- Submissions

Full Text
Integrative Journal of Conference Proceedings
The Pouched Proboscis - Nasolabial Cyst
Anubha Bajaj*
Department of Pathology, India
*Corresponding author: Anubha Bajaj, Department of Pathology, India
Submission: November 29, 2021;Published: December 08, 2021

Volume2 Issue5December, 2021
Preface
Nasolabial cyst is an exceptional, non-odontogenic, developmental, maxillofacial cyst which arises between nasal vestibule and upper lip. The extra-osseous nasolabial cyst was initially scripted by Zuckerkandl in 1882. The soft tissue cyst is commonly discerned beneath alae nasi and is additionally designated as nasoalveolar cyst or Klestadt cyst. However, nasolabial cyst is confined to the soft tissue, in contrast to a nasoalveolar cyst which characteristically engenders a maxillary bone defect. The infrequently discerned nasolabial cyst can be misinterpreted and subjected to unsatisfactory therapy. Clinical discernment may be appropriate and adequate on account of characteristic location and clinical representation.
Disease Characteristics
Nasolabial cyst demonstrates an incidence of around 0.7% of cysts confined to maxillofacial region and roughly 2.5% of non-odontogenic cysts. An estimated 90% cysts are unilateral and around 10% cysts appear as bilateral lesions [1,2]. Nasolabial cyst demonstrates a female predominance with a female to male proportion of 3::4 :1. Commonly, nasolabial cyst implicates African women between fourth to fifth decade. Nevertheless, majority of instances are discerned within the fourth decade. Mean age of cyst emergence is 51 years [1,2]. Of uncertain pathogenesis, it is hypothesized that nasolabial cyst arises from epithelial remnants of anterior inferior segment of nasolacrimal duct [1,2]. Alternatively, it is posited to arise due to persistence of epithelial remnants emerging from nasolacrimal duct which extends between lateral nasal process and maxillary prominence [1,2]. It is postulated that nasolabial cyst originates from the embryonic epithelium which appears entrapped between developmental fissures arising from lateral nasal and maxillary processes [1,2]. Besides, nasolabial cyst may be engendered from epithelial cells confined within the mesenchyme following fusion of maxillary prominence with medial and lateral nasal processes during foetal life [1,2]. Therefore, the cyst is hypothesized to emerge from entrapped nasolacrimal duct tissue or it may arise as an embryonic fissural cyst [3,4]. Although a developmental cyst, the lesion commonly manifests in adulthood [3,4]. Pathognomonic, perpetual location of nasolabial cyst is within the submucosa of anterior nasal floor. Classically, the cyst is situated anterior to piriform aperture. On account of characteristic location, the cyst may evolve towards the nasolabial fold, mouth vestibule or the nasal vestibule [3,4].
Clinical Elucidation
Commonly, nasolabial cyst manifests an asymptomatic, gradually enlarging swelling associated with cosmetic disfigurement. Secondary infection of the cyst may ensue [3,4]. Although asymptomatic, the well circumscribed swelling can demonstrate partial or total nasal obstruction or localized pain [3,4]. Characteristically, a painless, gradually progressive lump appears adjacent to nasal alae. Cyst magnitude varies from 1 centimeter to 5 centimeter wherein enlarged lesions infrequently erode subjacent bone [5,6]. Typically, nasolabial cyst manifests as a painless, localized swelling. Concomitant nasal obstruction is common and variable wherein the obstruction is unaccompanied by nasal discharge or haemorrhage [5,6]. Nasal swelling may be minimally painful, gradually progressive, of variable magnitude and is associated with nasal obstruction [5,6]. Around one third to one half (30% to 50%) of nasolabial cysts may initially be infected. The infected cyst appears painful and may rupture spontaneously into the oral cavity or nasal cavity [5,6]. Upon examination, facial asymmetry is accompanied by a non-tender or mildly tender, fluctuant, mobile, non-discharging, subcutaneous, soft tissue swelling of the alar region [5,6]. Nasolabial cyst may obliterate the nasolabial fold, elevate ala or floor of the nose and obstruct intraoral component of labial vestibule along with the absence or presence of obstructed nasal cavity. Superimposed cutaneous surface appears unremarkable [5,6]. Nasolabial cyst may manifest as a fluctuant swelling within the maxillary labial fold or floor of nasal vestibule or appear adjacent to the nose along with the emergence of a tumescence within oral canine fossa and nasal floor [5,6]. Additionally, nasolabial cyst emerges as a well-defined, localized, fluctuant, cystic swelling confined to the nasolabial sulcus [5,6].
Histological Elucidation
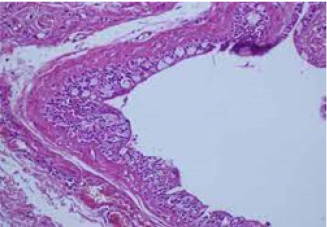
Upon gross examination, nasolabial cyst delineates a spherical, smooth, extra-osseous lesion with a pinkish or bluish countenance Figures 1 & 2. Cyst magnitude varies from 1 centimeter to 5 centimeters. The cyst adheres firmly to muco-cutaneous junction of the nasal cavity and is usually non adherent to subjacent bone [7,8] Figures 3 & 4. Upon microscopy, the cyst is layered by respiratory epithelium denominated by ciliated cylindrical or non-ciliated cylindrical, stratified or pseudostratified columnar or cuboidal epithelium imbued with numerous mucin-producing goblet cells [7,8] Figures 5 & 6. Circumscribing soft tissue stroma is loose, oedematous and infiltrated by chronic inflammatory cells as lymphocytes and macrophages. Infected cysts may display foci of squamous metaplasia [7,8] Figure 7.
Figure 1: Nasolabial cyst layered with a stratified and pseudo-stratified ciliated columnar epithelium with an encompassing inflamed fibrous tissue stroma.
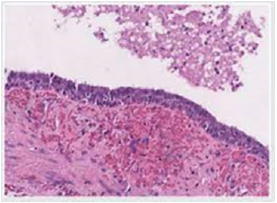
Figure 2: Nasolabial cyst exhibiting a layer of stratified ciliated columnar epithelium with a circumscribing, mildly inflamed fibrous tissue stroma.
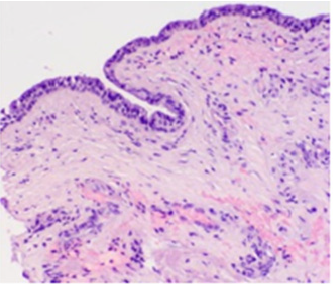
Figure 3: Nasolabial cyst exemplifying a layer of stratified ciliated cuboidal epithelium with a subjacent, mildly inflamed fibrous tissue stroma.

Figure 4: Nasolabial cyst enunciating foci of stratified squamous epithelium lining the cystic cavity and enveloping, mildly inflamed fibrous tissue stroma.
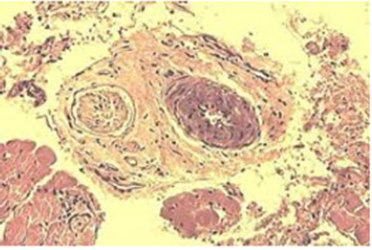
Figure 5: Nasolabial cyst demonstrating a cystic cavity lined with stratified, ciliated columnar epithelium with encompassing inflamed fibrotic stroma.

Figure 6: Nasolabial cyst delineating a layer of stratified and pseudostratified ciliated columnar epithelium enmeshed within an inflamed fibrotic stroma.
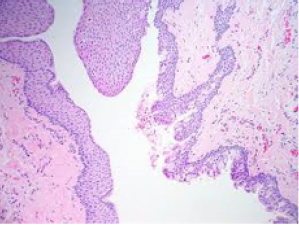
Figure 7: Nasolabial cyst lined with stratified columnar epithelium admixed with mucin producing goblet cells and a subjacent inflamed, fibrotic stroma.
Differential Diagnosis
The extra-osseous nasolabial cyst requires a segregation from
odontogenic lesions, developmental cysts and neoplastic lesions
such as
A. Odontogenic cyst which emerges as a periapical
inflammatory lesion and may manifest an epithelioid cell
granuloma, cyst or an abscess. The adjacent bony cortex may be
attenuated. Adjacent teeth are non-vital and appear radiolucent.
Teeth may be engendered from bud-like invaginations of
primitive ectodermal epithelial layer of the oral cavity. The
specialized epithelium or Hertwig epithelial root sheath
configures the root followed by degeneration into epithelial
rests of Malassez. Residual, bud-like invaginations of dental
lamina appear to induce epithelial rests of Serres delineated
within gingival soft tissues. Epithelial rests of Malassez manifest
as miniature spherules of six to eight epithelial cells with
enhanced nucleus to cytoplasmic ratio and minimal reverse
cellular polarity [7,8].
B. Dentigerous cyst represents a well demarcated,
radiolucent lesion which adheres at an acute angle to cervical
region of an un-erupted tooth. The cyst is layered by fibrous
or fibromyxoid connective tissue. Rete ridges are absent and
dermal-epidermal interface is flattened. The layering cuboidal
epithelium is two to four cell thick and devoid of superficial
keratinization. Occasional mucous cells, ciliated cells and
focal dystrophic calcification may be discerned. Odontogenic
epithelial rests are miniature and inactive [7,8].
C. Dento-alveolar abscess commonly manifests with nonvital
incriminated teeth. The abscess is encompassed with
dense fibrous tissue or granulation tissue which appears
infiltrated with an inflammatory exudate composed of
lymphocytes, neutrophils, plasma cells, histiocytes, mast cells
and eosinophils. Occasional, eosinophilic hyaline bodies appear
disseminated within corrugated, condensed peripheral collagen
with a smattering of lymphocytes and multinucleated giant
cells. Spicules of remodelled bone or dystrophic calcification
may be observed. Epithelial rests of Malassez may be identified
within the granulation tissue [7,8]. Cholesterol clefts appear
commingled with multinucleated giant cells, erythrocytes and
focal hemosiderin pigment deposits [7,8].
D. Nasopalatine duct cyst is layered by stratified squamous
epithelium, simple columnar epithelium, simple cuboidal
epithelium or variably ciliated, pseudostratified columnar
epithelium admixed with mucin- producing goblet cells. Cyst
wall is comprised of fibrous tissue commingled with a neural
component, cartilaginous rests, arteries and veins. Upon
Magnetic Resonance Imaging (MRI), the nasopalatine duct cyst
exemplifies an intraosseous lesion [7,8].
E. Epidermal inclusion cyst is commonly discerned in a subepidermal
location and the cyst may or may not be contiguous
with superimposed epidermis. The cyst is layered with stratified
squamous epithelium demonstrating a distinctive granular cell
layer. Cyst wall is devoid of eccrine glands, sebaceous glands or
hair follicles and the cyst cavity is imbued with abundant keratin
flakes. Foreign body giant cell reaction may be engendered
with cyst rupture. The cyst exhibits an identical radiographic countenance as nasolabial cyst. Besides, epidermoid and
dermoid cysts are characteristically discerned in childhood
and exhibit a yellowish discoloration of encompassing mucosa
[7,8]. Besides, nasolabial cyst requires a segregation from
odontogenic lesions such as canine space abscess, follicular
cyst, periodontal cyst and residual cysts along with benign and
malignant salivary gland neoplasms [7,8]. Additionally, lesions
such as sebaceous cyst, oro-nasal cyst or non-odontogenic
maxillary cyst require exclusion [7,8]. Infected nasolabial
cyst requires a demarcation from acute maxillary sinusitis,
periodontal abscess, furuncle of nasal vestibule floor or facial
cellulitis [7,8].
Investigative Assay
Digital palpation depicts a fluctuant swelling between floor of nasal vestibule and gingivolabial sulcus [9,10]. Endoscopic examination of the nasal cavity exhibits a mass which may occlude the nasal aperture [9,10]. Ultrasonography can be beneficially emp006Coyed as a manoeuver to appropriately discern nasolabial cyst [9,10]. Upon plain radiography, a cyst is discerned within the nasolabial region which appears segregated from adjoining bony anatomical structures and teeth. Nevertheless, alterations of abutting bone or teeth are absent. Significant erosion of maxillary bone may be discerned upon plain radiographs [9,10]. Computerized Tomography (CT) and Magnetic Resonance Imaging (MRI) can be adopted to affirm the presence and expanse of the cystic lesion, concordance with nasal alae and incrimination of maxillary bone [9,10]. Computerized Tomography (CT) and Magnetic Resonance Imaging (MRI) are advantageous in assessing the site and methodology of cyst origin and circumventing unnecessary procedures as needle aspiration or dental surgery [9,10]. Computerized Tomography (CT) is a cost effective, preferred preoperative investigative technique employed for assessing the lesion border. CT demonstrates a well demarcated, spherical, homogeneous soft tissue lesion of minimal density situated within the nasolabial region [9,10]. A space occupying, iso-dense or hypodense lesion may be discerned within the nasal alar region. Scalloping due to mass effect and bone remodelling may be observed although lesion enhancement or bone destruction is absent [9,10]. Upon Magnetic Resonance Imaging (MRI), the cyst demonstrates a hypo-intense signal intensity upon T1 weighted imaging and hyper-intense signal intensity upon T2 weighted imaging with characteristic features of fluid retention [9,10].
Therapeutic Options
Therapeutic intervention is indicated with the occurrence of cosmetic deformity, nasal obstruction or infection within the nasolabial cyst [9,10]. Spontaneous rupture of the cyst may occur. Also, nasolabial cyst can be evacuated through the oral route, nasal route or via a cutaneous fistula [9,10]. Cogent treatment strategies are comprised of injectable sclerotic substances, marsupialization or surgical eradication of the cyst. Surgical resection of the cyst is diagnostic and curative as a concomitant histological assessment is possible [9,10]. Surgical extermination is necessitated in order to confirm the morphological diagnosis, circumvent cyst infection, cyst reoccurrence and ameliorate cosmetic disfigurement [9,10]. Optimally adopted surgical manoeuvers as incision and drainage, injectable sclerotic agents or simple aspiration and cauterization of cyst may be associated with an enhanced proportionate cyst reoccurrence, a feature which may be circumvented by the employment of endoscopic marsupialization and comprehensive surgical cyst resection [9,10]. Nevertheless, in contrast to intraosseous cysts, marsupialization remains a rather ineffective procedure for treating the extra-osseous nasolabial cyst [9,10]. The optimal, preferred treatment strategy is comprehensive surgical extermination through a sub-labial incision [9,10]. Postoperatively, mild facial oedema and numbness upon the lower face may ensue. Perforation of nasal mucosa may occur during surgical extermination of the lesion [9,10]. Comprehensive surgical eradication is devoid of cyst reoccurrence. Malignant transformation is exceptional [9,10].
References
- Almutairi A, Alaglan A, Alenezi M, Alanazy S, Al-Wutayd O, et al. (2020) Nasolabial cyst: Case report and review of management options. BMC Surg 20(1): 10.
- Kajla P, Lata J, Agrawal R (2014) Nasolabial cyst: Review of literature and a case report. J Maxillofac Oral Surg 13(2): 227-230.
- Zografos I, Podaropoulos L, Malliou E, Tosios KI (2018) Nasolabial cyst: A case report. Oral Surgery 12(1): 51-56.
- Smith TL (2019) Scientific abstracts for RhinoWorld 2019. Int Forum Allergy Rhinol 9(S2): S49-S124.
- Dghoughi S (2017) Bilateral nasolabial cyst. J Stomatol Oral Maxillofac Surg 118(6): 385-388.
- Righini CA, Baguant A, Atallah I (2017) A nasolabial swelling. Eur Ann Otorhinolaryngol Head Neck Dis 134(2): 137-138.
- Ocak A, Duman SB, Bayrakdar IS, Cakur B (2017) Nasolabial cyst: A case report with ultrasonography and magnetic resonance imaging findings. Case Rep Dent 2017: 1-4.
- Sato M, Morita K, Kabasawa Y, Harada H (2016) Bilateral nasolabial cysts: A case report. J Med Case Rep 10(1): 246.
- Yeh CH, Ko JY, Wang CP (2017) Transcutaneous ultrasonography for diagnosis of nasolabial cyst. J Craniofac Surg 28: e221-e222.
- Sheikh AB, Chin OY, Fang CH, Liu JK, Baredes S, et al. (2016) Nasolabial cysts: A systematic review of 311 cases. Laryngoscope 126(1): 60-66.
© 2021 Anubha Bajaj. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






