]. In the present study, female age ranged from 17 to 43 years with a mean of 28.28 ± 5.869 years. Tumasian K et al. [22] examined women aged 25 to 36 years for treatment of endometriosis nearly in the same age group of the present study [22]. Pain was present in 50(58.82%) of the patients. Hsu AL et al. [23] reported that women with endometriosis had more menstrual pain (98.9%) and incapacitation due to menstrual pain (22.8%). Twenty patients (23.53%) of our sample had primary infertility and 31(36.47%) had secondary infertility. These findings are in agreement with Bulletti C et al. [24] who reported that endometriosis causes pain andinfertility, although 20-25% of patients are asymptomatic.
In the present study, black colored lesion was found in 14(16.47%), white in 28(32.94%), red in 23(27.06%) and brown in 20(23.53%). Mettler L et al. [16] emphasized that usually the laparoscopic diagnosis derives from the identification of the typical black or dark bluish or deep red spots on the peritoneal surface. But, one can easily miss the presence of endometriosis when a less marked discoloration is present. These "faint" lesions described by Jansen & Russel [25] include white opacification of the peritoneum, red flame-like lesions, yellowish patches, peritoneal defects, and adhesions. These lesions may be more common and possibly more active than the dark lesions [25,26]. Portuondo JA et al. [27] added that even when an exfoliative cytologic examination was applied in an attempt to widen diagnostic accuracy, it was shown to be of no value in the diagnosis, because in 46.5% of cases with positive histology the peritoneal aspirates failed to reveal the characteristics of endometriosis. Furthermore, our study demonstrates that even in the face of presumably certain endometriosis, as judged by the operators, histology failed to confirm endometriosis in 18.82% of the sites. Nevertheless, the overall diagnostic accuracy of the presence of endometriosis in the operated on patients was high, because in 69/85 patients (81.17%), histology confirmed the laparoscopic diagnosis of endometriosis. This finding was in agreement with Mettler L et al. [16] who reported that the accuracy in their study was 138/164 patients (84.1%). Redwine DB [28] recommended that a careful inspection of the peritoneum and laparoscopic magnification may help in the detection of minor lesions, but laparoscopic magnification may also contribute to the over diagnosis that we have observed in this study. Obviously, some endometriotic lesions are more easily recognized than others, especially the scarred blue/black, red, and brown lesions resulting from the accumulation over time of blood pigments, but a diversity of peritoneal lesions exists that may be mistaken for endometriotic lesions [16]. Among these are chronic inflammation, foreign body reaction (black punctations resulting from the reaction to previous sutures), electrocautery and laser carbonized burns, metastases of ovarian and breast cancer, epithelial inclusions, hemangiomas, and others [18,19,28].
Mettler L, et al. [16] also mentioned that another confounding factor for the laparoscopic diagnosis may be the frequent combination of endometriosis with smooth muscle or fibro fatty tissue observed in half of the patients, 82(50%), confirming previous observations [17] .In the present study, endometriosis was histologically determined mainly in brown 19/20(95.0%) and black 13/14(92.86%), to less extent in white 21/28(75.0%) and red 16/23(69.5%) lesions. These findings difference from those reported by Mettler L, et al. [16] who reported that in their study, endometriosis was histologically determined mainly in red and black lesions, but seldom in white lesions.
Conclusion
a) Laparoscopy can be used to diagnose endometriosis but it must to get better results to do histopathology to every suspected endometriotic lesion.
b) No significant difference between colors each other in relation to histopathology of endometriosis.
c) There's significant association between some colors (brown, black) in relation to suggestion of endometriosis.
Referencess
- Jansen RP, Russell P (1986) Nonpigmented endometriosis: clinical, laparoscopic, and pathologic definition. Am J Obstet Gynecol 155(6): 1154-1159.
- Olive DL, Henderson DY (1987) Endometriosis and mullerian anomalies. Obstet Gynecol 69(3 Pt 1): 412-415.
- Matorras R, Rodriguez F, Pijoan JI, Soto E, Perez C (1996) Are there any clinical signs and symptoms that are related to endometriosis in infertility women? Am J Obstet Gynecol 174(2): 620-623.
- Houston DE (1984) Evidence for the risk of pelvic endometriosis by age, race and socioeconomic status. Epidemiol Rev 6: 167-191.
- Redwine DB (1987) Age-related evolution in color appearance of endometriosis. Fertil Steril 48(6): 1062-1063.
- Abrao MS, Neme RM, Averbach M (2003) Endometriose de septo retovaginal: doenga de diagnostico e tratamento especfficos. Rectovaginal septum endometriosis: a disease with specific diagnosis and treatment. Arq Gastroenterol 40(3): 192-197.
- Tardif D, Poncelet C, Benifla JL, Madelenat P (1999) Exploration paraclinique des endometrioses. Paraclinical studies of endometriosis. Rev Prat 49(3): 263-8.
- Vercellini P, Trespidi L, De Giorgi O, Cortesi I, Parazzini F, et al. (1996) Endometriosis and pelvic pain: relation to disease stage and localization. Fertil Steril 65(2): 299-304.
- Wykes CB, Clark TJ, Khan KS (2004) Accuracy of laparoscopy in the diagnosis of endometriosis: a systematic quantitative review. BJOG 111(11): 1204-1212.
- Albert L Hsu, Izabella K, Pamela S (2010) Invasive and non-invasive methods for the diagnosis of endometriosis. Clin Obstet Gynecol 53(2): 413-419.
- Kennedy S, Bergqvist A, chaperon C, D'Hooghe T, Dunselman G, et al. (2005) ESHRE guideline for the diagnosis and treatment of endometriosis. Hum Reprod 20(10): 2698-2704.
- (2012) Practice Committee of the American Society for Reproductive Medicine. Endometriosis and infertility: a committee opinion. Fertil Steril 98(3): 591-598.
- Moses SH, Clark TJ (2004) Current practice for the laparoscopic diagnosis and treatment of endometriosis: a national questionnaire survey of consultant gynaologists in UK. BJOG 111(11): 1269-1272.
- Stratton P, winkel CA, Sinaii N, Merino MJ, Zimmer C, et al. (2002) Location, color, size, depth, and volume may predict endometriosis in lesions resected at surgery. Fertil Steril 78: 743-749.
- (1997) Revised American Society for Reproductive Medicine Classification of endometriosis 1996. Fertil Steril 67: 817-821.
- Mettler L, Schollmeyer T, Lehmann-Willenbrock E, Schuppler U, Schmutzler A, et al. (2003) Accuracy of laparoscopic diagnosis of endometriosis. JSLS 7(1): 15-18.
- Anaf V, Simon P, Fayt I, Noel J-C (2000) Smooth muscles are frequent components of endometriotic lesions. Hum Reprod 15(4): 767-771.
- Martin DC, Hubert GD, Vander Zwaag R, El-Zeky FA (1989) Laparoscopic appearances of peritoneal endometriosis. Fertility and sterility 51(1): 63-67.
- Redwine DB (1990) The visual appearance of endometriosis and its impact on our concepts of disease. Progress in clinical and biological research 323: 393.
- Nisolle M, Paindaveine B, Bourdon A, Berliere M, Casanas-Roux F, et al. (1990) Histologic study of peritonea endometriosis in infertile women. Fertility and sterility 53(6): 984-988.
- Vasquez G, Cornillie F, Brosens IA (1984) Peritoneal endometriosis: scanning electron microscopy and histology of minimal pelvic endometriotic lesions. Fertility and sterility 42(5): 696-703.
- Tumasian K, Bespoiasnaia V, Voronovskaia I (2001) Treatment of endometriosis in female infertility. Lik Sprava 3: 103-105.
- Hsu AL, Sinaii N, Segars J, Nieman LK, Stratton P, et al. (2011) Relating pelvic pain location to surgical findings of endometriosis. Obstetrics and gynecology 118(2 Pt 1): 223-230.
- Bulletti C, Coccia ME, Battistoni S, Borini A (2010) Endometriosis and infertility. J Assisted Reprod Genet 27(8): 441-447.
- Jansen RP, Russell P (1886) Nonpigmented endometriosis: clinical, laparoscopic, and pathologic definition. Am J Obstet Gynecol 155(6): 1154-1159.
- Vernon MW, Beard JS, Graves K, Wilson EA (1986) Classification of endometriotic implants by morphologic appearance and capacity to synthesize prostaglandin F. Fertil steril 46(5): 801-806.
- Portuondo JA, Herrán C, Echanojauregui AD, Riego AG (1982) Peritoneal flushing and biopsy in laparoscopically diagnosed endometriosis. Fertil steril 38(5): 538-541.
- Redwine DB (1987) The distribution of endometriosis in the pelvis by age groups and fertility. Fertil steril 47(1): 173-175.
© 2017 Hesham Abdel Fattah, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






